What is More Accurate for Diagnosing Early Stages of Hair Loss : A Scalp Biopsy or Clinical (Trichoscopic) Examination?
Biopsy or Up Close (Trichoscopic) Examination: What’s better for diagnosing the early stages of hair loss?
I’ve selected this question below for this week’s question of the week. It allows us to the review some key concepts in diagnosing hair loss via clinical scalp examination and through a biopsy.
QUESTION
What is more accurate - a scalp biopsy or a scalp exam with a dermatoscope? My biopsy results said telogen effluvium and androgenic alopecia with the diagnosis of androgenetic alopecia being favored.
As for me, I’m a 30 year old female. My scalp is itchy, likely from seborrheic dermatitis which was diagnosed by a dermatologist. I’ve suffered from alopecia areata in the past (1 small bald patch at a time and treated with cortisone injections) . I have a lot of food and environmental allergies that I’m treating naturally. My hair started shedding excessively at the end of February 2021 after a very traumatic event in December 2020. I’m not on any prescription medications but I do take supplements (iron, vitamin D and C, coQ10, quercetin, probiotic, l-lysine, caprylic acid, and a multivitamin for hair). The shedding has been diffuse and I have lost density. My family members insist that no one would know I’m having issues with my hair. In the past few weeks I have had days with minimal shedding. I have been treating the seborrheic dermatitis with medicated shampoos. I have been treating the hair loss naturally, through dietary changes, lowering stress levels with meditation, etc; I have not used any medications.
The dermatologist that performed the biopsy said it’s “age related” (I’m a 30 year old female) and therefore not even considered an early stage AGA. The second dermatologist I saw (for a second opinion) did a scalp exam with a dermatoscope and said there was “maybe one” miniaturized follicle at the biopsy site on my crown. Throughout the rest of the top of my scalp she said about 1 in 100 follicles are miniaturized. She gave me a diagnosis of just telogen effluvium. So far all of my test results (iron, ferritin, vitamin D, vitamin B12, thyroid panel, and hormone panel) have been normal. I’m very confused and not sure if and what treatment would be best for me. Thank you!
ANSWER
Thank you for the question. In order for me to advise you on what treatment would be best for you, we need a diagnosis.
So what is your diagnosis then?
Well, in order for me to give you a diagnosis, I would need to know a bit more about your story from birth until today, and see your scalp up close myself and review your blood tests. Those are the three key steps in order to make a diagnosis for anyone!. Because I don’t have any of these pieces of information in your case, I can’t actually say what your diagnosis is.
However, there are still some very important points to be aware of and that’s why I’ve selected your question for this week’s question. It’s such a good one with so many things for us to review.
So let’s get to it.
You have what I call early hair loss. You yourself know there is a change, but your friends and family think everything is just fine. Even one of the dermatologists thinks it’s simply a telogen effluvium. This is early hair loss.
As you have correctly outlined, this can often be due to androgenetic alopecia or telogen effluvium …. or both.
As I review all your information about what your biopsy showed and what your doctors actually said, I need to know how reliable each of these three pieces of information are. If dermatologist 2 is a world expert in hair loss and doesn’t think its AGA - does this carry more “influence” as I think about your case than if dermatologist 1 thinks it’s AGA but really has only seen a handful of hair loss patients in his or her career?
Yes it most certainly does.
Your question is really all about the reliability of these three pieces of information - the 2 doctors and the 1 biopsy.
And what if the biopsy was taken from an area on the scalp that is really not so useful for making a diagnosis (like the temples) - am I to trust this result? Well, no.
