Diagnosis and Treatment of Cutis Verticis Gyrata (CVG)
Cutis verticis gyrata: What is CVG? What are the options for treatment?
What is CVG? How common is CVG?
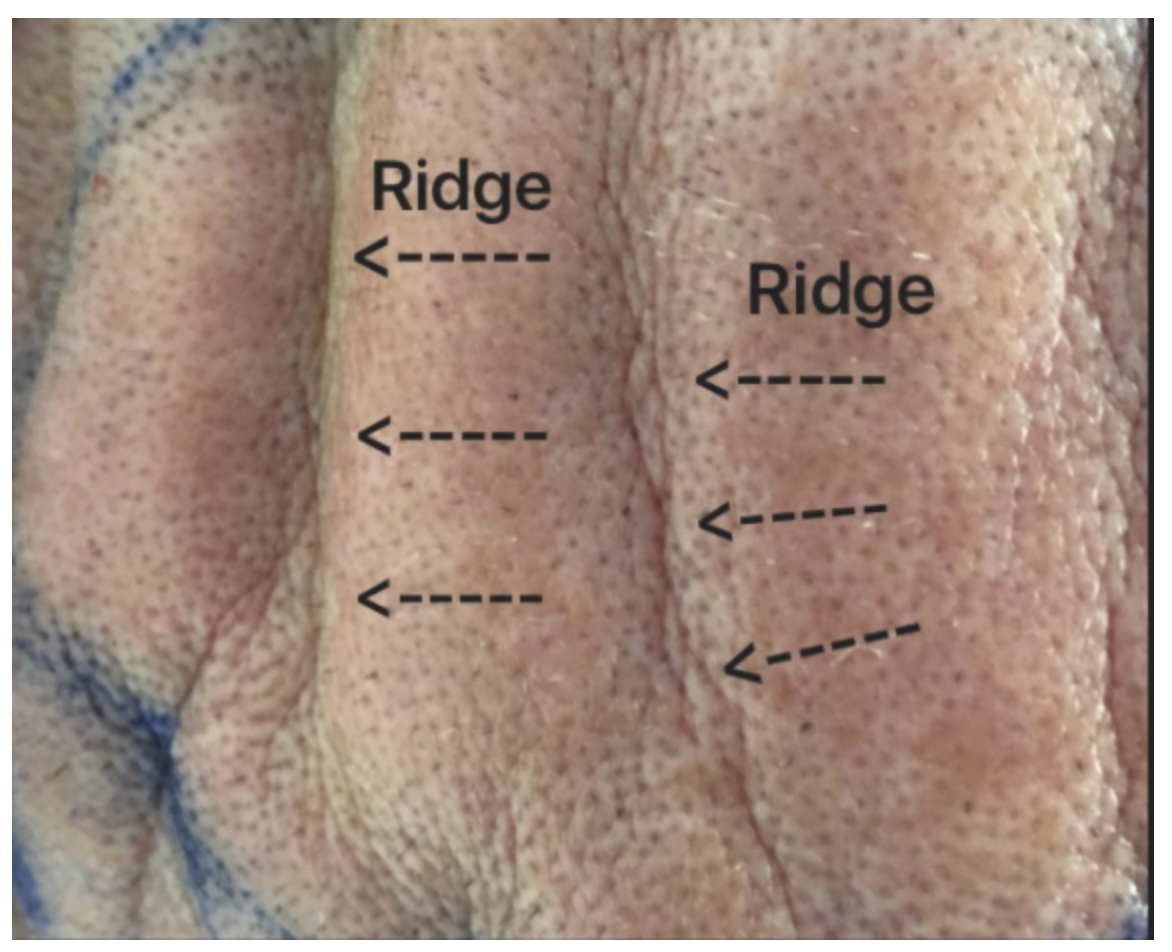
Cutis verticis gyrata (CVG) is a scalp condition whereby the affected individual develops folds and furrows in the scalp that resemble the appearance of the brain’s cerebral cortex (gyri). Cutis verticis gyrata was first described in the mid 1800s. The condition is estimated to affect about 1 in 100,000 men and 1 in 400,000 women. A photo of the folds and furrows from a patient with CVG is shown below.
