Hydroxychloroquine (Plaquenil) for Frontal Fibrosing Alopecia
Hydroxychloroquine (Plaquenil) for FFA
I’ve selected this question below for this week’s question of the week. It allows us to discuss the use of hydroxychloroquine (Plaquenil) in FFA as well as the rare cardiac effects of hydroxychloroquine.
QUESTION
I am a female in my late 70s with frontal fibrosing alopecia, confirmed by a scalp biopsy. It is being treated with clobetasol .05%, one application per day. I have read that this is not a very effective treatment when used alone. What would you suggest might be used with it?
My dermatologist suggested hydroxychloroquine (plaquenil), but I read that this might have an adverse effect on people with heart disease. Do you agree? The first symptom about six months ago was drastically thinning eyebrows. I am in the third month of treatment and hair loss around the hairline is not yet apparent. I have cardiomyopathy and atrial fibrillation, for which I am taking a blood thinner (Eliquis) plus daily irbesartan, bisoprolol and spironolactone. Do you think any of these drugs might be the cause of my FFA?
ANSWER
Thanks for the great question. I’d like to discuss several important points in the question you ask and the information you have submitted.
Before we go further, I’m going to assume here in your question that the diagnosis is correct. Can I be 100 % sure you have FFA? Well no - not at all. I haven’t seen your scalp and eyebrows and I don’t know all the details of your story. You might reply to me that you have already told me you had a biopsy. Well, biopsies are not 100% either. Nevertheless, it sure sounds like many aspects of your story do, in fact, support a diagnosis of FFA. So I’ll proceed with this assumption. If you do have FFA, this answer then helps. If the diagnosis is not correct, then the answer has helpful points nevertheless for others with the condition.
Let’s look at some aspects of your question:
a) How good is hydroxychloroquine in FFA?
Hydroxychloroquine is helpful in some patients with FFA. I tell my patients it’s a silver medalist. In other words, it can be helpful, it’s just that other treatments are probably better. We will get into that a bit later. That does not mean hydroxychloroquine is useless as a treatment. Not at all. For some patients with FFA, hydroxychloroquine does help. It does not help everyone that is for sure.
Let’s look at some helpful studies from the past evaluating the effectiveness of hydroxychloroquine in FFA treatment.
in 2013, Ladzinski and colleagues proposed that hydroxychloroquine had some benefits in about 50 % of patients,
In a much larger study conducted in 2014, Vano Galvan et al showed that a 15 % of patients with FFA using hydroxychloroquine had some improvement in their disease. 59 % had their disease stabilized. For about one quarter of patients, the drug did nothing helpful at all.
in 2018, Strazzulla and colleagues found that about 70 % of patients had some benefit with hydroxychloroquine - with results being more or less the same ass doxycycline.
A 2010 study by Samroa and colleagues found that hydroxychloroquine reduced redness and inflammation in FFA patients.
Treatment Options for FFA
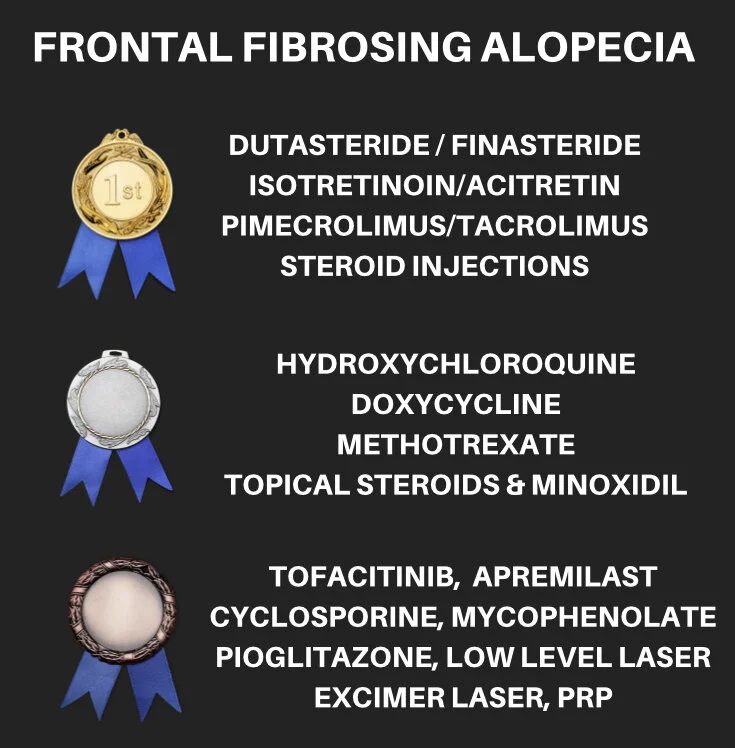
Before we leave the subject of hydroxychloroquine for treatment of FFA, let’s look at the options for treatment. Every single type of hair loss has treatment options. The thing that is often forgotten is that not all treatments are the same. Some are good. Some are not so good. Some are good but crazy expensive. Some are good and not so expensive. Some are good and fairly safe and some are good and incredibly risky. I divide every disease into gold, silver and bronze medal treatments.
