Increased Shedding: Should I start treatment for Male Pattern Balding?
Does increased shedding indicate that a male should start finasteride?
I’ve selected this question below for this week’s question of the week. It allows us to the review the diagnosis and work up of increased hair shedding in males.
QUESTION
I am a male, 30 years old who has been monitoring his hair for quite some time as I don't want to lose my hair to androgenetic alopecia (AGA). I have been counting the hairs that I shed in the shower since around 2016. Since I have usually midlength to long curly hair I stretch out the days I wash my hair, otherwise it gets dry. I have always shed around 210/220 hairs when showering every third day. This has increased to 280 since a few weeks now.
Since I said every third day this means the average on a day was: 210/3=70 . Now it has become 280/3=93 a day, for the last month or so. I know that 100 hairs a day is normal, but considering that the number I was shedding was consistently around 70 for years I am a little worried. The majority of the shed hairs look healthy and thick and long. My hairline, crown and density are still the same. Could this be temporary and could the shedding go down within the next few months?
When should I start finasteride? As soon as I see recession / lessening in density / thinning?
In short, is a little increase in shedding a reason to go on treatment?
ANSWER
Thanks for submitting this question.
I’d like to discuss several important things in the question you ask and the information you have submitted.
Before we do go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s story
2) the findings uncovered during the process of the scalp examination including trichoscopy
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis. I don’t have a full story in your case and I don’t have photos (or a chance to examine the scalp) and I don’t have the opportunity to review any tests …. so I am limited to some degree in my helpfulness. Nevertheless, I do think the discussion here will be helpful.
The main phenomenon you are describing is increase shedding. You have gone from 70 hairs per day of shedding to 93 hairs per day . Although both are considered within the realm of normal, I would agree that in your case this likely represents a true increase in shedding. This does not necessarily mean that this will be long term shedding or that it will actually translate into a loss of hair density or thickness. There are some unknowns here.
There are 3 potential considerations for why you are shedding more hair in the last month:
a) a telogen effluvium has occurred
b) the initiation of androgenetic hair loss has taken place
c) an autoimmune mimicker of telogen effluvium is present rather than telogen effluvium
d) combination of the above
Let’s take a look at these in more detail.
a) Is this a true telogen effluvium and if so what is the cause?
It’s quite possible that you are having a minor telogen effluvium. Hair shedding does not need to be over 100 hairs per day to have a telogen effluvium - it just needs to be more than one’s original shedding rates. If a person shed 38 hairs per day before and now sheds 68 - it’s abnormal. In your case, your shedding from 70 to 93 is abnormal. Of course, there is a big difference between something being abnormal and something being serious. Your hair shedding may not be serious and might only be temporary. We’ll get to that in moment. But this shedding suggests a potential diagnosis of telogen effluvium. As we’ve reviewed in the list above, a diagnosis of telogen effluvium is not the only cause of shedding. So it would be a mistake to assume otherwise.
A variety of ‘triggers’ are responsible for telogen effluvium. These triggers include stress, low ferritin levels, thyroid problems, medications, weight loss, seborrheic dermatitis, scalp psoriasis, immunizations, infections and internal illness inside the body.
You and your doctors really need to go through each of these potential triggers step by step very carefully to see if anything fits with your story. If your shedding started at the beginning of April, then you’ll want to go back to January or February (2-3 months prior) and ask yourself if something changed in your life. If this is a telogen effluvium, that’s probably when the body felt some sort of a trigger.
So, you and your doctors will want to evaluate that answers to the following
1) Did you experience higher stress levels in January or February?
Stress in January can trigger shedding 8-12 weeks later.
2) Did levels of any of your key blood test parameters change in January or February?
Clearly, blood tests are going to be needed if you really want to get to the bottom of why you are shedding more. There are over 75 blood test abnormalities that can trigger shedding. Fortunately, most of those 75 are rare and we don’t go about even ordering them. The ones we mainly check are iron (ferritin levels) and thyroid (TSH test) along with basic hemoglobin level and 25 hydroxy vitamin D level. However, your doctor will need to review your story from start to finish and examine your scalp and ideally perform aa physical examination too. If there’s anything that crops up as a concern, more blood tests besides just ferritin and TSH might be needed. For example, patient who has lost 25 pounds in 2 months and has no idea why they are losing so much weight is likely going to need an extensive work up.
