How deep should a scalp biopsy be? What problems arise if it's too shallow?
Depth of the Biopsy: What needs to be considered?
A proper scalp biopsy is 4 mm wide and deep into the fat layer.
There are several technical challenges that physicians can run into when doing scalp biopsies. One is not really a challenge at all but involves choosing the wrong sized punch biopsy tool. Too often physicians reach for a 3 mm or 3.4 mm punch in hopes that it will cause the patient less scarring. Sometimes even a 2 mm punch is used but fortunately that’s not common. A 4 mm punch is the proper size and allow the pathologist to measure hair follicle densities in a standard way.
The second technical error when performing biopsies is to make the biopsy too shallow. A physician might naturally be scared sometimes to go too deep out of fear a damaging a nerve or blood vessel. It’s true that some areas like the temples have pretty delicate neuromuscular structures. However, for the main areas where biopsies are done the scalp punch biopsy must extend deep into the fat layer to get a good sample for the pathologist. A deep punch is the only way for the pathologist to visualize what’s happening deep down in the fat layer and to visual the bulbs of the hair follicles.
The final depth is usually about 5-7 mm. Here’s a biopsy that is 4 mm wide and 7.4 mm deep. You can see the bottom of the hairs bulbs easily and lots of fat has been taken.
A good scalp biopsy is 4 mm in width and deep into the fat layer, well under where the hair ‘bulbs’ end.
A doctor must punch nice and deep if diagnoses like dissecting cellulitis, panniculitis, alopecia areata are suspected. It’s always nice of course to have deep biopsies to accurately count hairs in androgenetic alopecia, telogen effluvium and others.
Does a shallow biopsy need to be repeated?
I’m often asked if a shallow biopsy should be discarded and a new sample taken that is deeper. First, a shallow biopsy should always be analyzed by the pathologist because it still has a great great deal of useful information. Much of the information needs to rule in or rule out scarring alopecia lives just under the surface so poorly performed biopsies (ie too shallow) may not be a big problem or make a big difference if all the doctor is trying to do is rule in or rule out a scarring alopecia.
Second, sometimes the skin of the scalp is so thin from advanced age or advanced atrophy that it’s really difficult to go too deep. Third, sometimes the scarring is so incredibly thick that it’s touch to punch too deep. So there are a variety of reasons by a physician ends up with a biopsy that seems too shallow.
A Closer Look at 4 Situations that Follow A Shallow Biopsy
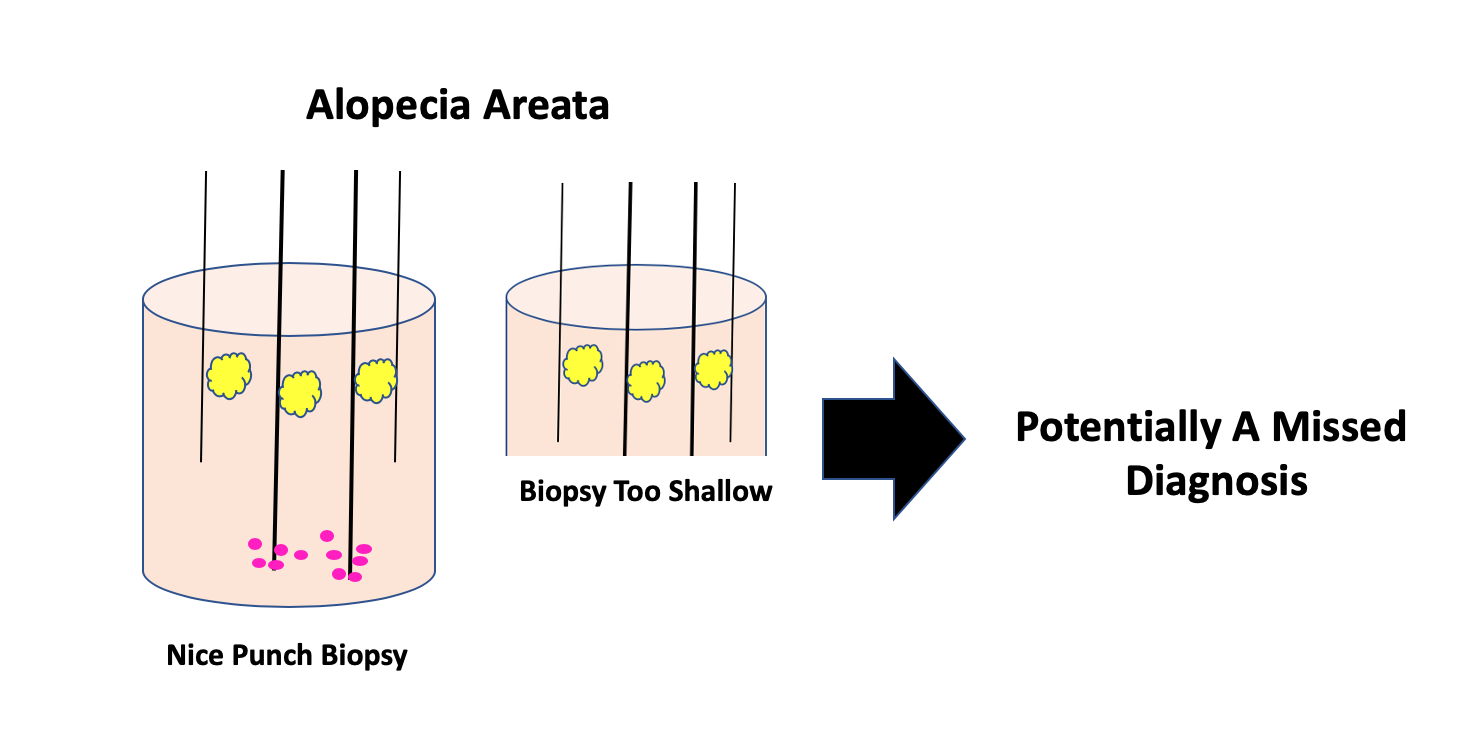
Example 1: Alopecia Areata: A Potentially Missed Diagnosis