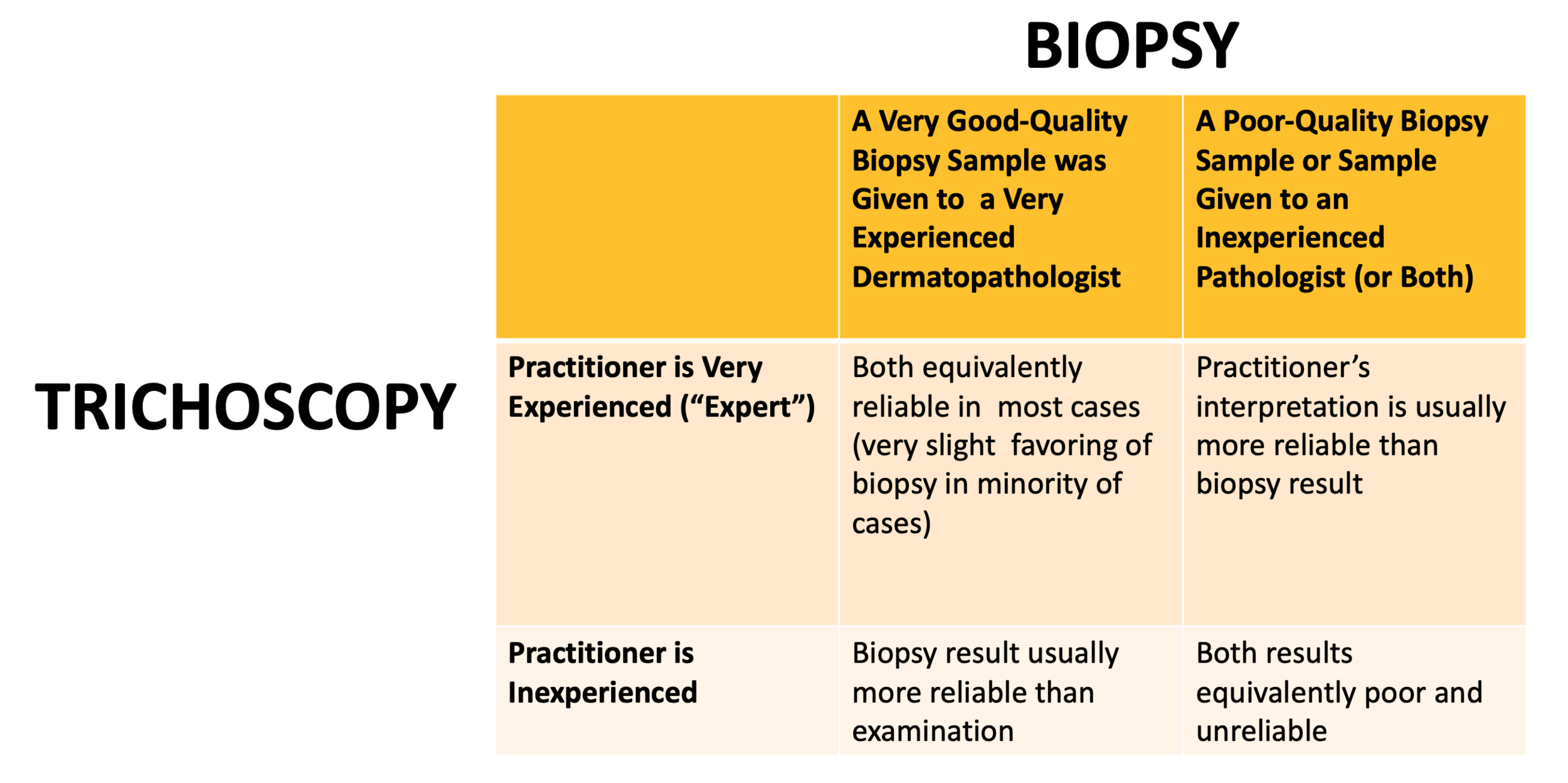
So, let’s take a look at these four scenarios below in order for us to better understand when a biopsy is better than a clinician’s interpretation and when a clinician’s interpretation is to be trusted more than a biopsy report.
In general, the very early stages of hair loss can be challenging to decipher from one another. The more experience and expertise the clinician has in treating hair loss … the more reliable his or her view will be on the cause of hair loss. The less experience the clinician has, the less reliable his or her view is and the more a biopsy result is to be trusted. However, biopsies are not all the same. The only biopsy result that I really trust is one taken from the correct area of the scalp and interpreted properly by expert dermatopatholgist.
Let’s take a look at the following chart and then we’ll break it down some more.
SCENARIO 1. The practitioner evaluating the scalp is a VERY EXPERIENCED hair loss expert and a 4 mm punch biopsy was taken from a correct area of the scalp and interpretations were done by a VERY EXPERIENCED dermatopathologist.