3) Did you start any new medication or vitamin or supplement in January or February?
Starting medications can sometimes be a trigger - and the same is true for some supplements, herbal medications, teas, and vitamins. This all needed to be reviewed.
4) Did you stop any sort of medication or vitamin in January or February?
Stopping medications can sometimes be a trigger - and the same is true for some supplements, herbs, teas, vitamins. This all needed to be reviewed. In addition to stopping medications. sometimes even changing brands can be an issue. For some people, a change in drug A from brand name to generic is enough to trigger a shed. You can see that we’re going to need aa pretty detailed understanding of what’s been happening in your life to determine why you area shedding.
5) Did you receive any sort of immunization in January or February?
Immunizations are not common causes of shedding but that does not mean they are not on the list. Immunizations of all kinds have a slight chance to trigger some temporary shedding. COVID vaccination rarely does too. I don’t know if you received a vaccine or not, but your doctors will need to review this carefully. If you were vaccinated in January or February, it most certainly could give a shed now. Fortunately, it’s pretty rare - but we’ve seen it.
6) Did you get any kind of infection in January or February?
Infections of any kind can trigger shedding. Granted, severe infections associated with someone being quite ill are more likely overall to trigger shedding than less severe infections. But even minor infections can trigger shedding. Tooth infections, flus, COVID 19, all can trigger shedding. Many patients who have been infected with COVID 19 do not even know they had COVID 19 but some still get shedding. In fact, about 10 % of patents with hair shedding due to COVID 19 didn’t really have any COVID 19 symptoms. You and your doctors are going to want to evaluate that carefully and whether there is any possibility of an asymptomatic COVID 19 infection happened in January or February. Antibody tests can help address this question in some patients.
Other infections may also be relevant to ask about. Again, over 300 infections can cause shedding but most of the time, none are all that relevant for the patent in front of the doctor. But a variety of bacterial, viral, protozoal infections can cause shedding. In some of my patients from outside of North America, Dengue fever (spread by dense virus) is a common cause of shedding. There are estimated to be 390 million Dengue viral infections every year in the world. Sometimes we test for infections like HIV and syphilis in patients with risk factor who have chronic shedding. So depending on your story, more broad testing could be needed. For most people, we don’t need much in the way to these sorts of tests.
7) Did you develop any kind of illness inside my body in January or February?
Any illnesses inside the body can trigger shedding. Most often these are illnesses that a significant impact on the body. For example, an illness that causes diarrhea or a bad cough or an intensively sore joint that affects the motion in the joint all have the potential to cause shedding.
8) Did you have any kind of surgery or procedure in January or February?
Any proper evaluation for shedding examines whether or not the patient had any type of surgery or hospitalization in the months leading up to the shedding. Medications used in surgery, blood loss during surgery are well known triggers of telogen effluvium.
In summary, you can see that if you want to get to the bottom of what is happening with your hair, you are going to need a proper history and examination and you are going to need blood tests. Whether you get blood tests now or simply wait a month or two if things don’t improve is a clinical decision that is left to you and your doctors. But the only way right now to be sure that an abnormality in some blood test is not the reason why your shedding went from 70 to 93 is to order these blood tests.