I personally like this analogy of categorizing treatments because it reminds us of a couple of key things. First, not all treatments are equal. We select treatments by balancing benefit and risk and take into account the safety, affordability, feasibility and effectiveness of treatment (what I have previously termed the "S.A.F.E." Principle. )
The second reason I like the analogy of gold and silver and bronze medal treatments is because it reminds us that this is not always going to be the order. The athlete that received the gold medal in the recent Olympics may not be the athlete that gets the gold medal in the next Olympics. Of course, if the athlete is really good - he or she will probably be up there one the podium in the top spot again in 4 years. The same is true with hair loss treatments.
As new treatments come out and as they are studied more and more, a certain treatment might just rise into the gold medal spot and push out other treatments that are there now down into silver or bronze positions. Sometimes, a treatment gets removed from the market entirely just as some Olympians get disqualified from the Olympics. They disappear entirely.
In the diagram below, I outline what I consider the gold, silver and bronze treatments for FFA. In FFA, Plaquenil is a silver medallist. It’s not useless. It has reasonable safety (although I will discuss the heart issues next). It’s relatively inexpensive (Plaquenil is about $1300 USD per year whereas Apremilast is $ 18,000 USD per year). It’s easy to use. It’s somewhat helpful. In terms of the SAFE principle, it’s an okay option to keep in mind for many.
b) Does hydroxychloroquine have effects on the heart?
Hydroxychloroquine can have effects on the heart. Fortunately, they are not common but risks do increase with advancing age. In fact, physicians need to be much more on alert for eye, muscle, heart side effects in patients over 65 compared to those under 65. Of course, side effects of this nature can happen at any age - but they are more common with advancing age. Hydroxychloroquine cardiotoxicity is non common - but it is a serious side effect.
Plaquenil “cardiotoxicity” (potential toxicity on the heart) has best been studied inn patients with the autoimmune disease lupus who take the drug and also to seem degree in patients with rheumatoid arthritis. Could it be that a these groups are more likely to experienced heart muscle side effects with Plaquenil? Could be, but more studies are needed. For now, it’s a potential side effect that needs to be considered in everyone. There’s nearly 100 reports in the medical journals now of hydroxychloroquine induced heart toxicity. When it does occur, the patient usually develops a restrictive or dilated cardiomyopathy or has conduction system abnormalities including atrioventricular block and bundle branch block. Studies by Costedoat-Chalumeau showed that when cardiomyopathy is present other signs of toxicity are often present as well - eye toxicity, nerve toxicity, and muscle toxicity.
