Hair Transplantation for Frontal Fibrosing Alopecia
Donovan FFA Hair Transplant Candidacy Criteria
The criteria we use in our clinic for evaluating FFA candidacy are more strict and rigorous than the criteria we use for lichen planopilaris. Hair transplants for FFA can be successful, but the overall chances of success are lower than for LPP. Not everyone who has surgery has a nice result and graft loss over 5-10 years is expected at least to some degree. Neverthless, the carefully selected FFA patient is often very very happy with their outcomes!
In order to be a candidate for hair transplant surgery, ALL FIVE of the following criteria must “ideally” be met in a patient with FFA who wishes to have surgery. Patients who do not meet these criteria could still be candidates - but the risk of a ‘less than satisfactory outcome” may be higher.
1. The PATIENT should ideally be kept on a 5 alpha reductase inhibitor medications during and after surgery (or be able to come off all medications without ANY evidence of disease reactivation over 2 years of close observation).
I do believe that the group of FFA patients who do the best with hair transplant surgery (ie the best long term outcomes after 5 and 10 years) are those that are kept on oral finasteride or dutasteride prior to, during, and after surgery. This many not be possible for all patients, of course, but this seems to increase the odds of a pretty good outcome. We don’t know if topical finasteride or topical dutasteride or dutasteride ‘mesotherapy’ offers similar benefits. Furthermore, we don’t know if oral or topical minoxidil or periodic use of pimecrolimus offers benefit but I suspect it may as well - especially minoxidil. Patients with an ongoing treatment plan seem to do best (in my opinion).
I am no longer of the opinion that coming ‘off’ all medications is really the best plan in FFA. It’s true that ideally the patient should be off all topical, oral and injection medications to truly know 100% that the disease is "burned out (burnt out)". However, I think this is a risk and even someone with what appears to be burnt out FFA can reactivate years later. The ideal plan for a long term good outcome is staying on some sort of first line FFA treatment.
Therefore, the ideal patient is one with long term stable treatment induced inactive FFA. The ideal candidate is someone who stays on treatment - especially 5 alpha reductase inhibitors. The absolute best candidate, however, is someone who already has proven that they did not flare after a prior surgery.
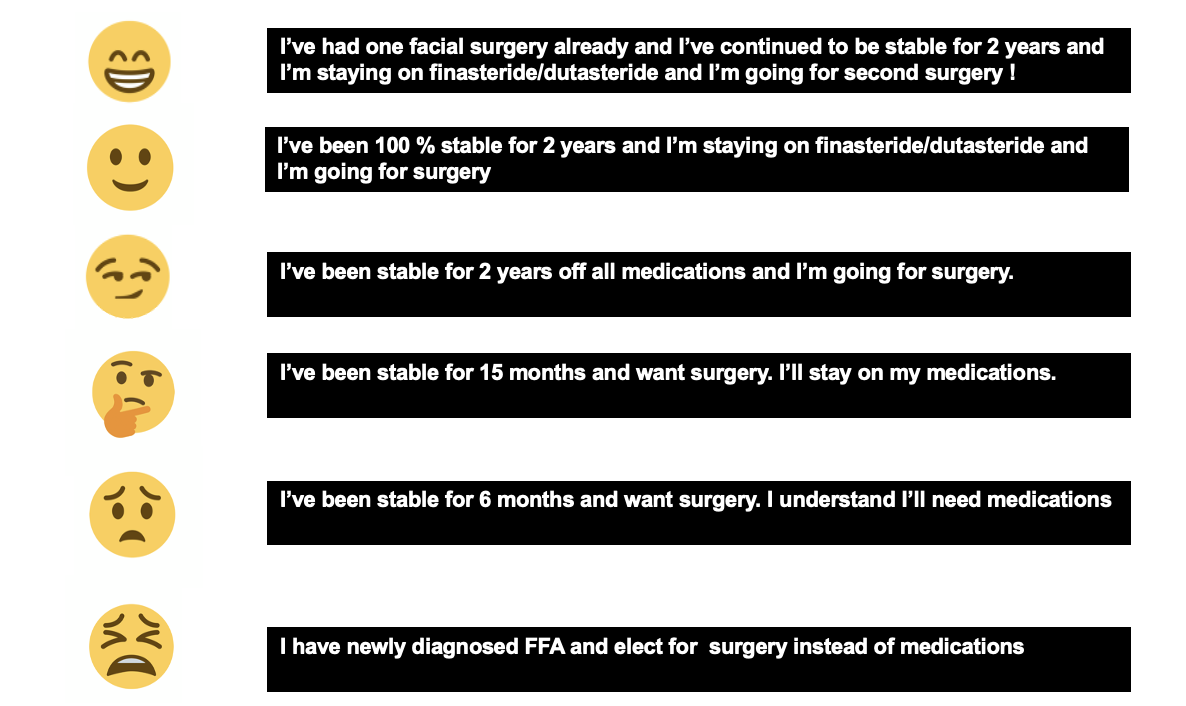
For those more visual, I rank these as follows:
2. The PATIENT must not report symptoms related to the FFA in the past 24 months prior to surgery.
The patient must have no significant itching, burning or pain. One must always keep in mind that the absence of symptoms does not prove the disease is quiet because FFA can be a quiet condition in some patients anyways. In FFA, the presence of symptoms raises suspicion the disease could be active. Even the periodic development of itching or burning from time to time could indicate the disease has triggers that cause a flare and that the patient is not a candidate for surgery. The patient who dabs a bit of clobetasol now and then on the scalp to control a bit of itching may also have disease that is not completely quiet. We need to be really strict if we are going to say someone is stable.
