Patients with Alopecia Totalis and Alopecia Universalis May Have Greater Risk of A Variety of Medical Issues
New Study Shows Heart Disease, Cancer, Blood Clots and Infections Are More Likely in Patients with AT/AU than Less Severe AA Forms.
In studies to date, it has not entirely been clear if alopecia is associated with an increased risk of certain adverse events like infection, cardiovascular disease, malignancy, and thromboembolism. Data has been inconsistent although the trend has been towards accepting that alopecia areata is associated with an increased risk of metabolic syndrome and heart disease.
In the past, we reviewed a nice 2021 study by Schneeweiss and colleagues which suggested that alopecia areata was not associated with an increased risk for blood clots.
It does seem that drugs that treat AA may be associated with an increased risk of some issues but perhaps not all of them. For example, JAK inhibitors may increase the risk of herpes zoster and herpes simples. Ongoing studies are looking at whether these medications may be associated with a higher risk of some adverse events cardiovascular disease, malignancy, and thromboembolism. As such, understanding the general baseline risk of these outcomes in a population with the disease is important .
George et al 2023
A new study set out to evaluate the risk of a variety of medical issues in patients with alopecia areata and how this compared to the risk in the general population. The researchers sought to understand not only how risk compares in patients with alopecia areata as a general group but also how risk compared in those with less severe forms and more severe forms.
The study was a retrospective cohort study that used medical and pharmaceutical claims from US administrative claims data in the Optum Clinformatics Data Mart database from 1 October 2016 to 30 September 2020.
Patients studied in the database were 12 years or older. Patients without AA were age-, sex-, and race-matched 3:1 to patients with AA. Baseline comorbidities were evaluated during the 12-month period pre-index date. Incident cases of serious/herpes infections, malignancies, major adverse cardiovascular events (MACE), and thromboembolic events were evaluated post-index date.
RESULTS
In total, 17,943,723 patients were in the database. There were 8,784 patients with AA (6.8% AT/AU n = 599, 93.2% non-AT/AU, n = 8185) matched to 26,352 patients without AA. The mean age of the study population was 45.6 years, and 55.6% were female. A total of 59.2% of patients were White, 20.3% were Hispanic, 10.2% were Black, and 10.2% were Asian. The mean age for patients with AA in the AT/AU group was 53.3 years and non-AT/AU subtypes was 45.0 years was 53.3 and 45.0 years, respectively.
AA VS NON AA: Are patients with alopecia areata more likely to have certain types of medical conditions?
The authors calculated incidence rates per 1000 person years among the AA and non AA cohort in order to determine if issues like infections with herpes simplex, herpes zoster, cancer, major adverse cardiac events and venous thromboembolism were any different in patients with alopecia areata compared to controls.
IRs per 1000 person-years among the AA and non-AA cohorts, respectively, were 18.5 and 20.6 for serious infections, 19.5 and 9.7 for herpes simplex infections, 7.8 and 7.6 for herpes zoster infections, 12.5 and 11.6 for primary malignancies, 16.0 and 18.1 for MACE, and 4.9 and 6.1 for venous thromboembolism. The authors concluded that it was really only the risk of herpes simplex that stood out as being more likely to occur more often in patients with alopecia areata.
AT/AU vs Milder AA Types: How do these compare?