Photo of a patient with cutis verticis gyrata
What is the cause of cutis verticis gyrata?
The cause of CVG is often not known. Given that primary forms often occur after puberty, it is often thought that hormonal and endocrine issues play a role in the development of the condition.
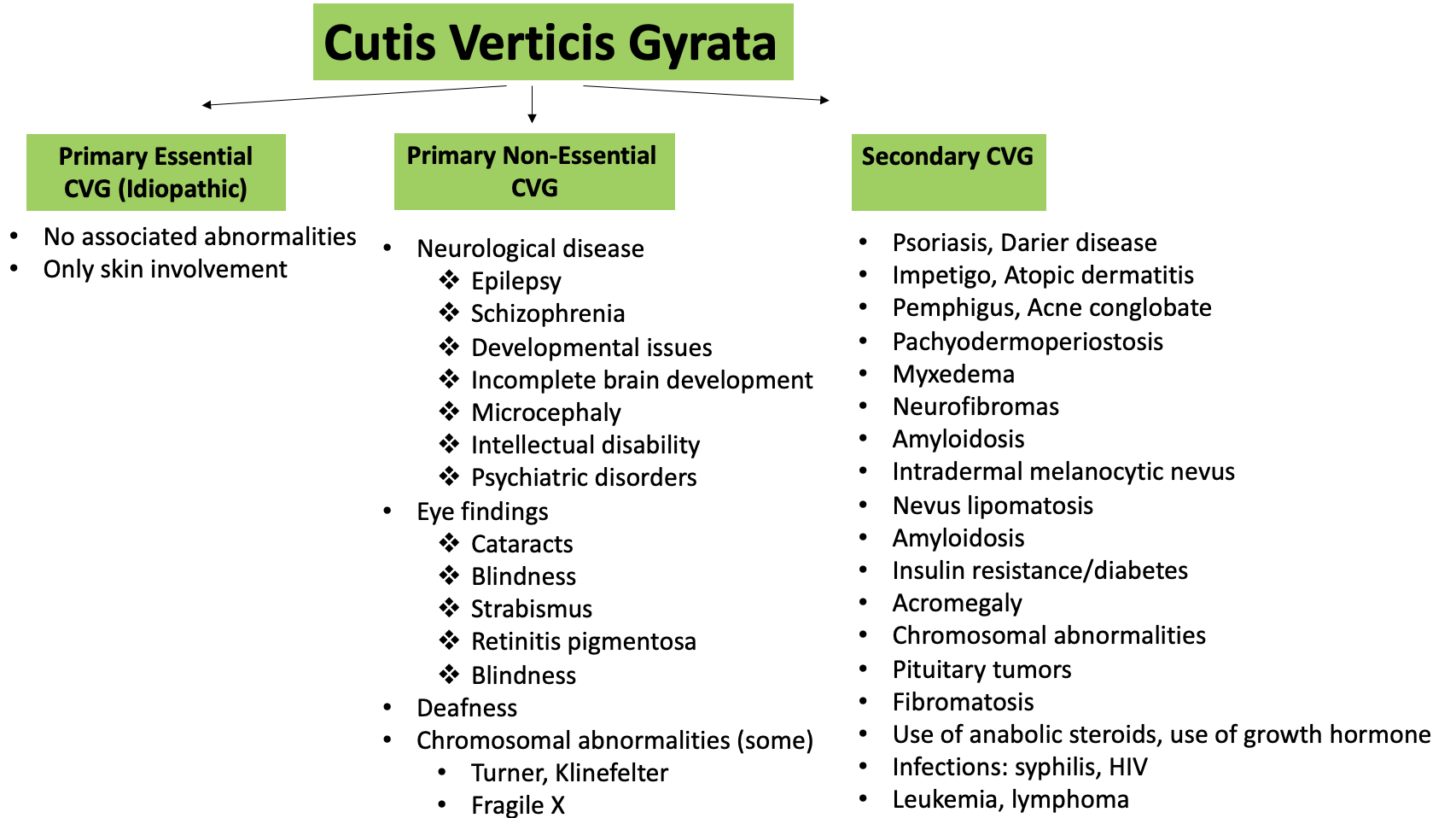
We divide CVG into three groups according to associated conditions and potential causes.
