Childhood Onset and Adolescent onset Androgenetic Alopecia (AO-AGA): Key Lessons
What you need to know about childhood and adolescent onset androgenetic alopecia.
Early onset androgenetic alopecia refers to androgenetic hair loss occurring before age 30. For males, androgenetic alopecia is commonly referred to as male balding. For females, we commonly refer to the process by the term female pattern hair loss.
Androgenetic alopecia does not typically occur in teenagers. However, 0.5 % to 2 % of senior high school students may have sings of thinning.
Childhood onset AGA and adolescent onset AGA (AO-AGA) are a special subtype of early onset AGA that requires special attention. Childhood onset AGA is a term that refers to AGA starting before puberty and adolescent onset AGA is a term to refer to androgenetic alopecia starting after puberty but prior to age 18. The exact prevalence is not clear but it’s likely that 0.5 to 2 % of high school students shown signs of androgenetic alopecia. Androgenetic alopecia can occur as young as 6-8 years albeit this early age of onset is very uncommon. The average age is usually 13-15 years. A study by Gonzalez et al showed that about 1 in 6 adolescents with early onset AGA had thinning before age 12. A 2010 survey by Trancik et al of 84 physicians who provided data on 448 adolescents with early onset androgenetic alopecia ( 341 boys and 107 girls), hair loss began between ages 7 and 17 years. The mean age at onset of 14.8 years in boys and 13.8 years in girls.
The general features of adolescent AGA are similar to adult onset AGA, namely the ‘miniaturization’ of hair follicles. Males tend to have a higher incidence of central hair loss as opposed to typical hair loss occurring in the temples and the crown area. Among 38 boys with early balding, Gonzalez et al (2010) showed that 47 % had thinning in the vertex and temporal areas, 34 % had diffuse thinning including the crown, 11 % had vertex only and 8 % had frontal only pattern. Among 19 girls with early androgenetic alopecia, 42 % had diffuse thinning, 42 % had thinning at the crown at 8 % had frontal thinning only.
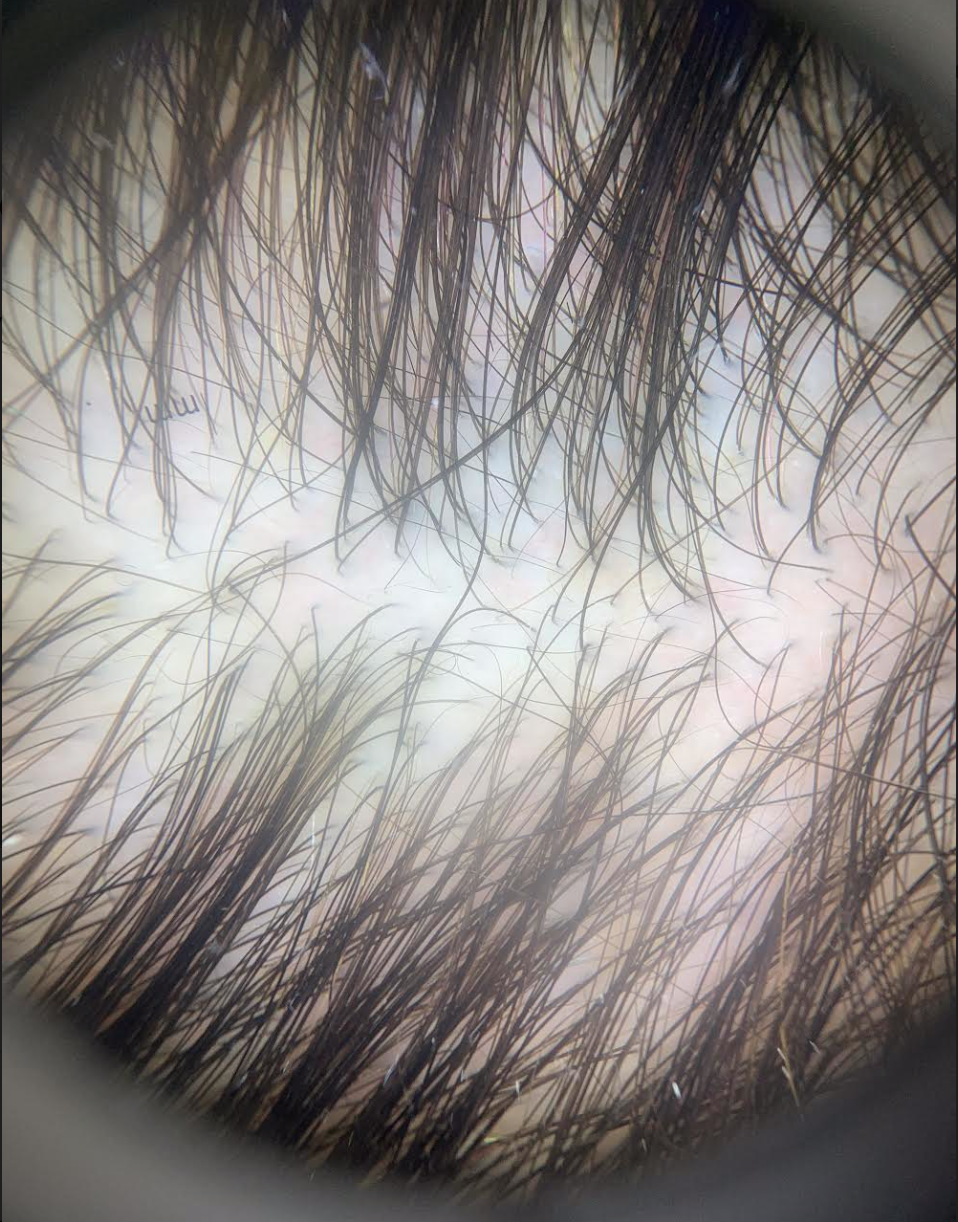
Trichoscopy of early onset androgenetic alopecia. A variation in the thickness of hair follicles can be clearly seen.
Family History