In this case, both the dermatologist’s opinion and the dermatopathologist’s opinion are fairly reliable. In fact, in most cases, they are fairly equivalent. A highly experienced clinician can examine all areas of the scalp and can determine just how much variation in the caliber of hair follicles (ie “miniaturization”) is seen in the various regions including the front, middle, top and back. If the clinician appreciates that density is slightly different in one area compared to another it’s like their is some androgenetic alopecia going on - especially if the thinner area show a greater degree of miniaturization.
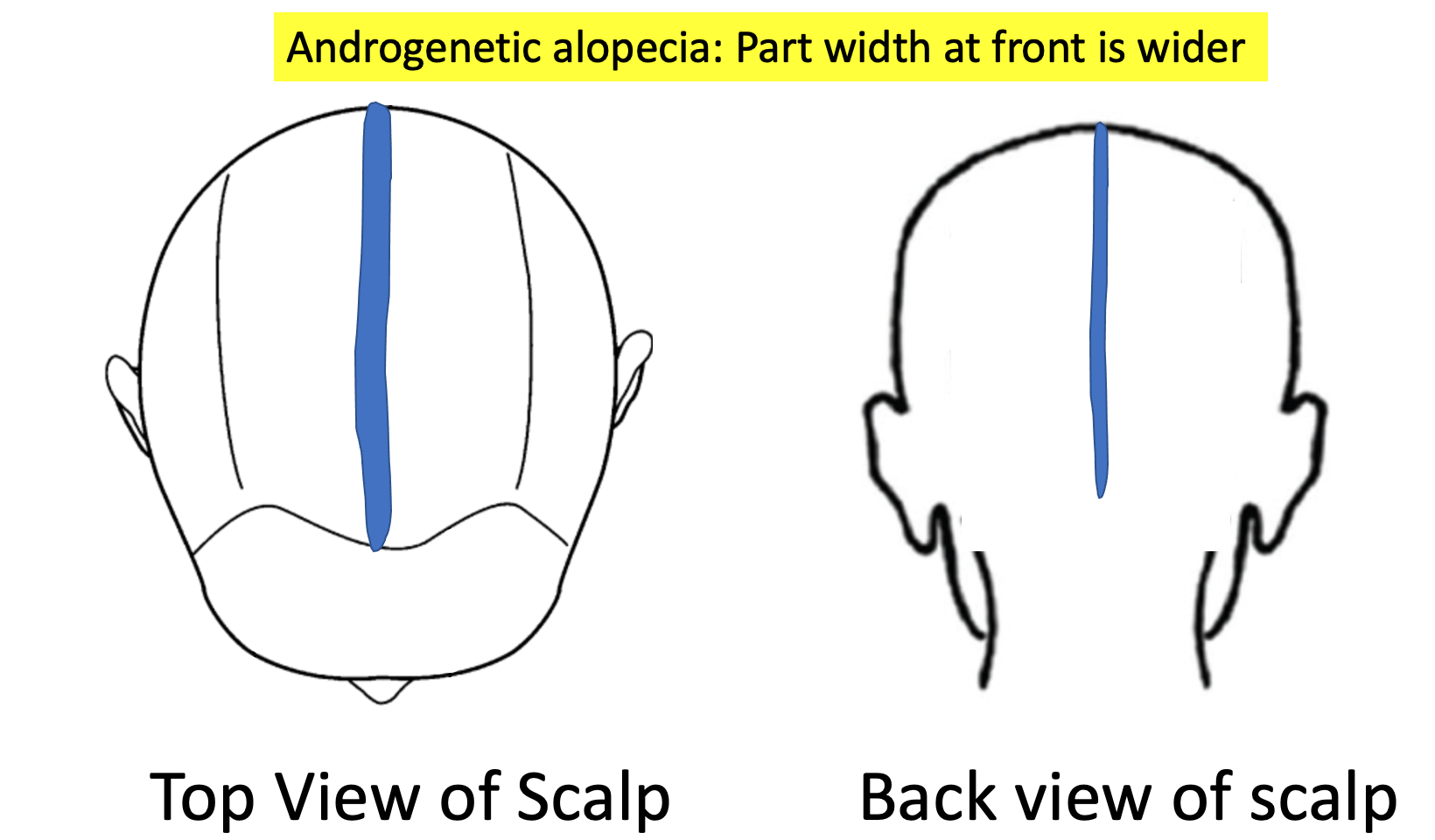
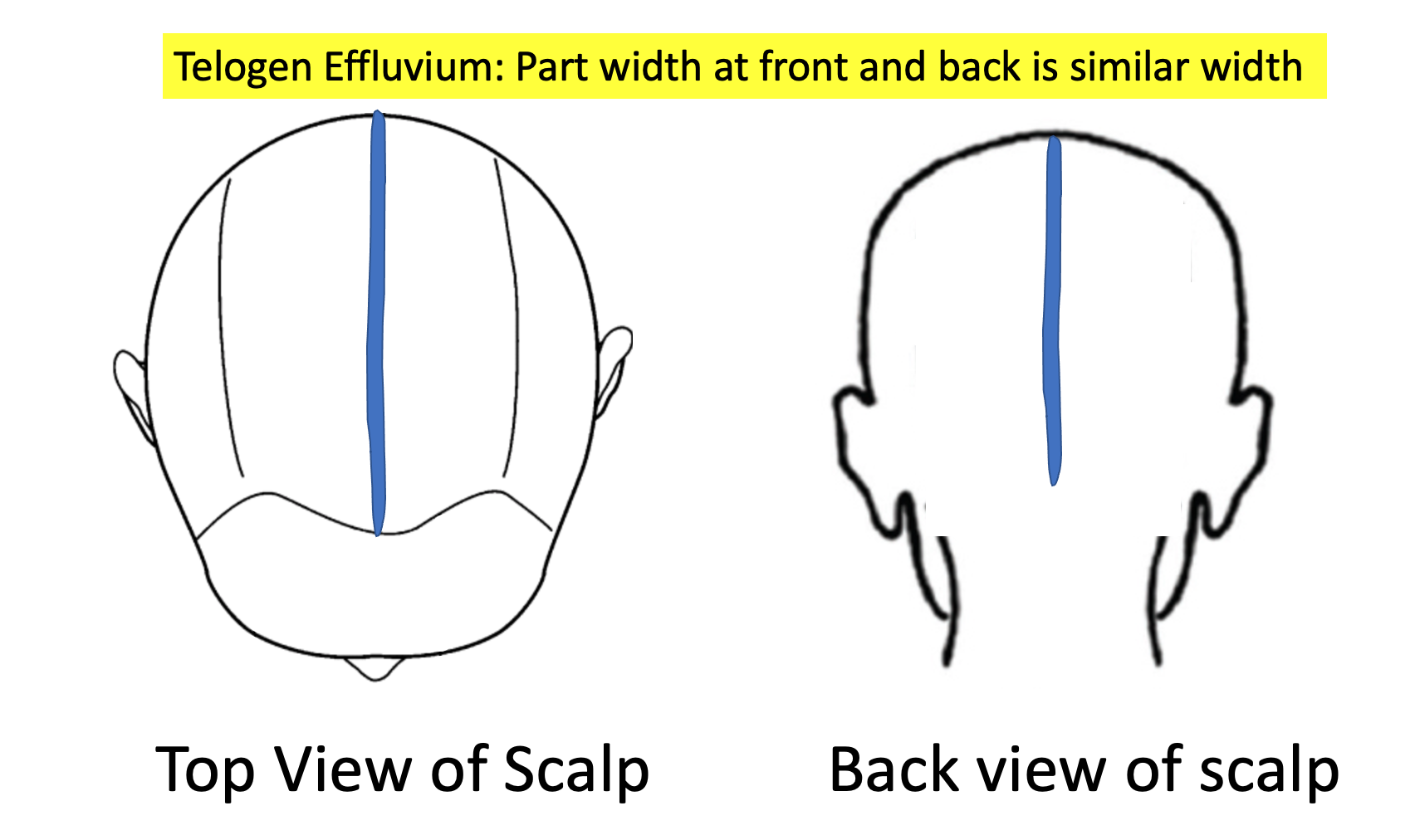
A clinician can also evaluate density in the frontal area and compare this to the back. If there is a subtle increase in “part width” in the frontal and mid scalp compared to the back, this gives a suggestion there could be some androgenetic alopecia going on.
So an astute clinician can look at the scalp, look at the part width, look a the density in various regions of the scalp and look at what the trichsocopy shows and come up with a conclusion.
