Hyperprolactinemia: Does elevated prolactin contribute to hair loss?
A Basic Primer on Prolactin and Addressing Elevated Prolactin
Introduction: Why does the hair specialist need to understand prolactin?
Hair specialists need to know a thing or two about prolactin. These reason is that hair specialists who are involved in the full evaluation of patients with hair loss are going to encounter abnormally elevated prolactin lab test results on a fairly frequent basis. It’s helpful to know what to do in these situations. In general, all women with hair loss who also have irregular menstrual cycles require a prolactin test in addition to other blood tests (LH, FSH, progesterone, testosterone, DHEAS, estradiol, 17 OHP, androstenedione, SHBG, AM cortisol). About 5 % of women with irregular cycles are going to have some degree of abnormal prolactin test result, so the hair specialist should have some understanding as to what to do next.
Below, we will review some of the basics of prolactin, focusing on the information that is most relevant to the hair loss specialist.
What is prolactin?
Prolactin is a hormone produced by the anterior pituitary gland in the brain. The main function of prolactin is thought to be to assist in development of breast tissue and facilitation of lactation. However, prolactin also has a range of reproductive, metabolic and immune functions as well.
The typical prolactin level is under 25 ug/L (25 ng/ml) although some labs set this cut off at 20 ng/mL and some set it at 30 ng/mL. It is important to consider the specific reference cut off value that the lab uses in order to determine if a prolactin reading is abnormal.
How common is hyperprolactinemia (elevated prolactin levels in the blood)?
Hyperprolactinemia is a frequently encountered endocrine condition. The finding of elevated prolactin is estimated to occur in about in 1 in 200 individuals and is much more common in women. Among women with menstrual irregularities and fertility concerns, hyperprolactinemia occurs even more commonly - in up to 10 % of individuals. About 1 in 2,000 individuals have a prolactin producing tumor in the pituitary gland called a prolactinoma. Prolactinomas are most common in women in the age group 25-35.
What are common signs someone with hyperprolactinemia might experience?
The symptoms and signs of hyperprolactinemia will depend on the degree of elevation and specific patient characteristics as well. Many patients with mildly elevated prolactin levels do not have any symptoms at all so that’s important to always keep in mind.
Symptoms of elevated prolactin in women may include:
· Irregular menstrual cycles (short luteal phase)