A family history of thinning may be present in some but not all cases. The 2010 study by Trancik et al showed that a family history is usually present but the absence of a family history does not rule out early onset AGA. Adolescents with AGA in the Trancik study had a family history of AGA on either on the father’s side or the mother’s side, or on both sides. Among males with early balding, 73 % had a family history of androgenetic alopecia in male family members and 38 % had a family history in female family members. Among females males, 57 % had a family history of androgenetic alopecia in male family members and 57 % had a family history in female family member.
Systemic Issues for Patients with Early Onset AGA
A number of systemic (whole body) issues can be associated with early androgenetic alopecia and these need to be ruled out. These include congenital adrenal hyperplasia (CAH) and metabolic dysfunction, insulin resistance, hypertension. Gonzalez et al showed that 1 out of 25 males adolescents with early onset balding had late onset CAH. A high proportion of females with early onset AGA have PCOS. In fact, elevated androgens were identified in 6 of 16 girls (38 %) with early onset hair loss and a diagnosis of PCOS was felt to be likely in all 6 patients. S
See
Evaluating the Patient with PCOS: What Labs are Needed?
Late Onset Congenital Adrenal Hyperplasia
Blood tests To Consider
Blood tests should be ordered according to the patient’s history. Generally, tests for androgen excess are front and center including testosterone and DHEAS. Other tests to consider include cholesterol, glucose, hemoglobin A1c, estradiol, 17 hydroxyprogesterone, AM cortisol, prolactin, TSH, LH and FSH. Gonzalez et al showed that hyperandrogenism was present in 14 % of 14 boys, mainly as elevated DHEAS and one had late onset congenital adrenal hyperplasia. Where possible, blood tests for females should be performed on day 3-5 of the cycle.
Scalp Biopsies
Biopsies are not typically necessary although if one does choose to biopsy the scalp it must be interpreted by an expert as erroneous diagnoses of lichen planopilaris are possible - and common!. Gonzalez et a showed that 57 % of biopsies of early onset AGA also had varying degrees of a peri-infundibular lymphocytic inflammatory infiltrate and fibrosis which is a findings also present in the autoimmune condition known as lichen planopilaris. In fact, in early one quarter of biopsies, the diagnosis of lichen planopilaris was strongly considered. Expert dermatopathologists will take note of the preservation of sebaceous glands in AGA, the absence of lichenoid change of the outer root sheath in AGA and the preservation of the elastic network in AGA if special stains like Verhoeff van Gieson are used. I commonly see misdiagnoses of ‘lichen planopilaris” in young patients whose biopsy reports return with these words. Of course, some young patients can have LPP but many times, the diagnosis is wrong.