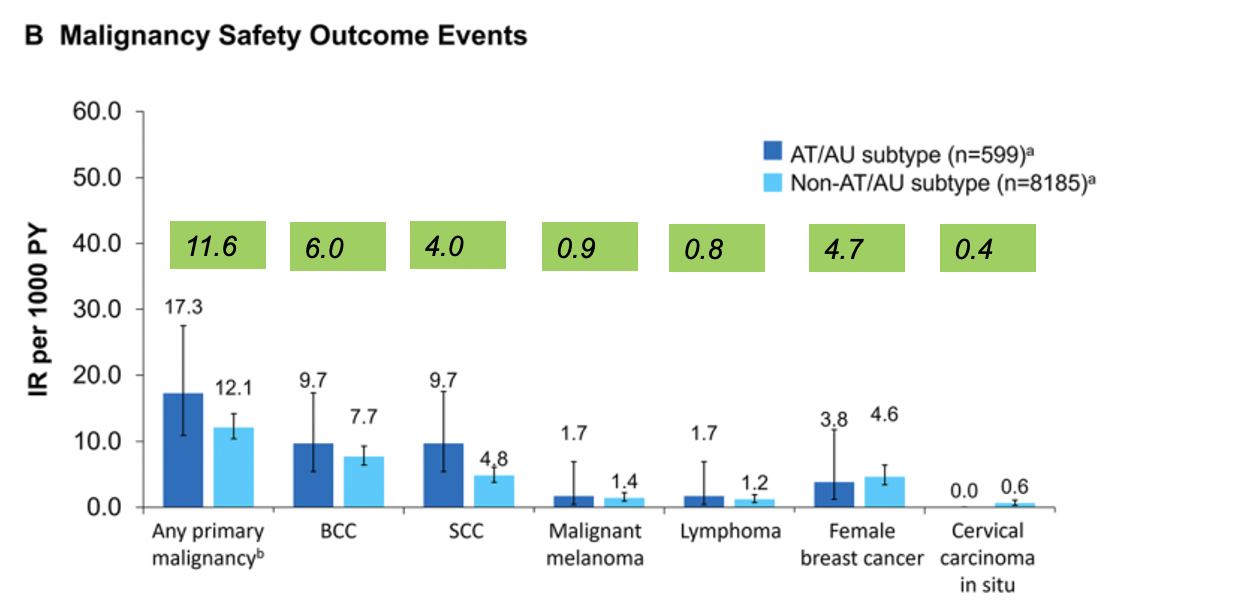
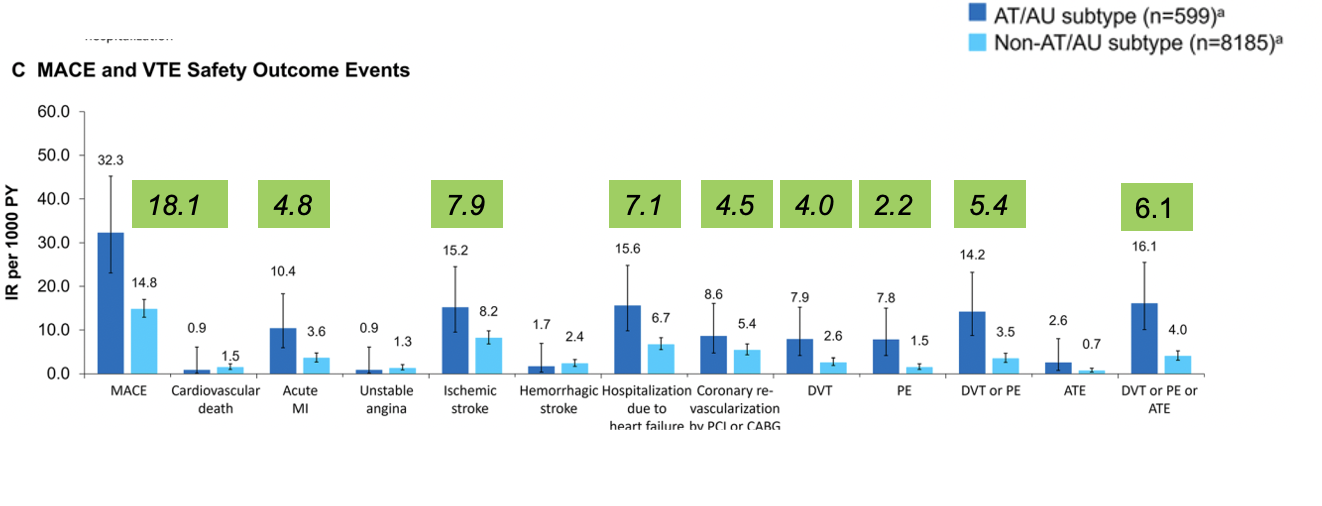
Generally, patients with AT/AU had higher IRs of events compared with patients with non-AT/AU AA, including serious infection requiring hospitalization, HZ infection, herpes simplex infection, any primary malignancy (except female breast cancer or cervical carcinoma in situ), BCC, SCC, malignant melanoma lymphoma, MACE, acute MI, ischemic stroke, hospitalization due to heart failure, coronary revascularization by PCI or CABG, any thromboembolic event, and all-cause death.
Compared to patients with non-AT/AU AA, patients with AT/AU largely had higher IRs for most baseline comorbidities and outcome events evaluated.