Clinical examinations of the early stages of hair loss are tricky to interpret. It takes expertise to appreciate subtle changes in hair follicle caliber. It’s not something that is learned overnight. It’s not a result that pops up on any sort of screen when one places a dermatoscope one the scalp. Of course, it one’s dermatoscope its connected to a computer and the caliber of follicles can actually be measured in various areas, this really increases the reliability of the interpretation for less experienced practitioners.
But if a practitioner is less experienced with hair and scalp issues, simply placing a dermatoscope on the scalp and concluding “I don’t see any miniaturization” does not give me a great amount of confidence in diagnosing early hair loss issues.
What about a biopsy? Biopsies in early hair loss can be wonderful! A biopsy taken from the area of androgenetic alopecia can also show a DECREASING terminal to vellus ratio from a normal low 7:1 or 8:1 down to 4:1 or less. In true telogen effluvium, the terminal to vellus ratio stays well above 6 or 7 to 1. An experienced dermatopathologist who interprets a biopsy from a patient with early hair loss and says ‘the T:V ratio is 3.5:1 and sebaceous glands appear enlarged and there is no real shift in catagen to telogen ratios and there is no peribular inflammation” is telling me this is likely androgenetic alopecia. I trust that report if I know the dermatopathologist is experienced.
To summarize, a very experienced practitioner can often make a diagnosis of androgenetic alopecia fairly reliably even without a scalp biopsy. However, if a scalp biopsy is done, the results should be similar trusted as the findings of a very experienced practitioner provided the biopsy is interpreted by an expert pathologist.
SCENARIO 2. The practitioner evaluating the scalp is an INEXPERIENCED practitioner and a 4 mm punch biopsy was taken from a correct area of the scalp and interpretations were done by a VERY EXPERIENCED dermatopathologist.
In this case, the biopsy report is MORE reliable than the view of the clinician. We need to remember here that early hair loss stages are really difficult to diagnose! There is no harm in saying that and I’ll be the first to point that out.
It can take anywhere from 6 months to 5 years from the time some types of hair loss first start before a patient themselves figure out that something is changing on their scalp. So, the early stages of hair loss are tricky to spot. The early stages of hair loss can sometimes look normal. The less experience the practitioner has …. the more the scalp will look normal to them ! That’s just a fact. Any practitioner who takes a quick 5-10 second glance at the scalp and says to their patient ‘your scalp looks fine to me… don't worry” is by definition an inexperienced practitioner. This is pretty much a rule. The early stages of hair loss are hard to spot sometimes and take a bit of poking and prodding in the scalp to see what all the 100,000 hairs are doing and a bit of sleuthing to gather information from the patient as to exactly what’s been happening over the past months.
If a very experienced clinician says ‘This scalp is normal” then it’s pretty unlikely there is any androgenetic alopecia. Not 100% guarantee of course….. but pretty unlikely. If an inexperienced clinician says ‘This scalp is normal” then it carries less meaning. Of course, it could be normal, but I’m a bit more skeptical. I am sent referrals every day of the year that say “ Normal scalp exam. Patient thinks they have hair loss. Please see in consultation.”
What do many of these patients end up having as a diagnosis ? Well, many have androgenetic alopecia !
Suppose I’m meeting up with a friend for dinner and I tell my friend that I have been getting some pretty bad headaches lately. If my friend tells me everything sounds fine, do I believe it? Well, if my friend is a neurologist I’m a bit more likely to trust this information than if my friend is an accountant. The quality of the information makes a difference.
So to summarize, if a clinician is less experienced with diagnosing hair loss but takes a biopsy from a correct area of the scalp (ie where the hair loss is most affected) and the biopsy lands in the hands of an expert dermatopatholgist …. then I would usually trust the dermatopathoglist report over the clinician’s interpretation of what’s causing the early hair loss.
