Hypervitaminosis D and Vitamin D Toxicity: A Short Primer for the Hair Specialist
HYPERVITAMINOSIS D and VITAMIN D TOXICITY
Download PDF: Hypervitaminosis D
What is Hypervitaminosis D?
Hypervitaminosis D occurs when vitamin D levels rise too levels that are higher than needed to maintain normal homeostasis in the body. Numerous health conditions, including some serious and life threatening ones, may result from having vitamin D levels that are too high.
Hypervitaminosis D is often referred to as “Vitamin D Toxicity” (VDT).
Hypervitaminosis D refers to more than just high vitamin D levels in the blood. It refers to high vitamin D levels (>150 ng/ml or > 375 nmol/l) PLUS evidence of an imbalance in one or more of the body’s delicate homeostatic mechanisms such as hypercalcemia, hypercalciuria and/or clinical symptoms.
The cut off of 150 ng/mL (375 nmol/L) is somewhat arbitrary. However, it should be noted that many patients with vitamin D levels 120-175 ng/mL (300 nmol/L to 437 nmol/L) do not have signs or symptoms of vitamin D toxicity – but some do
Where do we get vitamin D from?
Most vitamin D is synthesized in the skin. Only approximately 10 % of our vitamin D comes from dietary sources so it’s hard to overdose on vitamin D from eating too many vitamin D rich foods. Vitamin D supplements provide the final source in those who are supplementing.
What are some of the normal functions of vitamin D in the body?
There are numerous functions and too many to list fully. Maintaining normal blood calcium levels and bone health are two key functions of vitamin D
What cut off of 25 hydroxyvitamin D does one typically start to worry about an individual having too high of vitamin D levels?
There is no magic cut off whereby levels below a certain cut-off are perfectly fine and levels above that number are a cause for worry. Generally speaking though, 25 hydroxyvitamin D levels above 150 ng/mL (375 nmol/L) are a cause for more urgent concern.
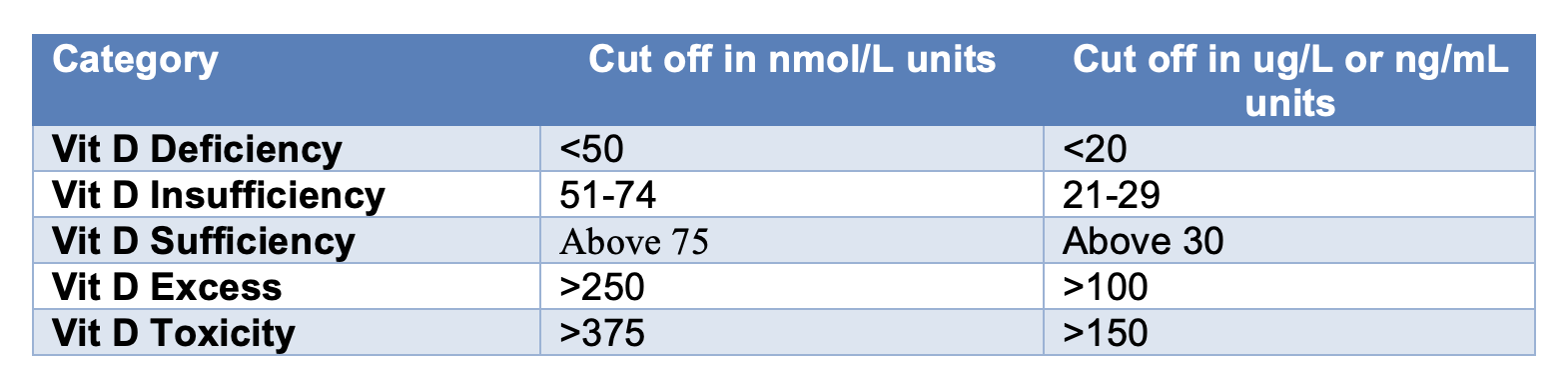
How do you classify the various vitamin D cut off levels?
How much vitamin D does one need to take to develop hypervitaminosis D?