Three Important Patterns of Telogen Effluvium
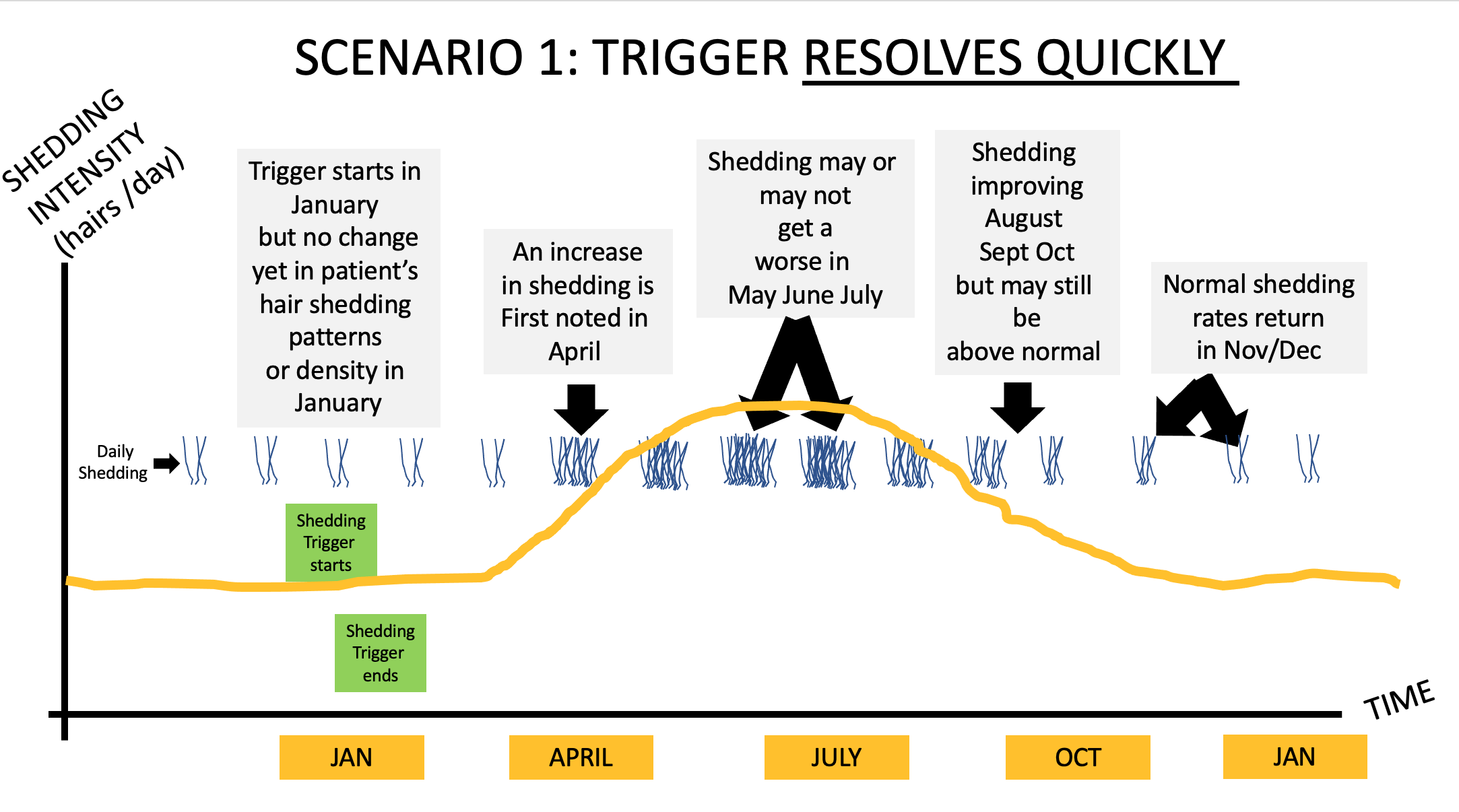
Before we leave the concept of telogen effluvium, it’s important to mention a few more points regarding the patterns of shedding that you might see. There are a few scenarios that might happen. If the diagnosis of your hair shedding is telogen effluvium and there is some well defined trigger that happened to you in January or February and then went away you will have some shedding in April through July but then the months of August September and October will be associated with less shedding and things should return to normal by November or December (assuming you don’t have genetic hair loss). If you do have genetic hair loss, that’s a bit of a different story as patients who are en route to slowly developing genetic hair loss may not find there shedding goes back completely to normal once the trigger of the telogen effluvium is fixed. We say in this case that the TE precipitated or unmasked an androgenetic hair loss.