3. The PHYSICIAN must make note of no clinical evidence of active disease in the scalp, eyebrows, eyelashes and body hair in the past 24 months.
There must be no scalp clinical evidence of active FFA such as perifollicular erythema, perifollicular scale (follicular hyperkeratosis). This assessment is best done with a patient who has not washed his or her hair for 48 hours. Some scalp redness may be persistent in some patients with scarring alopecia even when the disease is quiet. Therefore scalp redness alone does not ‘necessarily‘ equate to a concerning finding. Perifollicular redness, however, is more concerning for disease activity. In addition, the patient must have no evidence in the scalp for active lichen planopilaris. In addition, the pull test must be completely negative for anagen hairs and less than 3 for telogen hairs. A positive pull test for anagen hairs indicates an active scarring alopecia regardless of any other criteria.
In addition to the scalp, there should be no NEW changes in body hair or eyebrows in the past 12 months. Even if the scalp is quiet, new eyebrow loss indicates an increased change for disease flare following surgery.
4. Both the PATIENT and PHYSICIAN must demonstrate no evidence of ongoing hair loss over the past 24 months.
There must be no further hair loss over a period of 24 months of monitoring off the previous hair loss treatment medications. This general includes the patient and physician's perception that there has been no further loss, physician's measurements from the glabella to the frontal hairline showing no changes, as well as serial photographs every 6-12 months showing no changes.
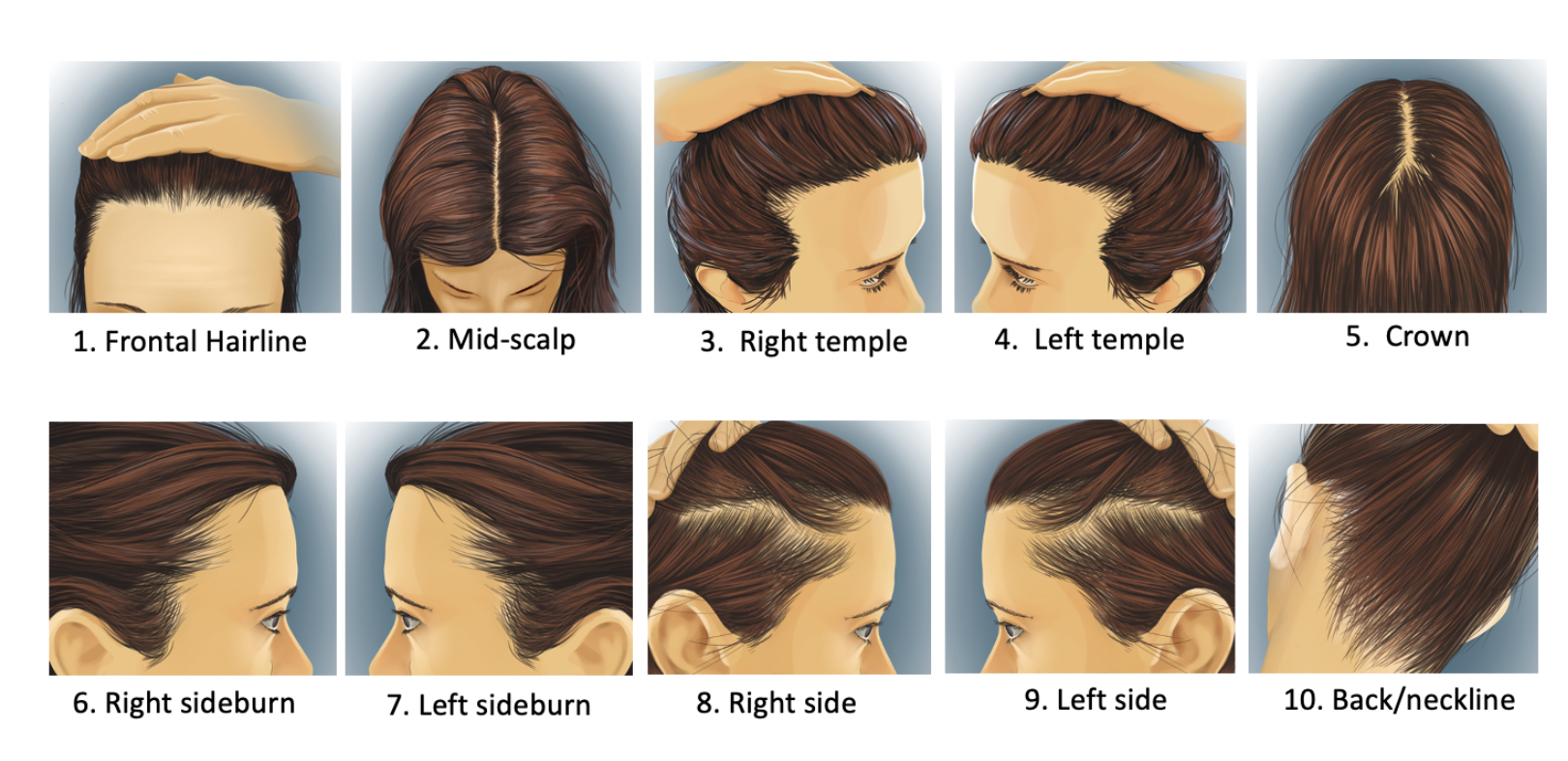
The photos that need to be compared are as follows (as well as eyebrow and eyelash hair)
5. The patient must have sufficient donor hair for the transplant.
Not all patients with FFA have sufficient donor hair even if their disease has become quiet. This is because many also have coexistent lichen planopilaris.
In situations where there is concern that the FFA may be active or concern that the surgery may not be a success, strong consideration should be given to performing a 'test session' of 50-100 grafts and observing their survival over a period of 6-9 months.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.