a) Primary Essential CVG
For many patients with CVG, there is no clear underlying cause and no abnormalities can be found. These patients are said to have “primary essential CVG.” Affected patients are usually male and develop CVG during or after puberty. The folds and ridges are usually distributed in a symmetrical manner and the vertex and the occipital region is commonly affected. Folds in primary CVG typically run in the antero-posterior direction. Patients do not have any type of underlying eye disease or neurological disease.
b) Primary Non-Essential CVG
This is the more common type of primary CVG. In primary non-essential CVG there are underlying abnormalities. These are typically neurological and ophthalmologic in nature, but hearing may sometimes be affected too. These abnormalities themselves don’t actually contribute to the folds of the scalp. They are simply important associations that also need separate investigation. In other words, treatment of the neurological or eye abnormalities will not lead to changes or improvement in the furrows and grooves on the scalp.
Chromosomal abnormalities contribute to some forms of primary non-essential CVG. Examples include fragile x syndrome, Turner and Klinefelter’s Syndrome
Folds in primary CVG typically run in the antero-posterior direction.
Most cases of primary CVG occur before age 30 and have a striking male predominance. As mentioned, primary non-essential CVG is more common than primary essential CVG. One must given strong consideration to evaluating for underlying neurological or eye disorders.
c) Secondary CVG
In so called “secondary” CVG, the patient may have one or more underlying abnormalities and these abnormalities directly contribute to the folds and furrows seen on the scalp. Unlike primary CVG, a scalp biopsy of secondary CVG often (but not always) shows features of specific underlying condition. Furthermore, treatment of the underlying condition may improve the condition of the scalp in some situations. Therefore, carefully ruling out secondary CVG is an important goal for anyone presenting with CVG.
Secondary forms occur at any age and in both male and females. When CVG occurs in children or at birth one needs to consider these secondary forms. Most forms of primary CVG don’t occur this early in life. CVG occurring a birth is often associated with a cerebriform intradermal nevus or a genetic syndrome.
Although folds in primary CVG typically run in the antero-posterior direction, folds in secondary CVG will be directed according to the underlying disorder.
Common underlying abnormalities in primary and secondary CVG are shown in the diagram below. We often refer to this as the classification of CVG.
Evaluation and Work up of Patients with Cutis Verticis Gyrata
All patients with CVG should have a proper evaluation. That does not mean that all patients will require all the possible tests that can be done, but certainly all patients should have their history reviewed by a physician knowledgeable about primary and secondary CVG and all patients should have a properly conducted scalp examination. Most patients will benefit from blood tests although the array of blood tests that are appropriate to order will depend on the patient. Consideration is given to scalp biopsies, MRI, CT and ophthalmology referral and neurology referral on a case by case basis.
a) Obtaining a history
It is important to obtain a proper history. This history will be important to help the clinician further determine whether the CVG could be primary or secondary.
It is important to assess for an array of symptoms related to neurological disease, eye symptoms, hearing, skin disease, infections, risk factors, diabetes, thyroid disease, medications, developmental and learning issues.
It is also important to determine if there are any scalp symptoms, such as itching or burning or pain/tenderness. Some patients have scalp odour due to overgrowth of bacteria in the furrows.
b) Scalp Examination
Scalp examination is important to rule out secondary causes that might be contributing to the CVG. Inflammatory and neoplastic skin diseases that contribute to secondary CVG can often be diagnosed with CVG.