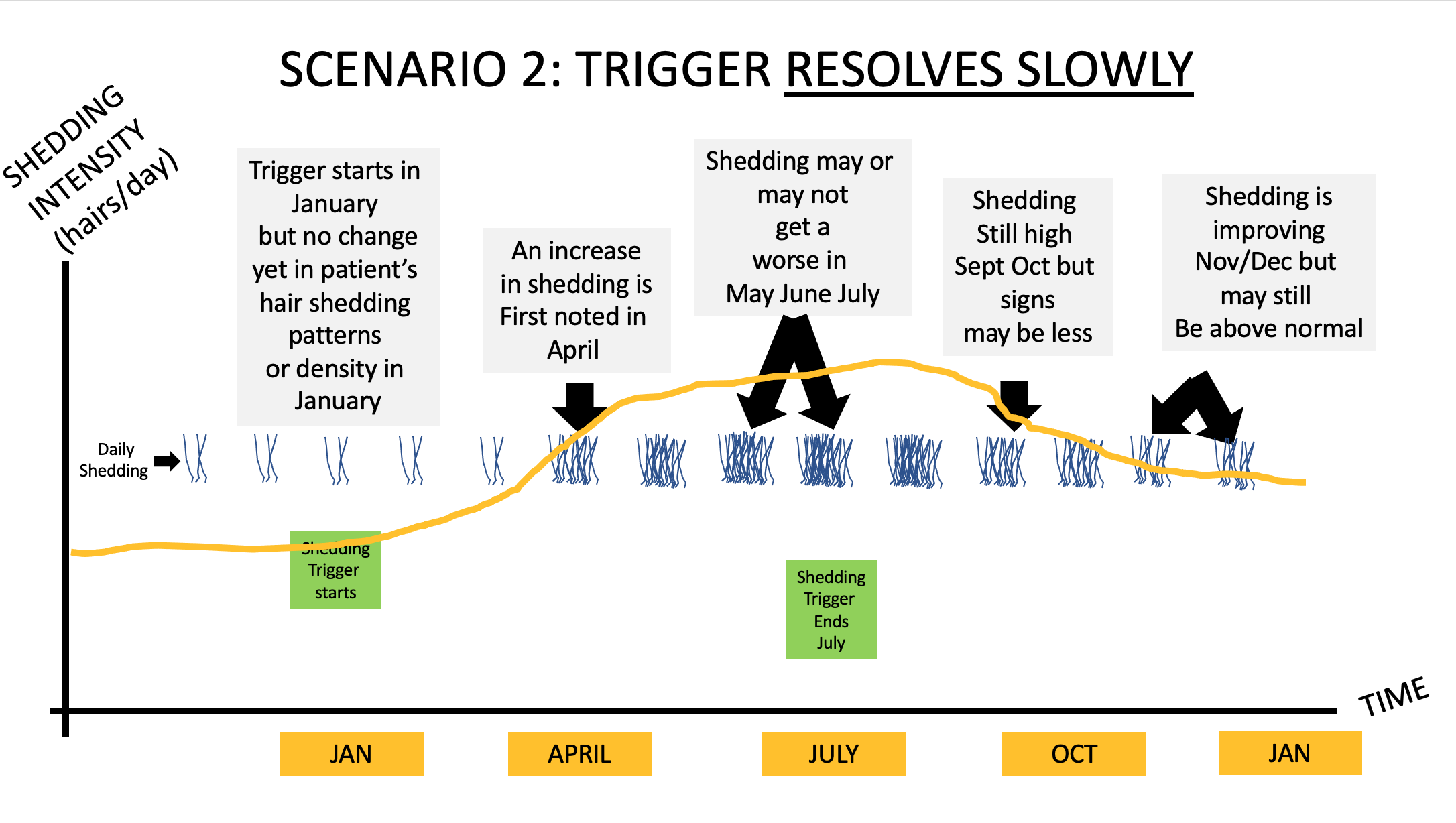
Let’s take a look at scenario 2 now. If the diagnosis of your hair shedding is telogen effluvium and there is some well defined trigger that happened to you in January or February but is not going to end up being fixed until July then you will have a bit more prolonged shedding. This could be a scenario whereby an individual went on a diet from January to July or had intense stress from January to July or developed a thyroid problem in January and could not get into the doctor until July to get it fixed. If scenario 2 applies in your case, you will not slow your shedding quite as quickly. You will have some shedding in April through July but then the months of August September and October will be associated with less shedding and things should return to normal by November or December (assuming you don’t have genetic hair loss). If you do have genetic hair loss, that’s a bit of a different story as patients who are en route to slowly developing genetic hair loss may not find there shedding goes back completely to normal once the trigger of the telogen effluvium is fixed.