· No menstrual cycles (amenorrhea)
· Low energy
· Infertility
· Decreased libido
· Breast enlargement
· Breast milk production (galactorrhea) in non-pregnant individuals
· Weight gain
· Hot flushes
· Vaginal dryness
· Low muscle mass
· Decreased bone density
· Headaches, nausea, vomiting
· Vision problems
Symptoms of elevated prolactin in men may include:
· Decreased bone density (osteopenia)
· Infertility
· Low sperm counts
· Decreased libido
· Erectile dysfunction
· Weight gain
· Low energy
· Low muscle mass
· Decreased body hair
· Headaches, nausea, vomiting
· Vision problems
· Breast enlargement (gynecomastia)
· Breast milk production (galactorrhea)
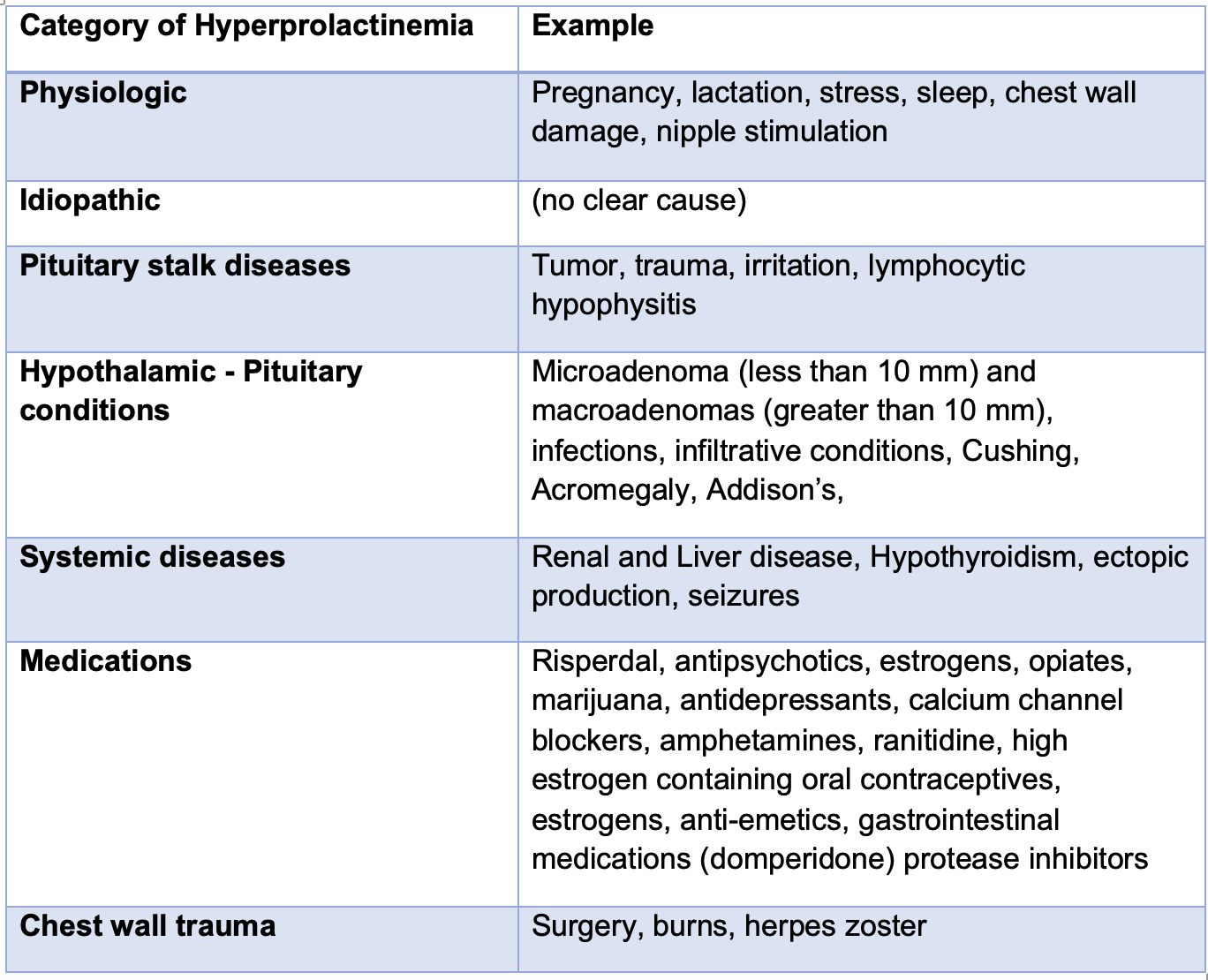
What are common causes of elevated prolactin?
There are about 50 possible causes of elevated prolactin. Common causes of elevated prolactin (hyperprolactinemia) are shown in the table below. Causes of elevated prolactin divided into physiological, idiopathic, pituitary gland related, pituitary stalk related, systemic disease and medications. Sometimes, no cause can be found and patients are then said to have “idiopathic” hyperprolactinemia. Macroprolactinemia is a cause of pseudohyperprolactinemia (false elevation) and is not a true cause of elevated prolactin. We will review that in a moment.
Causes of Elevated prolactin by Frequency of Occurrence.
When one looks at all the causes of elevated prolactin levels, a 2008 study by Viler et al of 1234 patients showed the breakdown of causes. That study showed that benign tumors known as prolactinomas top the list of causes in 53 % of those with elevated prolactin. This is followed by drug induced causes (14.3 %), macroprolactin (9.3%), non-functional pituitary adenomas stalk effect (6.6%), hypothyroidism (6.3 %), idiopathic (3.6 %) and acromegaly (3.2%).
Many patients with elevated prolactin levels have concerns that the elevated could be due to a pituitary tumor called a prolactinoma. This particular concern needs to be properly evaluated by a physician. The precise chance of that a patient has a prolactinoma as the reason for their elevated prolactin level increases as the prolactin level rises. Among patients under age 50, prolactinomas are more common in women. With age, prolactinomas become more common among men. It’s actually rare for men to be diagnosed with a prolactinoma under age 50. Men also tend to have larger tumors than women. If the prolactin levels are over 200 ug/L (200 ng/mL) the likelihood that elavated prolactin is due to a tumor is very high. However, patients with small elevations in prolactin may still have a prolactinoma.