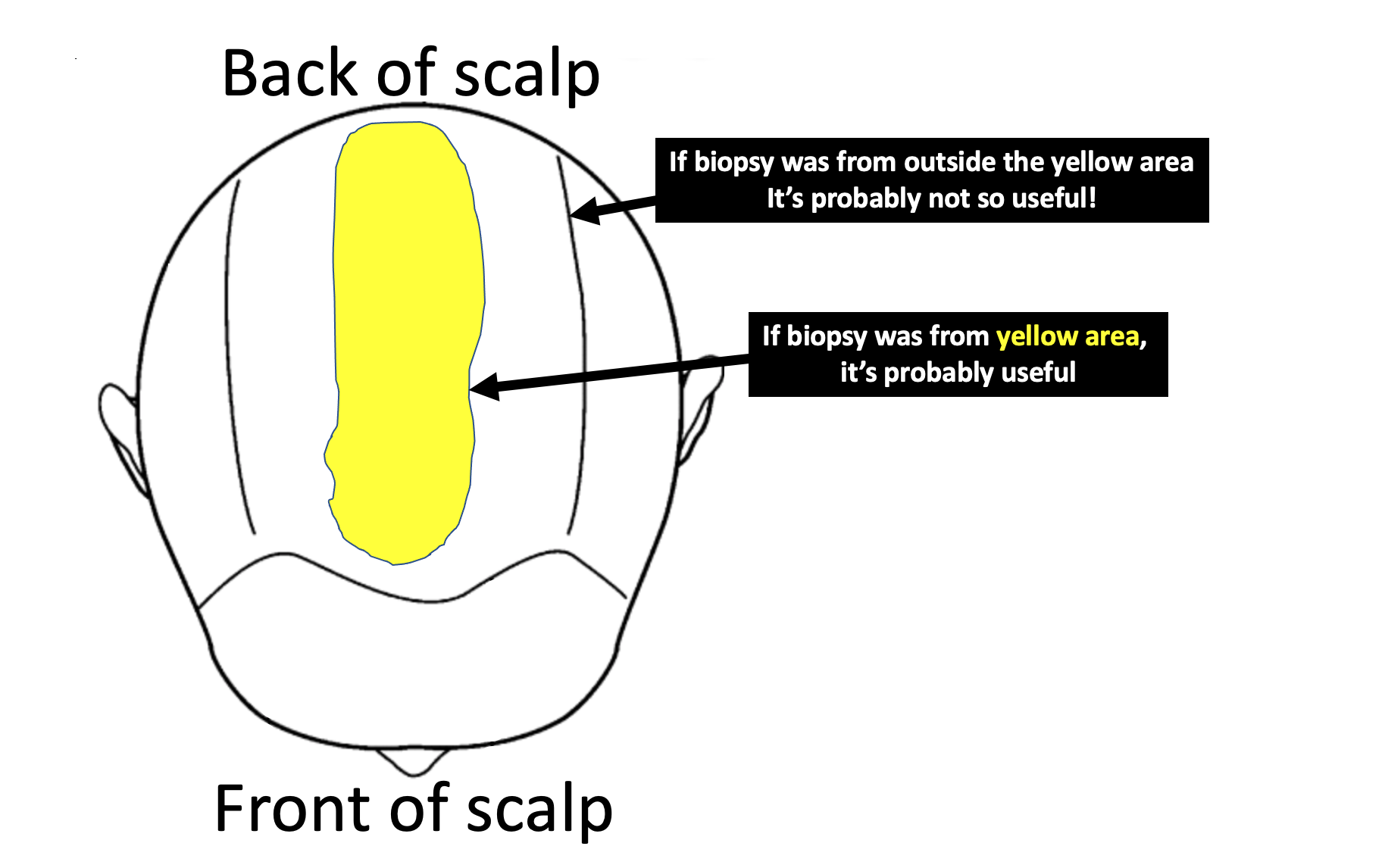
So what’s a good biopsy in your case? Well, in your case this likely means that biopsy was taken from somewhere in the yellow area shown below. I would prefer if the biopsy was 4 mm in size. I would also like if the biopsy was processed with horizontal sections as personally that increases my confidence in these early stages of hair loss. It’s only with horizontal sections that the pathologist can give a measurement of the terminal to vellus ratio. This can’t be done with vertical sections. If your T:V ratio is less than 4:1, we might begin to think there is some androgenetic alopecia present as a diagnosis.
SCENARIO 3. The practitioner evaluating the scalp is an EXPERIENCED hair loss expert and a suboptimal biopsy was taken from an incorrect area of the scalp and/or interpretations were done by an INEXPERIENCED pathologist.
This would be an unusual situation whereby an experienced clinician took a biopsy from a wrong spot. But this situation could be an experienced clinician is trying to decide what diagnosis a patient has and the patient brings in a biopsy report they had at another clinic showing a certain result.