Treatments for Childhood and Adolescent Onset AGA
The treatments for adolescent AGA in males is slightly different than for adults given that we place greater emphasis on the use of minoxidil and less emphasis on the use of anti androgens in those under 18. To date, there are no formally “FDA approved” treatments for those under 18 years. That is not to say that there are no treatments simply that no company has submitted data to Health Canada or the FDA to have their product specifically approved for adolescents
In the absence of an underlying endocrine issue, minoxidil remains the first line option for treating adolescent AGA. In 2001, Trancik et al reported finings of 448 adolescents with androgenetic alopecia who were treated with minoxidil for 18 months. For the 341 males using minoxidil, 55 % had improvement in hair density and 41 % had a slowing of thinning. For the 107 females using minoxidil, 51 % had improvement in hair density and 44 % had a slowing of thinning. In a second 2010 study by Gonzalez et al, 4 of 6 girls (67%) and 18 of 23 boys (78%) who were treated with 5% minoxidil for more than 6 months had a stabilization of their hair loss.
Minoxidil appears to be safe in those under 18. In fact, an open-label investigation of 13 boys, aged 13 to 17 years (mean age, 15.9 years), with early male balding confirmed this safety. Participants applied 1 mL of minoxidil topical solution 5% to the area of thinning hair every morning and evening for one week minoxidil topical solution did not alter pulse rate, blood pressure, or other vital signs.
Other options for treating early balding include low level laser. The use of finasteride in males has not been formally studied under 18 and is not typically started until 17-18. Spironolactone and oral contraceptives may be considered in some females especially if PCOS or CAH is an associated diagnosis.
Guidelines for Monitoring the Patient with Chilldhood and Adolescent Onset AGA
We do not yet have screening guidelines in the world for how best to monitor males and females with chilldhood onset AGA and adolescent onset AGA. We know confidently that males and females with early onset androgenetic alopecia have an increased risk of developing metabolic syndrome and cardiovascular disease later in life. I feel strongly that our medical community has neglected this issue but nevertheless we have guidelines in our clinic that we feel are appropriate first steps. In our clinic, we recommend the following:
1. Encouragement of healthy eating and diets rich in antioxidant rich fruits and vegetables.
2. Encouragement of active lifestyles with 300 minutes of physical exercise weekly.
3. Smoking cessation strategies for all smokers and guidance to not begin smoking.
4. Blood pressure measurements at baseline and then yearly by the pediatrician or family physician. Treatment of hypertension with lifestyle and pharmacological means as recommended by current evidence based guidelines
5. Cholesterol levels at baseline and then every 3-5 years. Aggressive treatment of abnormal cholesterol level according to current evidence based guidelines.
6. Fasting glucose insulin and hemoglobin A1c levels at baseline and every 3-5 years.
7. Weight and height measurements yearly and evidence based weight reduction strategies if weight rises into the overweight or obese ranges
Conclusions and Summary
Adolescent onset AGA is not common but carries significant psychological impact on teenagers. Getting a proper diagnosis is essential followed by initiation of treatment. In most cases, minoxidil will be an important first line consideration. Other options may be possible too. For males and females, it’s important to exclude an underlying endocrinopathy - especially PCOS in females.
References
Gonzalez ME et al. Br J Dermatol 2010.
Trancik RJ, et al Clinician survey evaluating minoxidil topical solution in the treatment of androgenetic alopecia in patients under 18 years of age. Poster presented at: 3rd Intercontinental Meeting of the Hair Research Societies; June 13-15, 2001; Tokyo, Japan. P129.
Trancik RJ et al. Investigation of the systemic bioavailability of 5% minoxidil topical solution in young males with early androgenetic alopecia. Poster presented at: 3rd Intercontinental Meeting of the Hair Research Societies; June 13-15, 2001; Tokyo, Japan. P126.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.