Does a scalp biopsy capture all diagnoses a patient has?
Biopsies answer key questions - but not all questions!
Scalp biopsies are wonderful tools when used properly. When not used properly they have the potential to create enormous confusion.
A scalp biopsy does not always capture all the diagnoses that the patient has. First, it depends where on the scalp the biopsy is taken from and second what exactly the diagnosis is.
Example
Let’s suppose a 43 year old female patient has what appears to be a scarring alopecia affecting her crown (i.e. the top of the scalp). She is quite concerned about hair loss in this area and pulls her hair back tightly into a pony tail in order that the crown hair loss can be hidden. She is also shedding much more than normal which she thinks is due to her recent diet which allowed her to lose 70 pounds in 4.5 months.
You examine her scalp and notice she has traction alopecia. In addition to the traction alopecia, you notice she has some female pattern hair loss (androgenetic alopecia) affecting the front one-third of the scalp. Blood tests show TSH 17.55.
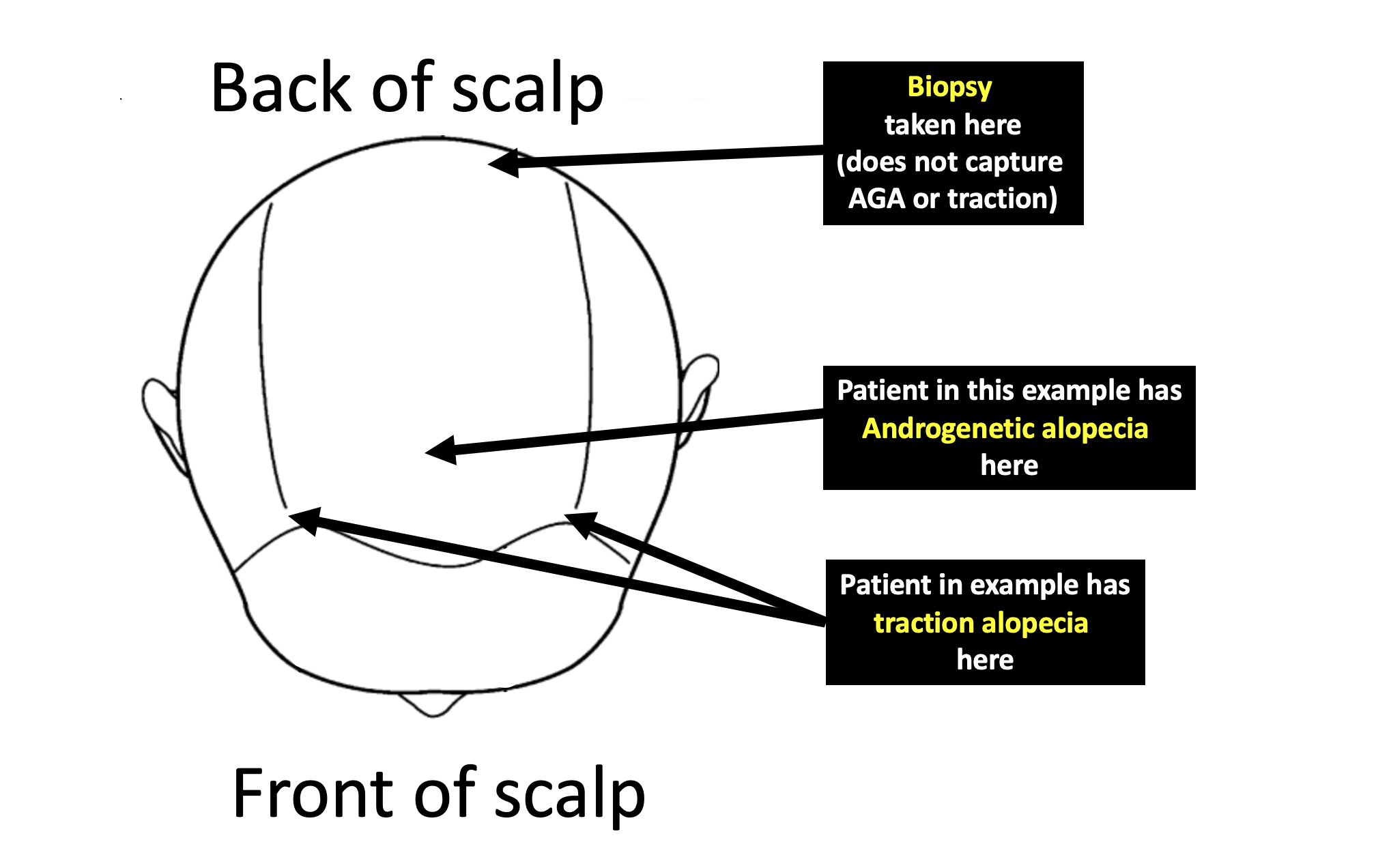
You now proceed to biopsy the crown. The biopsy returns showing evidence of folliculitis decalvans- a type of scarring alopecia. You look carefully to see if the pathologist reports anything about androgenetic alopecia and anything about traction alopecia and you are disappointed to see that you can’t find anything about these diagnoses.
So does she have androgenetic alopecia? Does she have traction alopecia ? That answer is yes! In fact, she also has a telogen effluvium (hair shedding disorder) from hypothyroidism as well as from her diet. The biopsy however captures mainly the folliculitis decalvans.
The site of the biopsy in the crown does not overlap with the area on the scalp that is affected by androgenetic alopecia and also does not overlap with the area affected by traction alopecia.
In addition, the biopsy contains mostly scar tissue and a few residual hairs. It’s possible for the pathologist to get an accurate assessment of the overall type of hair loss (ie. scarring vs non-scarring) but there is simply not enough hairs to comment on hair cycle parameters (ie a possible telogen effluvium). The diagnosis of telogen effluvium must come from the clinical history as well as from the scalp examination.
Conclusion
Biopsies are great diagnostic tools when employed properly. They aren't the final step in nailing down the diagnosis. If a doctor is going to perform a biopsy, he or she ideally needs to write down all the questions her or she is hoping to uncover by doing the biopsy. Before consenting the patient and before putting in the freezing to anesthetize the scalp, the physician needs to step back and ask again “does the biopsy I am about to do allow me to answer these questions?” If not, choose a different spot or choose another spot or choose a different diagnostic tool (blood tests, hair collections, etc). Biopsies are wonderful tools in the right situation and a great source of confusion when used in the wrong context.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.