It’s possible with a biopsy that is too shallow the a subtle diagnosis of alopecia areata might be missed. One of the hallmark features of alopecia areata is the identification of inflammation at the bottom of the biopsy. Pathologists refer to this as the so called “swarm of bees” sign. Now, an astute pathologist might be able to identify other signs of alopecia areata besides the inflammation hiding at the bottom of biopsy. These includes an increased number of catagen hairs and inflammatory cells known as eosinophils hiding in the spaces left behind when the hairs fall out. These can sometimes be seen even in a biopsy that is too shallow. But the main point here is that seeing the entire bottom fo the scalp biopsy can make challenging diagnoses and subtle diagnosis (such as alopecia areata) much easier.
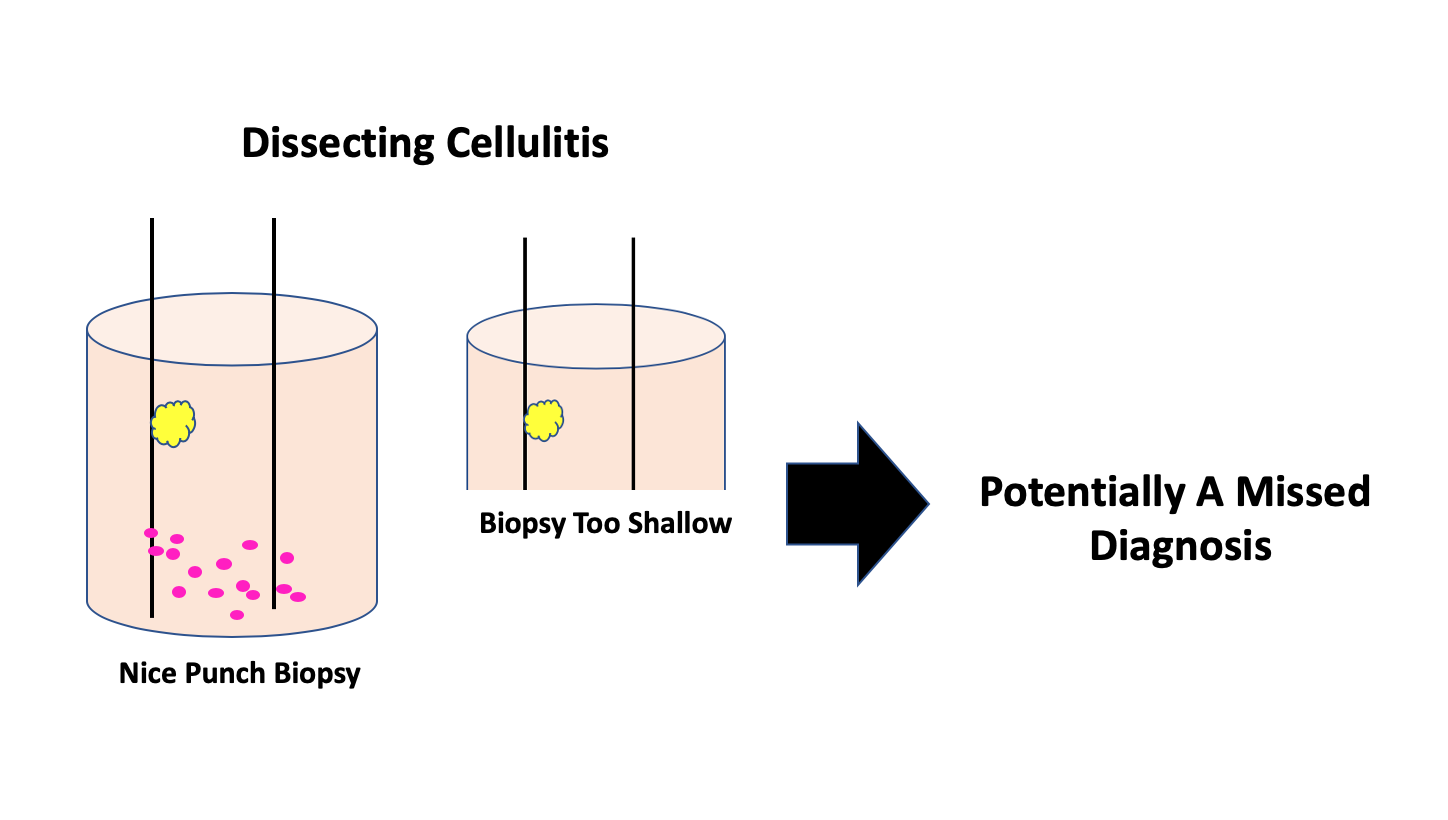
Example 2: Dissecting Cellulitis : A Potentially Missed Diagnosis
It’s possible with a biopsy that is too shallow the a subtle diagnosis of dissecting cellulitis might be missed. One of the hallmark features of dissecting cellulitis is the identification of inflammation at the bottom of the biopsy. This early staged inflammation causes hairs to fall out. Now an astute pathologist might still be able to identify other features of the biopsy higher up including scar tissue, secondary infection and even some f the sinus tracts.. But the main point here is that seeing the entire bottom fo the scalp biopsy can make challenging diagnoses and subtle diagnosis (such as dissecting cellulitis) much easier.