Minor increases in prolactin are often seen in healthy individuals and carry no significance. For patients with minor elevations of prolactin, the lab tests simply need repeating with the patient fasting and no exercise or physical activity within 30 minutes (or 4 hours) of the test. (See suggested testing strategies).
A Word About Macroprolactinoma
“Macroprolactinemia,” also called “pseudohyperprolactinemia” is a frequent cause of elevated prolactin in healthy patients. It is not true hyperprolactinemia and so it’s important to properly identify this condition so that patients are not given further work up or treatment. This phenomenon of macroprolactin happens when prolactin in the blood binds to IgG antibodies to form big complexes. These complexes are recognized by prolactin assays. However these complexes are too big to interact with prolactin receptors in the body so they don’t actually carry out any functions. Patients with macroprolactinemia will repeatedly show “high prolactin” on their blood tests but they won’t need to be concerned. These individuals have normal ovarian or testicular function and are asymptomatic. Generally speaking, for patients with hyperprolactinemia, it’s helpful to ask that lab to carry out polyethylene precipitation or simply ask for macroprolactin levels. If macroprolactin is identified as a significant contributor to the elevated prolactin, then no further work up is needed.
What are normal levels of prolactin and what does the degree of elevation signify?
Prolactin levels are typically less than 25 for most individuals. Slightly elevated/borderline prolactin (levels in the range 25-30 ug/L) are not typically associated with any concern.
The following diagram shows the typical conditions to consider when lab tests return with various prolactin in certain ranges. These are approximations rather than rules.
There are a wide array of possible conditions that cause mild hyperprolactinemia (levels 25-40 ug/L). Physiological causes, medications, stress, prolactinomas, hypothyroidism all need to be considered. Stress can rarely raise prolactin levels close to 100 ng/mL but this is of course not common. Prolactin levels peak after exercise and for this reason it is recommended to avoid testing after any type of exercise session.
Mild hyperprolactinemia (levels 25-40 ug/L) is common and caused by a very large number of conditions. Physiological causes (pregnancy, nipple stimulation, exercise, sexual intercourse) medications, stress, prolactinomas, hypothyroidism all need to be considered. Stress can rarely even raise prolactin levels close to 100 ng/mL but this is of course not common. Prolactin levels peak after exercise and for this reason it is recommended to avoid testing after any type of exercise session. Mild hyperprolactinemia may be associated with a short luteal phase, irregular cycles, decreased libido and infertility. Low progesterone is found in many women and causes the short luteal phase. Even mild hyperprolactinemia can affect fertility even when there are no abnormalities in the menstrual cycle. For this reason, I often advise women with persistent hyperprolactinemia to be seen by a gynecologist if a precise cause can not be found and corrected.
Moderate hyperprolactinemia (levels 40-100 ug/L) may be caused by a similar array of conditions. Hyperprolactinemia in the setting of kidney disease is usually in the range 35-100. The same is true of hyperprolactinemia occurring in the setting of hypothyroidism. 40 % of patients with primary hypothyroidism have elevated prolactin and levels are generally under 100 ug/L. This range of moderately elevated prolactin is often associated with irregular cycles in women.
Marked hyperprolactinemia (levels above 100 ug/L) is associated with more significant endocrine issues, including hypogonadism. Some drugs, including antipsychotics, may cause prolactin elevations in this range and so can pregnancy. The likelihood of a microprolactinoma is fairly high when prolactin levels return in this range above 100 ug/L. In general, prolactin levels under 200 ug/L are more typical of a microprolactinoma and levels over 200 ug/L (severe) are often associated with macroprolactinoma.
What is the work up for someone within elevated prolactin?
Patients with mildly elevated prolactin levels (under 40 ng/mL) first need to have the test repeated. It is a common occurrence to have mildly elevated prolactin given that so many issues can cause very mild elevations.
For example, poor sleep, stress, recent eating, exercise and sexual intercourse can all cause mild elevations. However, these elevations are typically in the 25-35 ug/L range rather than 50-100 range.
Repeat testing for prolactin should be done in the morning with patients avoiding physical or strenuous activities for a few hours before the test. Suggested strategies for taking the test most accurately can be found here.
