Patients with Dystrophic Epidermolysis Bullosa At Increased Risk for Folliculitis Decalvans
New Link Identified Between Dystrophic Epidermolysis Bullosa and Folliculitis Decalvans
Authors of a new study report here 30 cases of the scarring alopecia known as Folliculitis Decalvans (FD) associated with dystrophic epidermolysis bullosa (DEB). Their data suggest a new link between these two rare diseases.
Authors reviewed the records of 243 patients with inherited EB seen between 2010 and 2021 in two French centres specializing in EB. The total numbers of patients with each subtype (number of patients over 15 years of age in parentheses) were: EB simplex (EBS) = 69 (37); junctional EB (JEB) = 31 (22); dominant dystrophic EB (DDEB) = 35 (29); and recessive dystrophic EB (RDEB) = 108 (96).
The risk of FD was highest in RDEB: FD was found in 27 of 96 (28%) adult patients with RDEB, 3 of 29 (10%) with DDEB. There were no cases of FD in patients with EBS or JEB. No prepubertal children had FD, and FD started at puberty or after in all patients for whom this information was available (n = 16).
All in all, the authors showed that 24% of patients (30 of 125) with DEB also had FD. Most patients were women.
Discussion.
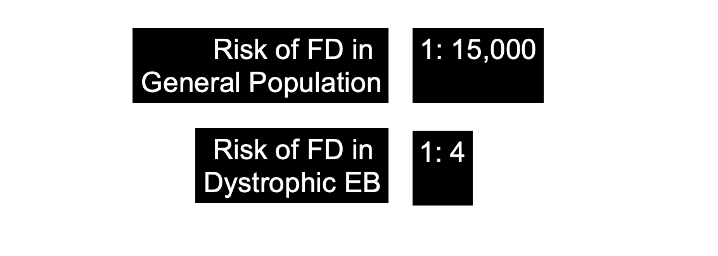
One quarter of patients with DEB had FD. This is an interesting link. It’s not clear why this is but it is dramatic. About 1 in 15,000 to 1:20,000 people in the general population have FD. This number seems to be 1:4 for those with Dystrophic EB
FD is more likely in female DEB patients. This is unexpected as DEB is equally common in males and females. Furthermore, FD tends to occur in males. So there is something unique here about female cases. The authors propose that perhaps mechanical stress due to some women’s habits of hairdressing with traction lead to this finding.
The authors also propose that perhaps there is some skin barrier defect in DEB that predisposes to FD. It is increasingly clear that FD is due to a disruption of the skin microbiome and the skin in DEB may have the changes in microbiome that facilitate FD.
More studies are needed to better understand this phenomenon and how nutrition, would care, and antimicrobial care might reduce the incidence of FD in patients with DEB.
A Brief Review of Epidermolysis bullosa (EB)
Epidermolysis bullosa (EB) is an inherited, rare genetic blistering disorder precipitated by mechanical stress. There are four major classes of EB based on level of tissue separation: EB simplex, junctional EB, dystrophic EB and Kindler syndrome
Dystrophic epidermolysis bullosa.
Dystrophic epidermolysis bullosa (DEB) is a genetic skin disorder affecting skin and nails that usually presents at birth. DEB accounts for 2–6 per million live births. The prevalence is similar in both sexes.
DEB is caused by mutation in type VII collagen, COL7A1. There are 14 subtypes of dystrophic epidermolysis bullosa and 400 mutations of COL7A1
In mild cases, blistering may primarily affect the hands, feet, knees, and elbows. Severe cases often involve widespread blistering that can lead to vision loss, disfigurement, and other serious medical problems.
Recessive Dystrophic EB (RDEB)
Recessive dystrophic epidermolysis bullosa (RDEB) ischaracterized by skin fragility leading to blistering, wounds, and scarring. The main findings in severe generalized RDEB include skin fragility. The patient has blistering with minimal trauma and this heals with milia and scarring. Blistering and erosions affecting the whole body may be present in the neonatal period. Oral involvement may lead to mouth blistering, fusion of the tongue to the floor of the mouth, and progressive reduction of the size of the oral cavity. Esophageal erosions can lead to webs and strictures that can cause severe difficulty swallowing food (dysphagia). Consequently, malnutrition and vitamin and mineral deficiency may lead to severe growth restriction in childhood.
The eyes can be affected too. Specifically, corneal erosions can lead to scarring and loss of vision.
Blistering of the hands and feet followed by scarring fuses the digits into "mitten" hands and feet, with contractures and pseudosyndactyly. Most patients develop skin cancer: The lifetime risk of aggressive squamous cell carcinoma is above 90%.
In contrast, the blistering in the less severe forms of RDEB may be localized to hands, feet, knees, and elbows with or without involvement of flexural areas and the trunk, and without the mutilating scarring seen in severe generalized RDEB.
Dominant Dystrophic EB (DDEB)
In DDEB, blistering is often mild and limited to hands, feet, knees, and elbows, but nonetheless heals with scarring. Dystrophic nails, especially toenails, are common and may be the only manifestation of DDEB.
When should one suspect DEB?
Dystrophic epidermolysis bullosa (DEB) should be suspected in individuals with the following clinical findings:
· Fragility of the skin, manifest by blistering with minimal trauma that heals with milia and scarring
· Blistering and erosions
· Dystrophic or absent nails, especially toenails
· Family history consistent with either an autosomal recessive or an autosomal dominant inheritance
CONFIRMING THE DIAGNOSIS VIA GENETIC TESTING
DEB is caused by changes in the COL7A1 gene. Genetic testing can confirm this diagnosis.
A patient with dystrophic EB. There are multiple vesicles and bullae with erosions and hemorrhagic crusts present There are also hypopigmented and atrophic areas of previously healed lesions. FROM: Randhir Sagar Yadav et al. Dystrophic Epidermolysis Bullosa . JNMA J Nepal Med Assoc. 2018 Sep-Oct; 56(213): 879–882. Published online 2018 Oct 31
Treatment of DEB
There is no specific treatment of ED. Symptomatic management remains mainstay of treatment. This include reducing trauma and treating wounds. Nutritional support with prevention of complications like skin infection, scar formation, skin cancers is key. Psychological support is also very important.
REFERENCE
Matard B et al. Folliculitis decalvans and dystrophic epidermolysis bullosa: a significant association. Br J Dermatol . 2022 Dec;187(6):1026-1028.
Randhir Sagar Yadav et al. Dystrophic Epidermolysis Bullosa . JNMA J Nepal Med Assoc. 2018 Sep-Oct; 56(213): 879–882. Published online 2018 Oct 31
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.