Why am I shedding?
What are the reasons for my shedding?
I’ve selected this question below for this week’s question of the week. It allows us to review some concepts in hair shedding.
Question
I am in my mid 50s, healthy and fit and not taking any medications except hormone replacement therapy started last year.
2 years ago I had a dramatic increase in hair shedding, more than 300 hairs a day. My temple area was always a bit thinner and so that area had shown the most visible loss, but the loss is all over my head, top, sides, back. The hairs that fall are almost all long hairs with a white bulb attached. I had started experiencing my first menopausal symptoms a few months prior to this increase in shedding.
The excessive shedding lasted 6 months or so and then slowed down and things seemed to return back close to normal shedding and hair density improved. It was during this time of normalization that I started hormone replacement therapy. After about 5 months on hrt, I cut my hormone dose in half. Less than 2 months later, the massive shedding started again.
Other considerations may be that 4 months prior to this second shedding, I was sick with a fever (not covid) and I also had the covid vaccine around that time, which triggered another fever that lasted for a couple days.
I have had blood tests done and everything is within range, except my ferritin is at 15. Vitamin D and thyroid are normal.
My scalp is itchy at times, but not constant and not sore or red or sensitive. There is a visible difference is how thick my hair looks now. It feels like I have lost 50% of my hair. I should note that I am always under chronic stress which has increased significantly since menopausal symptoms began 2 years ago.
Could this be AGA, TE, both? And depending on the diagnosis, would Minoxidil work (topical or oral) or Finasteride or something else?
PHOTO 1: FRONT OF THE SCALP
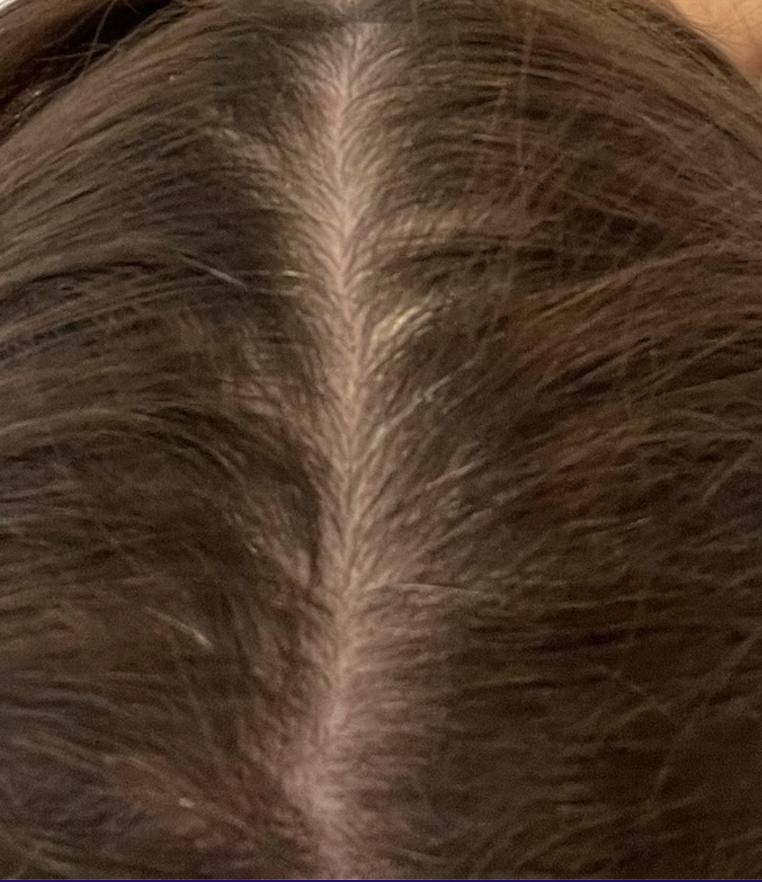
PHOTO 2: BACK OF THE SCALP
PHOTO 3: HAIRLINE
PHOTO 4: TEMPLE AREA
Answer
Thanks for the question. It’s pretty clear that telogen effluvium is a component of the loss and I also suspect some degree of androgenetic alopecia here - as well as seborrheic dermatitis. Without seeing the scalp up close myself with trichoscopy and knowing a great deal more of your story, it’s difficult to say whether any other cause of redness is contributing here (such as scarring alopecia, psoriasis, allergic contact dermatitis, or other immune based scalp disease). Overall, I don’t think it’s very likely especially when there have been periods where shedding really improved a great deal. (We don’t usually see shedding just settle so dramatically if an immune based issues is present).