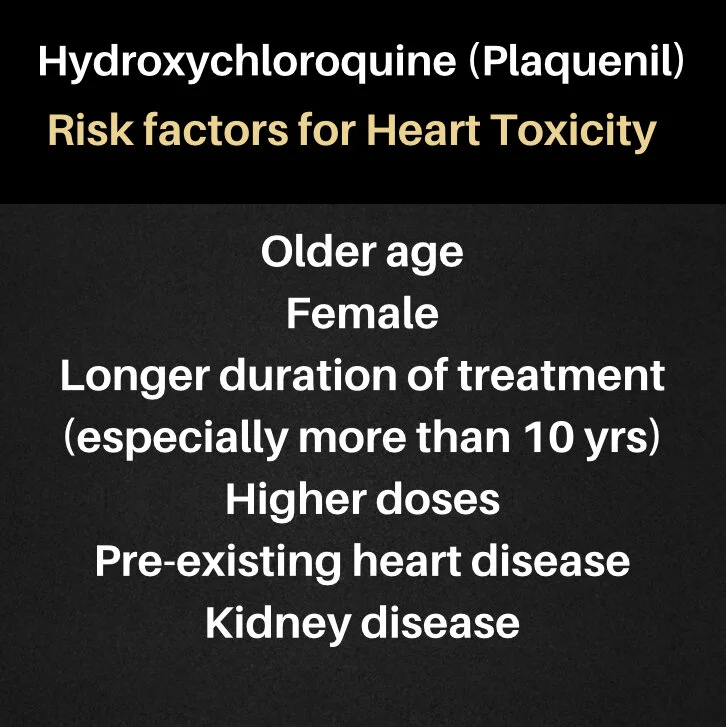
So who is more likely to get hydroxychloroquine induced cardiomyopathy ? Risk factors are currently proposed to include older age, female sex, longer duration of therapy (>10 years), higher doses of the drug, pre-existing cardiac disease, and renal insufficiency (kidney disease). It’s important to remember that most patients who develop hydroxychloroquine cardiotoxicity have been on the drug a long time - ie 10 years or more. Of course, there are reports in the medical journals of those who have been on it just a few months before developing side effects.
The Lane and Colleagues 2020 Study
Finally, I’d like to tell you about an important study by Lane and colleagues. This was recently published. This was a study of almost 1 million ( 956,374) hydroxychloroquine users so it’s a massive study. Massive studies of this size are important because they allow us to get a better sense of the risk associated with certain drugs. Lane’s study focused non patents with rheumatoid arthritis (not FFA) so we need to always keep that in mind. The researcher showed that long-term hydroxychloroquine use increased cardiovascular mortality 1.65 times compared with control treatments There are some limitations of the study (as there are with any study). nevertheless, it points to the fact that there may be a slight increase risk of heart related effects with long term use of hydroxychloroquine - at least in patients with rheumatoid arthritis. Fortunately, side effects of this nature are still quite uncommon.
In conclusion, there are some small risks with hydroxychloroquine use in your case. This is something you’d certainly want to review with your heart doctors too. Depending on the degree of heart issues (class of heart failure, etc), it may be something they agree with at a low dose, or something they advise against.
c) What would you suggest might be used with clobetasol?
This is actually a very involved question. If you find that use of clobetasol in the manner described and recommended by your doctors stops further hair loss completely - then you don’t need to use anything else. The key to treating FFA is not to pile on more and more drugs but rather to use the safest and simplest approach possible that stops the disease. if clobetasol stops your FFA 100% - then you need not look for anything else.
Is it likely that clobetasol stops your disease 100%? Well, no. But again - it’s not impossible that it does. It’s a silver medallist.
There are some 20 other options available. Again we follow a logical approach to deciding on which other treatments to use. We select treatments that have good evidence from good studies as well as treatments that have good safety.
You may want to review with your doctors other options like topical calcineurin inhibitors (like Pimecrolimus) as well as low doses of steroid injections (2 mg per mL) every few months. Topical clobetasol is going to give atrophy after a few months of daily use so you and your doctors are going to need to decide when to start reducing that dose.
You can also review options like topical anti androgens (topical finasteride) or even oral dutasteride. Starting two times weekly could be something that you are your doctors discuss. You’ll want to carefully review if you have any contraindications to its use (depression, cancer risks, osteoporosis). Adding acitretin once weekly or twice weekly may also be something you discuss.
d) I am taking a blood thinner (Eliquis) plus daily irbesartan, bisoprolol and spironolactone. Do you think any of these drugs might be the cause of my FFA?
Some drugs do contribute to the development of FFA. For example, the antiestrogen tamoxifen is one of them. The drugs on your list have not been implicated to date in the development of FFA. However, some can cause hair loss - just not FFA.
