Normal Appearing Areas of the Scalp in Frontal Fibrosing Alopecia Show Abnormalities
Is FFA involvement More Widespread than in Looks? Does it matter?
Authors of a new study sought to compare the histopathological features of the frontal hairline in patients with FFA compared to the ‘normal appearing’ parietal area. The purpose of the study was to determine if normal appearing areas of the scalp have any pathological abnormalities.
Two dermoscopy-guided 4 mm punch scalp biopsies were performed on all patients. The first one was done in the frontal hairline in the most clinically affected area. The second one was done in a “normal-appearing” parietal area based on the absence of trichoscopic signs of FFA. All specimens were divided and analyzed between two dermatopathologists, and then processed and stained with hematoxylin-eosin and cut in vertical sections. Orcein stain was used to assess elastic fibers.
Results
A total of 52 women with FFA were included, which implied 104 scalp biopsies. The mean distance between both areas was 4 cm (1.4–17.6 cm, SD 3.26).
A. INFLAMMATION PRESENT IN FFA AND NORMAL APPEARING SCALP
Inflammation was present in both clinically apparent FFA and normal appearing areas. Inflammation was present in 92.3 % of biopsies from FFA areas and 86.5% of normal appearing areas.
B. NORMAL APPEARING AREAS SHOWED ABNORMALITIES OF ORS AND PERIFOLLICULAR FIBROSIS
Normal appearing areas showed inflammatory changes - just fewer and less pronounced than in clinically apparent FFA areas. Vacuolar degeneration of the ORS was present in 36.5% of normal appearing areas and 64.7 % of FFA areas. ORS necrosis was present in 15.4 % of biopsies from normal appearing scalp (and 43% of FFA areas). Perifollicular fibrosis was present in 30.8% of normal appearing areas and 71 % of FFA areas.
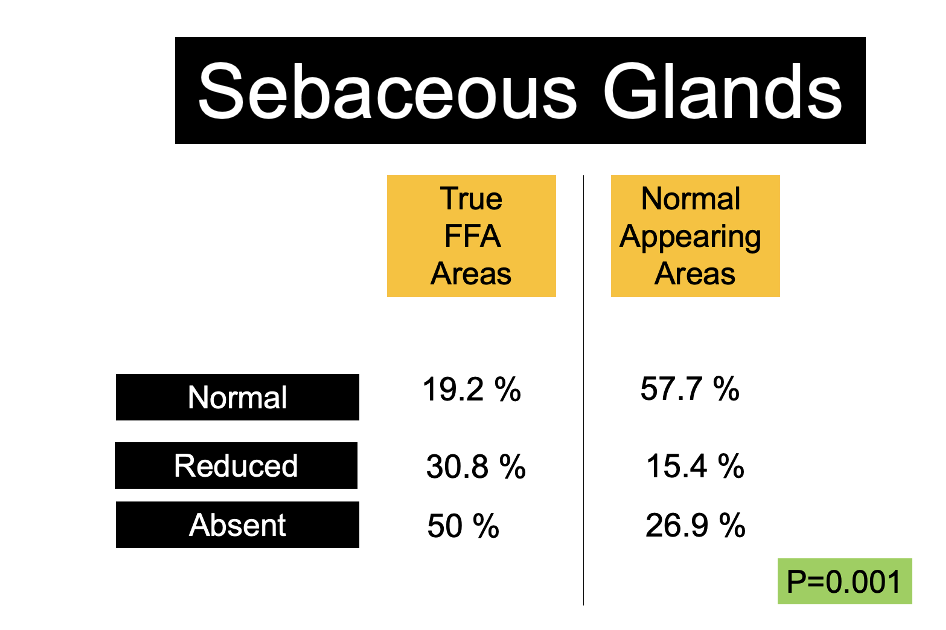
C. SEBACEOUS GLANDS REDUCED IN SOME NORMAL APPEARING SCALP
In clinically apparent FFA, sebaceous glands were normal in 19.2% (10/52), reduced in 30.8% (16/52), and absent in 50% (26/52), whereas in normal appearing areas, normal sebaceous glands were observed in 57.7% (30/52), reduced in 15.4% (8/52), and absent in 26.9% (14/52) (p = 0.001) .
Conclusions
This study showed that both the normal and FFA appearing scalp have histopathological changes. The presence of the inflammatory infiltrate, sebaceous gland atrophy, and perifollicular fibrosis were found in the normal-appearing scalp and frontal hairline area in patients with FFA. All the histopathological features described in FFA were observed in both the frontal active hairline and the “normal-appearing” scalp, although some of them were less frequent or to a lesser degree in the latter.
The existence of histological abnormalities in areas of the scalp without clinical and trichoscopic inflammatory signs suggests that FFA may affect the entire scalp. The reasons why these areas don’t develop scarring alopecia as readily is not clear. The frontal hairline is somehow more susceptible to the hair loss than the parietal area.
This study by Porriño-Bustamante ML et al builds on prior studies published by Doche and colleagues in 2020. Doche et al showed that "normal-appearing" scalp that is devoid of clinical lesions of LPP and FFA showed lymphocytic perifollicular inflammation around the isthmus/infundibulum areas in 65% of biopsy specimens, perifollicular fibrosis in 15% and mucin deposits in 7.5% of the cases.
The reason why this normal-appearing scalp, with histopathological evidence of the disease, does not develop alopecia like the frontal hairline does, is still unknown;
This study reminds us that we don’t treat FFA based on biopsy results. We treat FFA based on clinical findings and look at the biopsy results for further information if available. There clearly will be some biopsies of FFA that return showing inflammation and loss of sebaceous glands but these areas are not at risk for losing hair and therefore do not need treatment. More studies are needed to understand the clinico-pathological correlates that predict disease progression.
Simply looking at a biopsy report and seeing that an area has FFA or LPP like features does not necessarily mean that local, intralesional or systemic treatment is needed. We treat FFA and LPP aggressively if it is showing signs of progression and signs that the disease process wants to remove hairs from the scalp or cause unpleasant symptoms. We don’t necessarily treat LPP and FFA if it shows pathological features but the patient has not lost a single hair in 5 years.
Alot of attention is given in this study and the study by Doche et al to the presence of perifollicular fibrosis. Perifollicular fibrosis is common in AGA and so is perinfundibular inflammation. Both Porriño-Bustamante ML et al and Doche et al studies have not controlled for AGA to know how much AGA contributes to perifollicular fibrosis. Perifollicular fibrosis is therefore not all that surprising in these studies as we expect to find it in the scalp of at least half of patients over 50 anyways. Perifollicular fibrosis has not been studied well enough in normal scalp biopsies in different areas of the scalp and according to different age groups to really interpret too much about perifollicular fibrosis.
The changes in sebaceous glands in normal appearing scalp and the necrosis and vacuolar change in the outer root sheath keratinocytes are among the more interesting and surprising findings in my opinion.
More studies are needed to better understand the progression of changes of the normal scalp according to age as well as in different areas of the scalp.
REFERENCE
Porriño-Bustamante ML et al Frontal Fibrosing Alopecia: A Histopathological Comparison of the Frontal Hairline with Normal-Appearing Scalp. J Clin Med. 2022 Jul 15;11(14):4121.
Doche et al. "Normal-appearing" scalp areas are also affected in lichen planopilaris and frontal fibrosing alopecia: An observational histopathologic study of 40 patients. Exp Dermatol. 2020 Mar;29(3):278-281.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.