TELOGEN EFFLUVIUM
Your story fits well with a telogen effluvium - and likely two episodes at least of telogen effluvium. Telogen effluvium is a hair shedding disorder and happens following a trigger in cases of the classic ‘acute telogen effluvium’. Triggers include stress, low iron, thyroid disease, medications, crash diets, scalp inflammatory disease, fevers and internal illness. Shedding happens 1-3 months after the trigger and improves once the trigger is resolved.
TELOGEN EFFLUVIUM FROM LOW FERRITIN
I’m a bit concerned about your ferritin of 15 and certainly that needs to be looked into further. Most women age 55-60 have ferritin levels in the 75 range. Some women age 55-60 have a ferritin of 50 and some have 150. But 15 is actually abnormally low. You and your doctor need to discuss this and look up old ferritin levels in past blood tests. If you have had a ferritin level of 15 for the past 40 years it’s less of an issue from the hair perspective. If it was much higher in the past and now it is lower, then that’s a concern. Other tests need to be measured including CBC, RDW, MCV, MCHC, MCH. These are standard parameters but give key information. B12 levels, folate, ESR, creatinine, zinc, AST, ALT and also helpful in a situation like this. If you have low hemoglobin (less than 12.0 in the USA and less than 120 in International units), the necessary tests may expand a bit further than these.
THE “OTHER BLOOD TESTS”
Other tests may be useful too but it all depends on what information is found when a thorough history is done and when the scalp and skin and nails are examined. I can’t go through all the possibilities as the list is enormously long. For example, if there are new joint symptoms an RF (rheumatoid factor) and ESR and anti-CCP may be advised. If there are muscle symptoms or certain skin rashes a CK and ANA may be advised. If there are significant concerns for dry eyes and dry mouth and extractable nuclear antigen blood test may be advised. If there are any nutritional concerns, a zinc level might be added. If there is any hair growth on the face, change in voice, or acne then a testosterone and DHEAS might be advised. If there are bruising, muscle weakness and fat redisribution, an AM cortisol might be ordered.
In anyone with shedding that is chronic, a really thorough history and examination is critical.
IRON SUPPLEMENTATION AND TESTING
Starting iron supplementation is likely to be part of the plan. But not first without a thorough discussion with your doctor. Colonoscopy screening is to be discussed too. The age range is dropping for who should be screened with colonoscopy. But this is something you should talk to your doctor about. The U.S. Preventive Services Task Force (Task Force) recommends that adults age 45 to 75 be screened for colorectal cancer. This is regardless of a person’s hemoglobin or ferritin level. I highly advise colonoscopy screening in my own patients with similar stories as you have given. If you’ve already had that screening then that’s great. But this is something you need to discuss with your providers. Mammography is also necessary. The U.S. Preventive Services Task Force (Task Force) recommends that all women 50-74 have mammography screening every 2 years.
Low iron comes from many reasons including poor absorption or poor intake, excessive loss and excessive demand. There are some 30 reasons why someone can have low iron. This needs to be looked into.
There’s nothing wrong with starting iron therapy provided you have a plan in place to further investigate why it is your ferritin is low.
Low ferritin can contribute to hair loss for many patients - especially a ferritin level of 15.