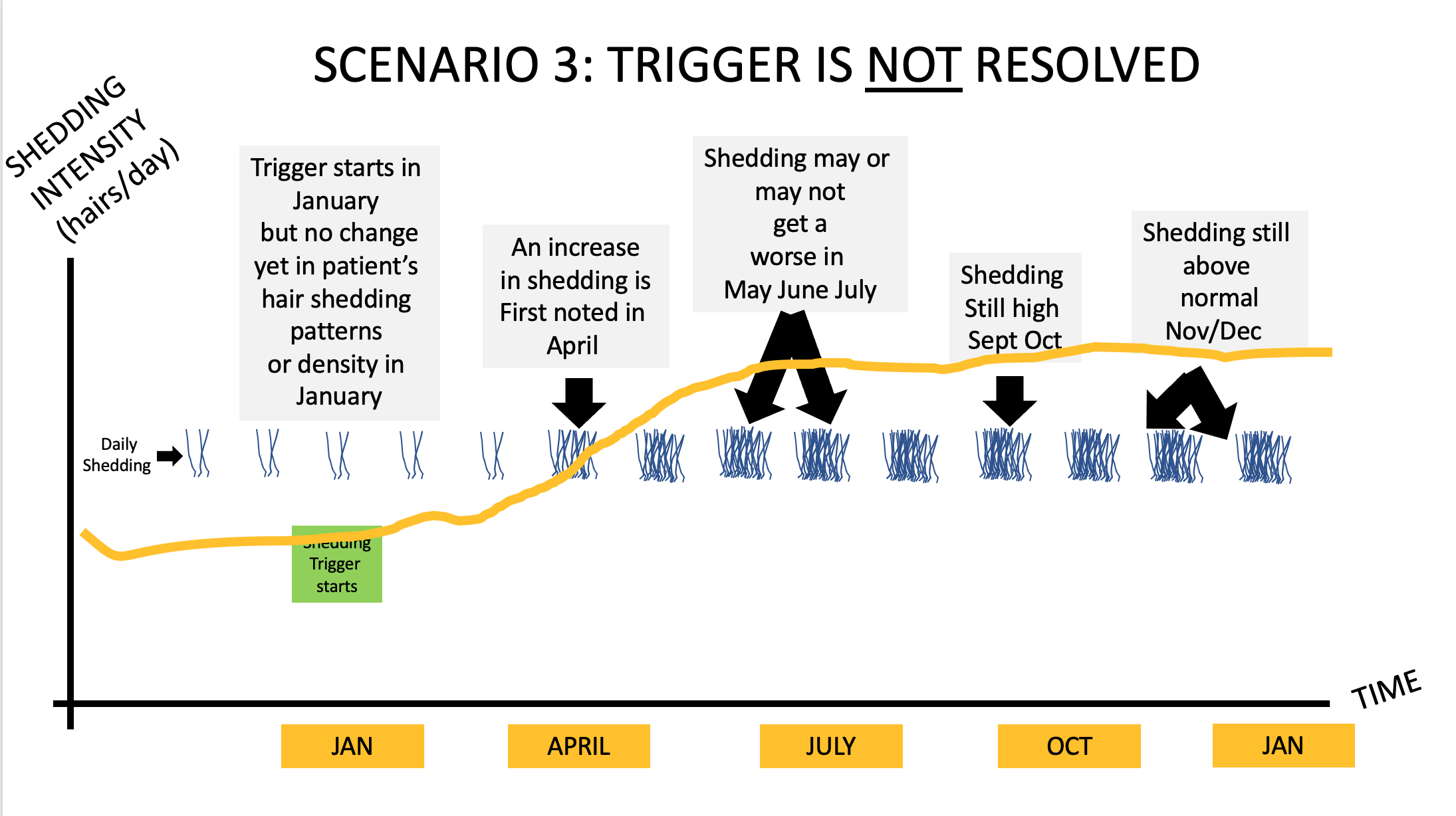
Let’s take a look at scenario 3 now. If the diagnosis of your hair shedding is telogen effluvium and there is some well defined trigger that happened to you in January or February but it simply goes unfixed then you will have a prolonged shedding and it’s not going to stop. This could be a scenario whereby an individual developed a chronic illness like inflammatory bowel disease in January and does not get connected with the right treatment because either the diagnosis has not yet been even uncovered or the medications are not working. Another example would be a patient who experience high stress starting January because they are caring for a terminal ill member of the family and the stress just continued to run high. Another example is patient who develops an unknown chronic illness in January but just can’t get the right diagnosis and shedding just goes on and on because the issue is not addressed.