In primary CVG, the folds are symmetrical and run front to back and usually involve the vertex and occiput. Secondary CVG can resemble primary CVG perfectly but may involve the entire scalp rather than favoring the vertex and occiput. There may be just a few folds or upwards of 20-30. The folds do not flatten when pressure is applied.
c) Blood tests
Blood tests are important to consider in all patients with CVG. Not all patients require extensive work ups but a variety of tests should be considered. These include;
a) CBC, TSH, glucose, hemoglobin A1c, creatinine, AST, ALT (usually ordered)
b) Consideration can be given to order LH, FSH, testosterone, PTH, RPR, HIV, SPEP, IGF-1, prolactin, AM cortisol
d) Scalp Biopsy
A scalp biopsy is often not required but can be helpful in more challenging cases of suspected secondary CVG. CVG starting in the teens or 20s with folds and furrows that run front to back is often due to primary CVG and may not require a biopsy. If there is a history of neurological or eye issues, a diagnosis of primary non-essential CVG is given but also may not require biopsy in many cases.
However, patients with early onset CVG, late onset CVG, symptomatic CVG, those with systemic symptoms, and those with unusual patterns of furrows and fold should have full evaluation to rule out secondary forms of CVG. A scalp biopsy is often helpful in these secondary CVG cases.
Histology typically shows hyperplasia and hypertrophy of epidermal appendages. Sebaceous glands are enlarged. Collagen bundles are thickened and there is increased matrix material in the dermis. In the secondary forms, biopsy may reveal clues to the underlying disorder.
e) Medical Imaging
CT exams and MRI examinations can be helpful to evaluate the diagnosis but is typically used for evaluating underlying neurological abnormalities that might be present. For example, pituitary abnormalities (pituitary adenoma) might be seen on MRI.
f) Ophthalmology Referral
A low threshold should be given to referring patients for eye examinations. I am of the opinion that most patients with CVG benefit from at least a one time eye screening. The most common form of primary CVG is primary non-essential CVG and eye abnormalities are common in these patients.
f) Referral to Other Specialists
Given the many associations with CVG, referral to other specialists may be appropriate. For example, there are important associations between some cases fo CVG and neurological disorders and therefore consultation with a neurologist may be advised if there are concerns about any type of neurological disorder (i.e. seizures). Consultation with an endocrinologist may be important if the CVG is felt to be secondary to an endocrine disorder (i.e. acromegaly, pituitary disorder, diabetes). Other referrals may be important. For example, referrals to a pediatric development specialist may be important if there is underlying neurodevelopmental issues.
Treatment fo CVG
Treatment of CVG will depend on whether the final diagnosis is primary or secondary CVG. In cases of secondary CVG, treatment of the underlying issue will often improve the appearance of the folds and furrows or potentially slow the progression of the CVG.
Attention to scalp hygiene is important for all patients, but especially important for those patients with current symptoms and signs of infection. Frequent shampooing and drying and attention to use of antibacterial cleansers can be helpful.
Not all patients require treatment. Many patients have milder forms of primary CVG and are not significantly bothered by the appearance and do not experience symptoms. A “watch and wait” approach may be appropriate for many patients who fit this description. Patients with more significant CVG or who are symptomatic or who feel their quality of life will be improved by addressing the CVG can consider treatment.
Surgery is an important treatment to consider. In fact, surgical treatment is still currently viewed as the mainstay of treatment for many patients with CVG. Skin is excised and edges brought together in order to create a flattened appearance. More extensive disease may require tissue expanders before excision. Surgery has variable effectiveness depending on the severity of the CVG.
Other treatments include use of fillers or fat grafting although good studies have not been done. A recent treatment, involving the use of hyaluronidase, appears to be a promising treatment.
References
Adôrno IF et al. Primary essential cutis verticis gyrata. Radiol Bras. 2019 Jul-Aug;52(4):276-277. doi: 10.1590/0100
MacGillivray RC. Cutis verticis gyrata and mental retardation. Scottish Medical Journal. 1967;12(12):450-454.
Schenato LK et al. Essential primary cutis verticis gyrata. J Pediatr (RiO J). 2002;78(1):75-80. 7.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.