In this case, I trust the result from the clinician any day over the biopsy report. Every day, I see biopsy reports that are taken form the back of the scalp or the sides of the scalp or the temples. These are not the ideal areas to be taking biopsies from if we want determine whether or not the patient has androgenetic alopecia!!!
Sometimes, the doctor does not want to cause a scar…. and so takes it from the sides of the scalp so as to hide any scar. Sometimes, a patient asks the doctor to take it from the temples because that’s where they are most worried and where they see the changes every day of their life when they look in the mirror. These are not where we should be taking biopsies to confidently assess androgenetic alopecia !
If a biopsy returns showing “no evidence of androgenetic alopecia” but was taken from the sides fo the scalp does it mean the patient does not have androgenetic alopecia? No! Not at all,. That biopsy was not helping in making the proper diagnosis.
If a biopsy returns showing “no evidence of androgenetic alopecia” but was taken from the main area of hair loss in the central scalp zone, does it mean the patient does not have androgenetic alopecia? Probably that is the correct interpretation.
SCENARIO 4. The practitioner evaluating the scalp is an INEXPERIENCED practitioner and a suboptimal biopsy was taken from an incorrect area of the scalp and interpretations were done by an INEXPERIENCED pathologist.
A particularly challenging situation is when a less experienced practitioner is not sure what the diagnosis is but proceed to take the biopsy from an area of the scalp which is less than ideal. Typically this is a well meaning practitioner who wishes to take the biopsy from an area that will best be hidden in the future should the area form a small scar. So the biopsy is taken from the sides of back of thee scalp and typically returns showing no evidence of androgenetic alopecia. The only thing that can be interpreted in this situation is that the patient does not have androgenetic alopecia down the sides of their scalp. However, we can’t conclude anything at all about what might be happening in the middle of the scalp - the area where the patient is most concerned about the hair!
I often use the following analogy when I explain the concept to doctors that I teach.
Suppose you have a mold of some kind in your home. The house smells like mold! Terrible, right?
And so you call a mold specialist for help. Unfortunately, all the mold specialists in town are away at a convention so you decide to call a plumber. After all, mold grows in water and damp conditions, and you figure that a plumber knows a lot about water and damp conditions in homes.
The plumber answers the call and says he or she knows how to take mold samples because they learned how to do so in a course they took.
Voila!
You are happy with the answer and invite the plumber to your home to get some help.
The plumber finds a bit of water in the basement and takes some mold samples. It all comes back negative.
You are all relieved there is no mold!
The problem is that the smell continues.
When the mold specialist in town returns from the convention, you invite him or her now into your home. Within a few minutes the source of the mold is located in the attic of the house. Their is a leak in the roof and this is causing the roof to leak and the attic to grow mold !!!! Samples are taken and the mold is finally proven.
Did it matter where the samples were taken? You bet it did!
An experienced specialist is more likely to know where to take the sample .
Conclusion
Your question is really a great one. Thanks again for submitting. It’s difficult, if not impossible for patients to know if their biopsy was taken from the correct spot or whether their clinician really has a lot of experience or not. It’s tough to navigate the medical world sometimes.
The short answer to your question , however, is that a very experienced clinician can often diagnose hair loss with a similar degree of accuracy to a biopsy interpreted by an expert dermatopathlogist. If the skills of the clinician change or the skills of the dermatopathologist now change, this no longer holds true and you’ll need to see the chart about as to which is better.
It is quite likely with your story that at least one of your diagnoses was telogen effluvium that was triggered by the stress of December 2020. With your story, I think it’s really important that someone make sure that your seborrheic dermatitis is under good control and someone keep an eye on the possibility that a diffuse alopecia areata is not part of the reason for your shedding. I think that would be unlikely given that shedding has settled now and that the biopsy did not capture this.
With this one biopsy that you do have I can’t exclude that there is not some degree of androgenetic alopecia present. There certainly is a possibility with this information you’ve given. oOf course, I would need to see the scalp or a photo of your scalp myself to know for sure one way or another.
Please keep taking photos of your scalp to show your doctors. If you feel that your hair returns to full by September 2021 and you are really pleased with the way your hair looks and feels at that time, then it’s pretty unlikely there is any AGA. However, if your hair does not return to full by September, I would encourage you to further explore ways to confirm this diagnosis with certainty one way or another so that you might get connected with the correct treatment in the event you do have androgenic alopecia.
Thank you again for your question.