A Complete Testing Panel Might Include Some of All of the Following:
Prolactin, macroprolactin, TSH, T3, T4, DHEAS, AM cortisol, testosterone, estradiol, LH, FSH, ANA, Beta HCG, creatinine, AST, ALT. This can ideally be done in the follicular phase of the menstrual cycle for premenopausal women. A day 21 progesterone could be helpful to evaluate anovulatory cycles. For patients with elevated prolactin for which no clear trigger factor can be explained, an MRI of the pituitary gland might be performed.
Patients are advised to see “Guide For Retesting Prolactin”
Does elevated prolactin cause hair loss?
It’s still not entirely clear if elevated prolactin contributes to hair loss or not. There is some who believe that prolonged hyperprolactinemia may increase androgens in those who are so predisposed and facilitate the development of female pattern hair loss in someone who has this tendency. This is still controversial and needs further study.
Current evidence would suggest that most patients with mildly elevated prolactin under 40 ng/mL do not experience much hair loss as a result of the elevated prolactin. Certainly women with low estrogen and hypogonadism as a direct result of elevated prolactin can potentially experience hair loss hair loss. These are generally individuals with prolactin levels above 200 ug/L. In the adrenal glands, prolactin stimulates the secretion of androgens [including dehydroepiandrosterone (DHEA)], cortisol, and aldosterone. Prolactin is also a known inducer of catagen phase. Furthermore, prolactin is growth inhibitory in some models raising the possibility that prolonged hyperprolactinemia could negatively affect hair growth. However, prolactin may inhibit 5 alpha reductase in some studies so the exact relationship is unclear.
The relationship between prolactin and hair loss has actually been very poorly studied. To date only a few studies attempt to address this issue.
Orfanos and Hertel, 1988
In 1998, Orfanos and Hertel discussed the possible relationship between hyperprolactinemia and hair loss in five female patients age 25-35 years old. Four had hypertrichosis, 4 had irregular periods, 2 had amenorrhea, 2 had galactorrhea and 2 had seborrhea and one had acne. Testosterone and thyroid function were found to be normal in these patients. Two of the 5 patients had telogen effluvium. The authors proposed that hair loss issues may occur in the setting of hyperprolactinemia. Furthermore, they proposed that women with seborrhea, acne, hypertrichosis/hirsutism and alopecia (ie the SAHA syndrome) should be tested for prolactin levels in addition to androgens and thyroid tests.
Schmidt, 1994
In 1994, Schmidt showed that women with androgenetic hair loss were more likely than controls to release prolactin from the pituitary following stimulation with thyroid releasing hormone (TRH). This suggested that prolactin may have some role in the pathogenesis of female pattern hair loss.
Lutz, 2012
One of the largest studies of prolactin in hair loss is a 2012 study by Lutz. The author studied 40 women with hyperprolactinemia and hair loss including 17.5 % with androgenetic alopecia and 82.5 % with telogen effluvium. The average age was 45.8 and most patients in the study were between 30-65. Prolactin levels were above 255 in only 2 patients, and were between 80 and 150 ng/mL in 6 patients, between 51-79 ng/mL in 10 patients and less than 50 ng/mL in 22 patients. None of the patients in the study had abnormal androgen levels.
There was no clear relationship between prolactin levels and a diagnosis of androgenetic alopecia and no relationship between prolactin levels and a diagnosis of telogen effluvium. However, 42 % of women in the study had a telogen effluvium, which was higher than expected. The conclusion of the Lutz study was that elevate prolactin does not affect hair growth patterns in most women. However, there are several unanswered questions in this study. Surprisingly, 16 of 38 (42 %) of patients had telogen rates in the occipital scalp above 20 %. It is not clear if there is in fact some threshold for which prolactin above a certain level does cause a mild telogen effluvium. It was surprising in this study that higher levels of prolactin don’t seem to cause more shedding.
The Lutz study does not provide us with any information regarding the effect of high prolactin levels on the hair. Many macroprolactinomas for example, are associated with prolactin levels above 200 ng/mL. There was only 1 patient in this study with high prolactin levels in this range so we can not conclude much about the effects of severe hyperprolactinemia on the hair. Furthermore, none of these patients had hypogonadism or severe endocrine disorders so again we cannot conclude much about hair loss in patients with hyperprolactinemia who have endocrine issues.
Further study is needed to better understand the effects of high prolactin on hair. It would be helpful to know how hair parameters change with resolution of the elevated prolactin as well as what is happening to the hair as the prolactin rises. We also need to better understand the effects of prolactin on the hair in the setting of underlying endocrine disturbances.
