Which patient with discoid lupus erythematosus (DLE) is most likely to develop severe SLE?
Patients with DLE Who are Young, Darker Skin Types and Have High ANA are Most Likely to Progress to Severe SLE
Introduction
Discoid lupus erythematosus (DLE) is a form of chronic cutaneous lupus. Some patients have involvement of the facial skin and some have scalp involvement. It can cause scarring alopecia. Some patients with DLE can go on to develop systemic lupus erythematosus. Some of the patients with SLE will have mild disease but some will have a severe SLE form (sSLE) which can affect multiple organs of the body.
At the time of diagnosis of DLE, most patients with DLE do not have any evidence of SLE. Some patients, however, will go on to develop SLE over time. Studies have suggested that the risk of progression from DLE to SLE ranges from 6% to 21% depending on the study. More recent studies using the newer criteria have put the number around 3% and 11%.
Some studies have outlined criteria that increase the chance that a person with DLE will go on to develop SLE. These include widespread DLE lesions, arthralgia, nail changes, anemia, leucopenia, high erythrocyte sedimentation rates, and high titers of antinuclear antibodies (ANA).
The main issue with the definition of lupus is that some patient can meet criteria for lupus but have very mild disease and never require treatment. What matters most is what proportion of patients with DLE will develop severe SLE. A 2014 study by Wieczorek et al showed that only 5 of 74 patients (7%) with CLE developed moderate or severe SLE.
Fredeau L et al 2023
Authors of a new study set out to determine risk factors for patients to progress from discoid lupus erythematosus (DLE) to severe systemic lupus erythematosus (sSLE)
In this study there were a few definitions.
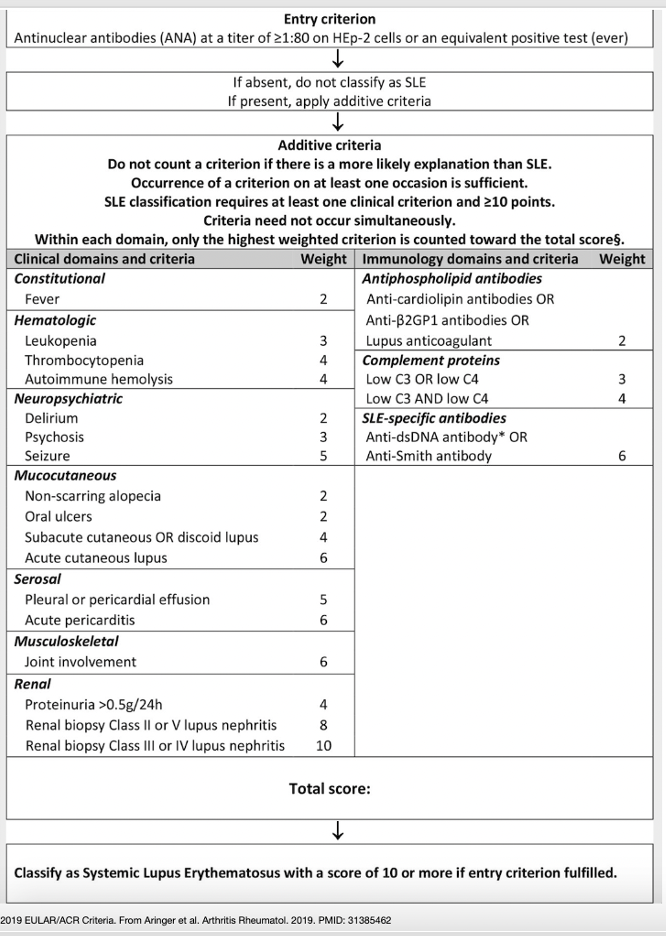
DLE with mild biological SLE was defined by the presence of at least 10 points using the 2019 ACR/EULAR Criteria with DLE as the only clinical feature but associated with the presence of biological abnormalities, including leucopenia, decreased C3 and/or C4 levels, and presence of specific autoantibodies, with no specific treatments regarding these abnormalities
Severe SLE was defined as follows: (1) by the occurrence of at least 1 of the following features: SLE fever, serositis (pericarditis or pleural effusion), lupus nephritis, neuropsychiatric manifestation, autoimmune hemolysis, or autoimmune thrombocytopenia and (2) the need for a specific treatment with systemic corticosteroids ([0.5 mg/kg), immunosuppressant drug, and/or hospitalization related to SLE.
Fredeau L et al 2023 Study
Patients were included in the study if they had DLE with pathologic confirmation or had DLE or mild biological SLE at the time of diagnosis. Patients with severe SLE were excluded.
At baseline, 86 (52%) patients were classified as having DLE only and 78 (48%) patients were classified as having DLE associated with mild biological SLE.
In total, the study included 30 patients with DLE who developed sSLE and 134 patients who did not. Patients were women (81%), and the median age at the time of DLE diagnosis was 33 years (range, 9-79 years). The median follow-up duration was 12.14 years (range, 2.64-48.56 years).
RISK FACTORS FOR PROGRESSION TO SEVERE SLE
In multivariable analysis, the following features were associated with a risk to progression to severe SLE:
a) an age of less than 25 years at the time of DLE diagnosis (OR, 2.8; 95% CI, 1.1-7.0; scored 1 point if present)
b) phototype V to VI (OR, 2.7; 95% CI, 1.1-7.0; scored 1 point if present )
c) an antinuclear antibody titers of 1:320 or higher (OR, 15; 95% CI, 3.3-67.3; scored 5 points if present).
SCORING SYSTEM TO PREDICT PROGRESSION TO SEVERE SLE
Among the 54 patients with a score of 0 at baseline, none progressed to severe SLE. In contrast, 1 (6%) of 17 patients with a score of 1, 1 (17%) of 6 patients with a score of 2, 6 (18%) of 33 patients with a score of 5, 18 (39%) of 46 patients with a score of 6, and 4 (50%) of 8 patients with a score of 7 developed DLE- sSLE.
Conclusions
The authors of this study helped develop a simple scoring system using three items that can predict progression of DLE to severe SLE:
1) an age of <25 years at the time of DLE diagnosis (1 point)
2) ANA titers of 1:320 or more (5 points)
3) Phototype V or VI (1 point)
Patients with a score of zero have zero risk. Patients with a score of 6 or more have markedly increased risk.
The authors say that we may reassure patients with DLE with a score of 1 or less, even among those who fulfilled the ACR/EULAR 2019 criteria for SLE. Moreover, patients with DLE with a score of 6 or more may require closer monitoring.
REFERENCE
Fredeau L et al. Risk factors of progression from discoid lupus to severe systemic lupus erythematosus: a registry-based cohort study of 164 patients. J Am Acad Dermatol. 2023 Mar;88(3):551-559.
Wieczorek IT, Propert KJ, Okawa J, Werth VP. Systemic symptoms in the progression of cutaneous to systemic lupus erythematosus. JAMA Dermatol. 2014;150(3):291-296.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.