I’ll make a few additional comments at this point. First, your patterns of hair shedding are going to be important in giving you the fullest answer possible. Your story is interesting in that it seems that you have eyebrow loss without scalp frontal loss yet. Yes, that sure sounds like FFA but again I can’t say much more because I don’t know much about your story and haven’t seen your scalp. If your hair shedding is markedly increased the question must be posed to your health care team as to whether there is any component of telogen effluvium as well. All the drugs on your list can cause telogen effluvium - fortunately that’s still really unlikely overall. Most people have no issues of the sort.
Now on to the tricky part. it’s not possible to 100% say that the drugs you are taking had nothing to do with the development of FFA. Beta blockers (like bisoprolol), angiotensin II receptor blockers (like irbesartan) and spironolactone have rarely been involved in skin rashes known as “lichenoid” drug eruptions. There is some similarity between lichenoid drug eruptions and the lichenoid eruption that is part of the pathology of frontal fibrosing alopecia. Have any of the drugs you are taking been convincingly implicated in the development of FFA? No. It is possible there is some link in those with some sort of predisposition to this disease ? Yes.
Conclusion and Summary
Thanks for submitting your question. I do hope this will be helpful in the discussions you have with your doctors. I’ve included references below in the event they too are helpful. I wish you the best of health.
Reference
August C, Holzhausen HJ, Schmoldt A, et al. Histological and ultrastructural findings in chloroquine-induced cardio- myopathy. J Mol Med (Berl) 1995; 73: 73–77.
Baguet JP, Tremel F and Fabre M. Chloroquine cardiomypathy with conduction disorders. Heart 1999; 81: 221–223.
Clark C, Douglas WS. Lichenoid drug eruption induced by spironolactone. Clin Exp Dermatol. 1998 Jan;23(1):43-4
Costedoat-Chalumeau N, Hulot JS, Amoura Z, et al. Cardiomyopathy related to antimalarial therapy with illustra- tive case report. Cardiology 2007; 107: 73–80.
Fesssa et al. Lichen planus-like drug eruptions due to β-blockers: a case report and literature review. Am J Clin Dermatol 2012 Dec 1;13(6):417-21.
Ladzinski et al. Frontal fibrosing alopecia: a retrospective review of 19 patients seen at Duke University. J Am Acad Dermatol. 2013 May;68(5):749-55.
Lane, J. C. E. et al. Risk of hydroxychloroquine alone and in combination with azithromycin in the treatment of rheumatoid arthritis: a multinational, retrospective study. Lancet Rheumatol. (2020).
Massa MC, Jason SM, Gradini R, Welykyj Lichenoid drug eruption secondary to propranolol. Cutis. 1991 Jul;48(1):41-3.PMID: 1831116
Nord JE, Shah PK, Rinaldi RZ, et al. Hydroxychloroquine cardiotoxicity in systemic lupus erythematosus: a report of 2 cases and review of the literature. Semin Ann Rheum Dis 2004; 33: 336–351.
Pfab et al. Lichenoid drug eruption due to an antihypertonic drug containing irbesartan and hydrochlorothiazide. Allergy 2006; 61(6):786-7
Samrao A et al. Frontal fibrosing alopecia: a clinical review of 36 patients. , Chew AL, Price V.Br J Dermatol. 2010 Dec;163(6):1296-300.
Schön MP, Tebbe B, Trautmann C, Orfanos CE. Lichenoid drug eruption induced by spironolactone.Acta Derm Venereol. 1994 Nov;74(6):476.
Strazzulla LC et al . Prognosis, treatment, and disease outcomes in frontal fibrosing alopecia: A retrospective review of 92 cases.. J Am Acad Dermatol. 2018 Jan;78(1):203-205. doi: 10.1016/j.jaad.2017.07.035.
Vano-Galvan S. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol . 2014 Apr;70(4):670-678.
Yogasundaram H, Putko BN, Tien J, Paterson DI, Cujec B, Ringrose J, Oudit GY. Hydroxychloroquine‐induced cardiomyopathy: case report, pathophysiology, diagnosis, and treatment. Can J Cardiol 2014; 30: 1706–1715.