Comparison of infection rates in patients with milder alopecia areata (light blue) compared to alopecia totalis and universalis (dark blue). Green boxes are not part of the original figure and are Dr Donovan’s notations showing incidence rate in the general population. This figure shows that patients with alopecia totalis and universalis have a higher rate of serious infections, herpes zoster and herpes simplex compared to patients with mild AA and compared to the general population. FROM: George P et al. Incidence Rates of Infections, Malignancies, Thromboembolism, and Cardiovascular Events in an Alopecia Areata Cohort from a US Claims Database., Dermatol Ther (Heidelb). 2023 Aug; 13(8): 1733–1746. Image used with creative commons license.
Comparison of cancer incidence rates in patients with milder alopecia areata (light blue) compared to alopecia totalis and universalis (dark blue). Green boxes are not part of the original figure and are Dr Donovan’s notations showing incidence rate in the general population. This figure shows that patients with alopecia totalis and universalis have a higher rate of non-melonoma skin cancer, melanoma, and lymphoma compared to patients with mild AA and compared to the general population. FROM: George P et al. Incidence Rates of Infections, Malignancies, Thromboembolism, and Cardiovascular Events in an Alopecia Areata Cohort from a US Claims Database., Dermatol Ther (Heidelb). 2023 Aug; 13(8): 1733–1746. Image used with creative commons license.
Comparison of Major Adverse Cardiac Events and Venous Thromboembolism incidence rates in patients with milder alopecia areata (light blue) compared to alopecia totalis and universalis (dark blue). Green boxes are not part of the original figure and are Dr Donovan’s notations showing incidence rate in the general population. This figure shows that patients with alopecia totalis and universalis have a higher rate of major adverse cardiac events, heart failure, stoke venous thrombembolism compared to patients with mild AA and compared to the general population. George P et al. Incidence Rates of Infections, Malignancies, Thromboembolism, and Cardiovascular Events in an Alopecia Areata Cohort from a US Claims Database., Dermatol Ther (Heidelb). 2023 Aug; 13(8): 1733–1746. Image used with creative commons license.
COMMENTS
Compared with those in the matched non-AA cohort, patients with AA had similar IRs for components of most studies issue cardiovascular disease, malignancy, and thromboembolism. The major exception was that patients with AA had a greater incidence of herpes simplex infection than those in the matched non-AA cohort.
Higher rates of herpes simplex infection in patients with AA may be due to a higher baseline usage of immunosuppressants.
What was so interesting in this study is that patients with AT/AU had a higher incidence of baseline comorbidities, risk factors, and outcome events than patients with non-AT/AU AA, There were a total of 599 AT/AU patients examined in this study!
What do we do with this information?
More studies are needed to better understand these baseline risks and how we should best care for patients with AT/AU. Is more screening required? Should we have more aggressive treatment cut offs for cholesterol, blood pressure? If patients with AT/AU are at increased risk for blood clots, should we be using oral contraceptives?
Are you a lumper or a splitter?
This is a really important study. On one had there is a major push in our field to stop dividing and subdividing AA into all the different forms. There is a major push to lump rather than split.
I am a splitter.
The reality is that – in my opinion – we are not ready to lump yet.
We still have a long ways to go to the finish line for alopecia areata. JAK inhibitors are great but they help only a small proportion of patients get all their hair back and unfortunately many patients ( at least 10%) seem to lose their nice results in year 2.
So it does not seem like we are really ready to lump all alopecia areata together. It seems pretty clear that AT and AU are very different. They have a unique set of comorbidities. It seems like we do need to have the alarm bells on in room 5 when we meet a patient with AT or AU. It does seem like outside the door of room 8 there needs to be a flashing light reminding us that the patient we are about to see has AT and AU.
How else are we going to pay attention to the fact that these patients seem to have a higher risk of cancer, heart disease, some infection and blood clots.
If we lump all alopecia together, we are prompted to feel that their risks are the same as anyone else. If we decide to reject that concept of being lumpers and instead be splitters, we realize that AT and AU come with very different risk than mild AA.
I think we owe it to our patients to be splitters. I think we owe it to our patients to see something very special and unique in a patient with AT and AU and make sure that we are doing everything we can to address heart disease, cancer, blood clots and infection.
REFERENCE
George P et al. Incidence Rates of Infections, Malignancies, Thromboembolism, and Cardiovascular Events in an Alopecia Areata Cohort from a US Claims Database., Dermatol Ther (Heidelb). 2023 Aug; 13(8): 1733–1746.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.