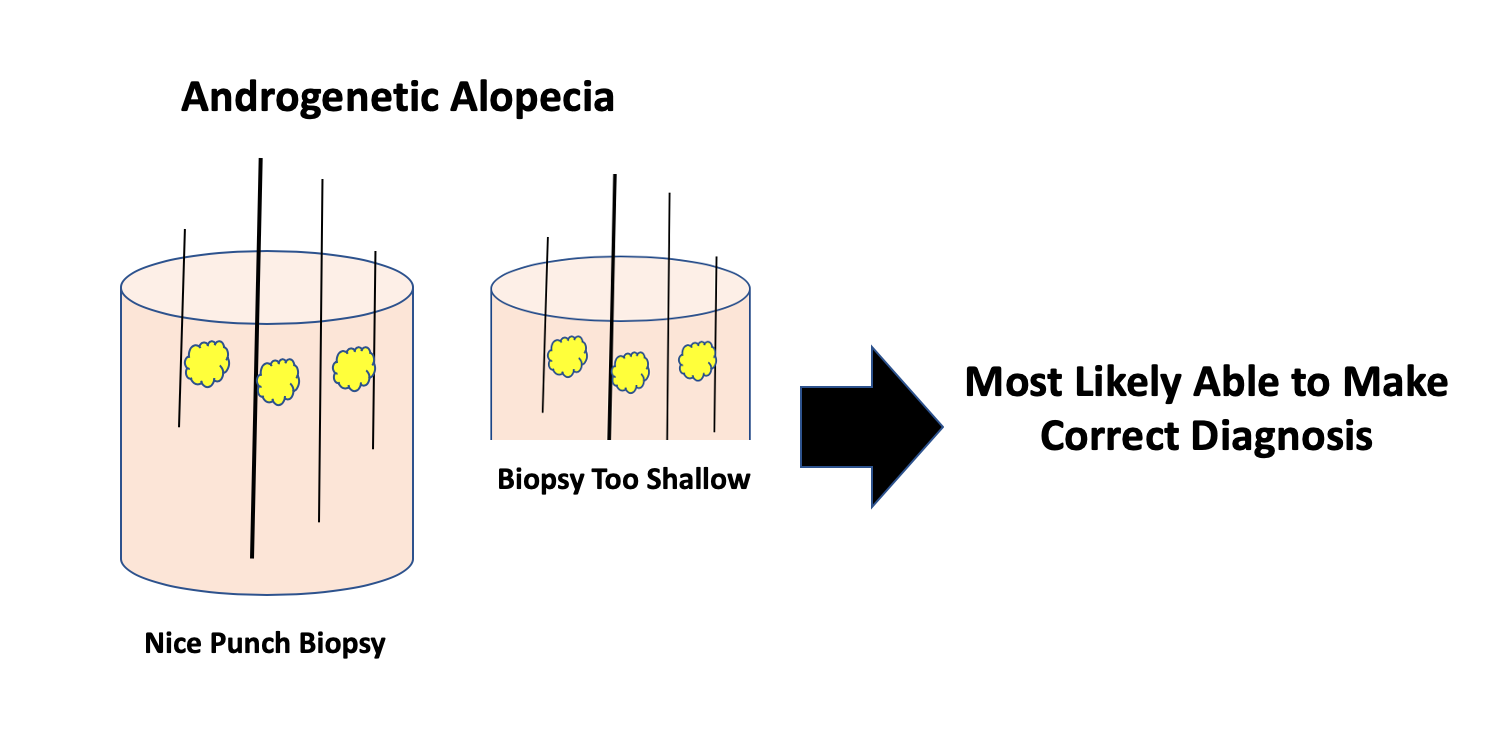
Example 3: Androgenetic Alopecia: Usually Diagnosis Still Possible.
It’s not all that likely that a biopsy that is too shallow will cause a diagnosis of androgenetic alopecia to be missed. One of the hallmark features of androgenetic alopecia is the identification miniaturizing hairs, vellus hairs and hairs of all different diameters. This can often be appreciated even in a biopsy that was taken too shallow. Of course, other diagnoses might be missed that could be present with the androgenetic alopecia.
Example 4: Lichen Planopilaris : Usually Diagnosis Still Possible.
It’s not all that likely that a biopsy that is too shallow will cause a diagnosis of lichen planopilaris to be missed. One of the hallmark features of lichen planopilaris is the identification that sebaceous glands (oil glands) are lost, that inflammation is present around the hairs, that scarring is present around the hairs and that hair cells are dying. This can often be appreciated even in a biopsy that was taken too shallow. Of course, other diagnoses might be missed that could be present with the scarring alopecia..
Summary and Conclusion
In summary, most good scalp biopsies are 5-7 mm deep and deep into the fat and well under the area where the hairs stop. This allows the pathology to see the bottom of the follicles and get a good sense of the inflammatory pattern sin the deep dermis and subcutaneous fat. To watch the related video, click here
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.