What are the treatments for elevated prolactin?
Many patients with elevated prolactin do not require treatment. The one exception is those with a diagnosis of a macroprolactinoma where treatment is often administered regardless of symptoms and signs. Many patients with hyperprolactinemia who are asymptomatic and have normal ovarian (women) or testicular (men) function simply need monitoring to follow the level and ensure that it does not increase or does not cause issue. That’s probably the most important thing to remember.
For example, some patients with idiopathic hyperprolactinemia just have higher prolactin levels and levels just stay this way. If the elevated prolactin is mild and does not cause problems with the patient, that patient might not necessarily need treatment. Similarly, even if a patient has a diagnosis of a pituitary microadenoma most of these tumors (50 % or more) do not enlarge over time. In fact, many people in the world have asymptomatic prolactinomas that never get diagnosed and it’s possible these tumors never cause any sort of problem in their life.
When it comes to most patients with small prolactin elevations, treatment is recommended only if the prolactin is causing some sort of issue in the body. If the patient is experiencing symptoms as a result of the elevated prolactin (reproductive, fertility, vision, headaches, galactorrhea, libido, etc – see list above) then there are both medical, surgical and radiation treatments that can be considered. Treatment is generally always considered to be a good option in cases of macroprolactinomas (great than 10 mm) and in women with microadenomas (less than 10 mm) who are considering pregnancy. These patients are started on treatment most of the time regardless if they have symptoms or not.
Treatment of hyperprolactinemia usually begins with addressing the potential cause. Therefore, a full history and physical examination is needed by the doctor. If stress or medications are the cause of the elevated prolactin, then the treatment first begins with addressing these issues and attempting to remove triggers of elevated prolactin (if deemed appropriate). If elevated prolactin is causing issue such as irregular periods, infertility, reduced libido, enlarged breast tissue, medical treatments can be considered to improve symptoms and reduce the prolactin levels.
Medical Treatments
Medical treatments are generally always considered first before considering any of the surgical treatments.
Medical treatments include agents such as bromocriptine and cabergoline (and quinagolide in some countries). Medical treatment may be coupled with periodic repeat measurements of prolactin levels and repeat MRI. The baseline health status of the patient and side effects of the medications need to be carefully considered before starting medical treatments. Therapy may not be needed lifelong in some cases as prolactin levels may decrease and remain low in some patients even after stopping medications. Similarly prolactinoma size may reduce dramatically in some patients and even disappear on follow up MRI such that medications can eventually be stopped. Many women can stop their prolactin suppressing medications in menopause.
Surgical Treatments
Surgical treatments are considered for patients in several situations including 1) women with a microprolactinoma who wish to become pregnant 2) patients who cannot tolerate medical therapies 3) patients who do not want to use medication 4) patients who used medications but did not respond 5) adenoma has cystic features on MRI and 5) patients with vision issues directly related to a pituitary issue.
Surgery is not always completely curative and recurrences of prolactinomas may occur. Furthermore, some complications are possible with surgery and these need to be carefully reviewed. Referral to a center that specializes in pituitary issues (and a highly experienced neurosurgeon) is generally advised.
Radiation Treatments
Radiation treatment is generally reserved for very special situations such as treatment of a large macroprolactinoma. It is considered a “third-line” treatment and is often combined with medical and surgical treatments rather than as a stand-alone treatment.
References
Chanson and Maiter. The epidemiology, diagnosis and treatment of Prolactinomas: The old and the new Best Pract Res Clin Endocrinol Metab . 2019 Apr;33(2):101290.
Leca et al. Identification of an optimal prolactin threshold to determine prolactinoma size using receiver operating characteristic analysis. Scientific Reports volume 11, Article number: 9801 (2021)
Lutz. Hair loss and hyperprolactinemia in women. Dermatoendocrinol 2012 Jan 1; 4(1): 65–71.
Orfanos et al. . [Disorder of hair growth in hyperprolactinemia] Z Hautkr . 1988 Jan 18;63(1):23-6.
Schmidt JB. Hormonal basis of male and female androgenic alopecia: clinical relevance. Skin Pharmacol. 1994;7(1-2):61-6.
Vilar et al. Diagnosis and management of hyperprolactinemia: Results of a Brazilian multicenter study with 1234 patients. Journal of Endocrinological Investigation 2008; 31(5):436-44
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.