Generally speaking, intake of 4000 IU per day or less does not lead to VDT for the vast majority of the population. Most studies would suggest that even 10,000 IU per day for several months in a row is extremely unlikely to cause vitamin D toxicity. However, these studies have not been carried out for long enough (over years and years) to know for sure that this level of chronic supplementation is safe.
What are the causes of hypervitaminosis D?
There are many causes and they are typically divided into “exogenous” causes and “endogenous” causes
“Endogenous” Causes of High Vitamin D Levels
1) In granulomatous diseases such as endogenous VDT is related to the abnormal extrarenal synthesis of 1,25(OH)2D by activated macrophages. The list of granulomatous disorders includes sarcoidosis, tuberculosis, leprosy, fungal diseases, infantile subcutaneous fat necrosis, giant cell polymyositis, and berylliosiis. In these cases, vitamin D levels can rise to high levels even with dietary intake or sun exposure.
2) Lymphomas
3) Idiopathic infantile hypercalcemia
“Exogenous” Causes of High Vitamin D Levels
Exogenous causes include taking too much vitamin D. VDT does not usually result from too much sun or eating too many vitamin D rich foods
What are the signs and symptoms of hypervitaminosis D?
Signs and symptoms are varied. Some patients have no symptoms at all. Many of the signs and symptoms are related to hypercalcemia (what happens when calcium levels in the blood rise too high).
High vitamin D levels may be associated with
o Neurological problems
§ Confusion, drowsiness, depression, psychosis
§ In rare cases, coma can result
o Gastrointestinal problems
§ Vomiting, abdominal pain, constipation, pancreatitis, peptic ulcers, loss of appetite.
o Heart problems
§ High blood pressure
§ ECG changes
· Shortened QT interval
· ST segment elevation
· Bradyarrhythmias (low heart rate)
o Kidney problems
§ Polydipsia (excessive drinking of water)
§ Polyuria (excessive urine production)
§ Dehydration
§ Kidney failure
§ Kidney stones (nephrocalcinosis)
What are three of the first measurable signs of vitamin D toxicity?
1) Hypercalcemia (high levels of calcium in the blood)
2) Hypercalciuria (high levels of calcium in the urine)
3) Hyperphosphatemia (high levels of phosphate in the blood)
Hypercalcemia, hypercalciuria and hyperphosphatemia are considered to be the initial signs of vitamin D toxicity
What tests should be done in someone with hypervitaminosis D?
A full history and physical examination should be done
· Repeat the 25 hydroxy-vitamin D levels (generally above 150 ng/mL or 375 nmol/L)
· Serum calcium (may be elevated)
· Urine calcium levels (may be elevated)
· Parathyroid hormone levels (may be low)
· 1,25 vitamin D levels are often normal but may be elevated.
· Phosphate levels
o In a hypercalcemic patient, hyperphosphatemia suggests VDT
o In a hypercalcemic patient, hypophosphatemia suggests primary hyperparathyroidism
Consideration can be given to other tests depending on the findings of the history and physical examination. These might include ECG, lipase, amylase, BUN, creatinine, sodium levels, blood pressure assessment, glucose, renal stone protocols, etc
What treatments are needed for someone with hypervitaminosis D?
· Patients with urgent symptoms including dehydration, heart issues, gastrointestinal issues, abdominal pain may need to be seen in the emergency department and some will need to be admitted.
· If VDT is due to vitamin D supplementation, then stopping vitamin D supplements and reducing calcium intake is a key first step.
· If VDT is due to granulomatous disease or lymphoma or IIH, then avoiding UV exposure is very important as a first step.
· In the emergency setting saline (sodium chloride) may be given to help rehydrate the patient and return kidney function back to normal. Once volume status is restored, loop diuretics may be given.
· The treating urgent or outpatient physician may consider
o Glucocorticosteroids to decrease serum calcium
o Calcitonin
o Bisphosphonates
o Phenobarbital
o Ketoconazole
o Hydroxychlorqouine in cases of granulomatous disease
o Rifampin
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.