If scenario 3 applies in your case, you will not slow your shedding at all until the problem is fixed. You will have some increased shedding starting in April but then it will persist. Only when the trigger actually gets fixed will you shedding resolve.
b) Is this the start of androgenetic hair loss?
You are very wise to consider the possibility that your increased shedding is actually a reflection of androgenetic alopecia arriving on the scene. Very wise. More hair specialists and patients need to get into the frame of mind that hair shedding means potentially so much more than simply a diagnosis of telogen effluvium. What’s the most likely cause of chronically increased shedding in a healthy 30 year old male with normal blood tests? Androgenetic alopecia is the answer.
Now, are you a 30 year old male with chronically increased hair shedding and normal blood tests? No, you are not. You are a 30 year old male with acutely increased shedding (just a few weeks so far) and I have no idea what your blood tests show.
So you could have the early stages of endogenetic alopecia and this diagnosis becomes more and more likely if your shedding does not reduce as time goes on and more and more likely if all your blood tests come back normal.
Is now the right time to start finasteride?
You have asked a great question - is now the right time to start finasteride? In my opinion, a male should only every consider finasteride if five conditions are met. Interested readers can read more about these in a previous article that I wrote last year.
Criteria 1: The individual has a proven (confirmed) diagnosis androgenetic alopecia
Criteria 2: The individual does not have any contraindications to finasteride
Criteria 3: The individual accepts the potential side effect profile of this drug
Criteria 4: The individual has considered the other treatment options but feels they are not better than finasteride as a starting point (topical minoxidil, oral minoxidil, laser, PRP)
Criteria 5: The individual plans to use the medication lifelong.
A little bit of shedding that is due to AGA is certainly a reason to consider starting treatment but it does not necessarily mean it has to be with oral finasteride. It could be topical minoxidil, topical finasteride, laser or PRP . There’s nothing wrong with being conservative in the early stages and seeing if the AGA can be halted with minimal coaxing.
Before leaving the topic, let me reiterate how important criteria one actually is. If you had some major stress in January or February and telogen effluvium is actually the cause of your shedding rather than a diagnosis of androgenetic alopecia, starting finasteride would not be the right step, If you are shedding 93 hairs because your diet is poor and you have a micronutrient deficiency, starting finasteride is not the right step, However, fixing the diet or starting a vitamin in the meantime would be .
c) Is this a mimicker of telogen effluvium ?
There are many conditions that look like telogen effluvium, sound like telogen effluvium but aren’t telogen effluvium. Unfortunately, they can be tough to spot for even clinicians. Fortunately, they are not common. Alopecia areata incognito is not common but presents with shedding. Trichoscopy is needed for the diagnosis (or a biopsy). It’s usually not so perfectly symmetrical as seen with AGA but it can be of course. It responds to topical steroids and Rogaine. Lichen planopilaris and folliculitis decalvans are scarring alopecias that can mimic AGA in some cases. They generally have associated itching, burning or scalp tenderness. Some patients have all three symptoms and some have only two and some have no symptoms at all .
The other common mimicker of classic TE is seborrheic dermatitis and scalp psoriasis. These are common in the population so every hair specialist needs to know everything there is to know about scalp seborrheic dermatitis and scalp psoriasis because these are common concerns. . About 5-10 % of people have seborrheic dermatitis and 2-3 % of all people have psoriasis. In mild cases, seborrheic dermatitis and psoriasis don’t give much in the way of shedding. In moderate to severe cases, they most certainly do. These can mimic a telogen effluvium.
Conclusion
Thanks again for your great question. I hope this helped.
In summary, it’s likely your shedding is abnormal but it could be temporary. A full exam together with review of your story and completion of some key blood tests would be part of an ideal plan. Taking photos every 3 months is probably the most helpful thing you can do for yourself. If your shedding settles but density seems to be dropping off it’s likely there is some AGA present and starting one of the treatments is a good idea if your goal is to halt hair loss. If your shedding stabilizes in the next few months and density stays high, watchful waiting is probably the way to go. This later situation probably means you had some form of telogen effluvium.