TELOGEN EFFLUVIUM FROM MEDICATION STARTING AND ADJUSTMENTS
It is likely that starting and adjusting HRT medications has given some shedding too. Provided levels stay the same, this particular cause of shedding will settle out and disappear from the list (usually). But every dose adjustment could give shedding again.
SEBORRHEIC DERMATITIS
I suspect in the photos that there is seborrheic dermatitis present. It’s quite possible this accounts for at least some of the redness seen in the photos and the itching. Whether it accounts for all the redness is not clear. I would need to see the scalp up close. It may make sense for you and your doctors to discuss a really solid seborrheic dermatitis treatment plan. This involves ‘dandruff’ shampoos used 2-3 times per week. Ingredients like ketoconazole shampoo, zinc pyrithione shampoo ciclopirox shampoo and selenium sulphide shampoo can help. These should be left on 2-3 minutes although sometimes we advise 3-5 minutes depending on the situation. They can be drying. Use of a mild corticosteroid lotion can help a great deal if you get itching.
THE ‘RED SCALP’
There are many causes of ‘red scalp’ and the list is long. I’m not too suspicious of any of these being relevant in your case but no it’s not possible to say 100% because I don’t have the whole story and I don’t have the chance to see the scalp up close myself. Some conditions are great great mimickers and always need to be considered including lichen planopilaris and contact dermatitis. A proper examination with trichoscopy can exclude the condition known as lichen planopilaris with reasonably high certainty. If anyone has doubt, a biopsy of the scalp can be done and is quite safe and easy to do. I don’t think you have this condition but you do appear to have seborrheic dermatitis scale that can hide other conditions. Again, I’m not too suspicicious about any sort of scarring alopecia and I see very large numbers of patients with this rare condition.
Allergic contact dermatitis is always to be considered. Nothing really worries me in your story so far about contact dermatitis except for the fact that we need to figure out the cause of your redness. It appears to be seborrheic dermatitis for at least one of your causes. If you get rashes on the face, neck, eyelids, ears, chest, the chances of a true allergy to some topical product in your life goes up a bit. These can give itching and shedding and include shampoos, conditions, styling agents, dyes, mousse, etc. I’m not really of the opinion this is likely to be a culprit here but someone needs to give it a passing thought with proper examination and proper questions. If there is even a hint of suspicion about allergic contact dermatitis, referral for ‘patch testing’ can be done. This is done usually by a dermatologist in most countries although some allergists will also do.
ANDROGENETIC HAIR LOSS
There is likely a component of androgenetic alopecia here. I feel that it’s not the only cause as there is most certainly a telogen effluvium here as well as seborrheic dermatitis. But AGA is quite likely a part of why you are losing hair. The frontal scalp zones appear less dense than other areas although you do have diffuse loss as well. A proper examination and use of trichoscopy can confirm the diagnosis of AGA. But it seems to be a component.
TREATMENT
There are a large number of treatments that can be considered here. The exact plan will depend on the final diagnosis. Because I can’t offer a definitive diagnosis, I can’t give a definitive plan. If we assume the diagnosis is androgenetic alopecia with seborrheic dermatitis and telogen effluvium then first we need to treat the seborrheic dermatitis and investigate the cause of low iron while starting supplementation of some kind. A really thorough history and physical will determine if you need more blood tests done. If any other labs (blood tests) come back abnormal, they need to be addressed. I think that’s pretty unlikely.
In addition to iron supplementation, dandruff shampoos and possibly topical corticosteroids, you can also consider one or more of the following for treatment of the androgenetic hair loss: topical Rogaine, oral minoxidil, finasteride, low level laser and PRP. For someone with your story, I’d generally advise starting Rogaine with or without finasteride and then deciding from there whether to add laser, PRP or oral minoxidil in the future.
SUMMARY
Thanks again for the question. I hope this helps. I think seborrheic dermatitis, telogen effluvium and androgenetic alopecia are the three diagnoses. I can’t say it’s chronic telogen effluvium you have because really what it seems like we are dealing with is an acute TE that has not been fully addressed.