What to do when you don’t know what to do: Advice for Practitioners
Getting to the diagnosis: What to do when we don’t know what to do anymore
A situation sometimes arises whereby hair specialists can’t confirm the exact diagnosis (or diagnoses) that a patient has. The clinical picture might be a bit unusual or atypical such that it does not fit perfectly into one diagnosis or another. A biopsy might be unhelpful or “equivocal.” Blood tests might not be that helpful either.
So what do we do?
A common scenario is the patient with hair shedding with what seems to be a diagnosis of ‘non-scarring alopecia.’ There is probably some debate among hair specialists as to whether this represents androgenetic alopecia or telogen effluvium or alopecia areata or something else. Some specialists might say one thing and some might say another.
What should one do when one really can’t confirm the diagnosis? Here are some tips in dealing with a challenging situation of this nature.
1. Consider whether or not one really has the full story.
In a challenging situation, one really needs to figure out if they truly have the full story. There are a few things that are often missed when collecting information about the hair loss that can have a great deal of relevance:
a) Has there been any RECENT changes in eyebrows, eyelashes or body hair? In the situation, I’m referring to new changes in these hairs - and not chronic changes. I’m not referring to eyebrow thinning from chronic tweezing that dates back 25 years but rather new changes in the eyebrows. I’m referring to recent eyelash changes and recent body hair loss. These are all potentially relevant. We don’t see a sudden and dramatic reduction in body hair loss or eyebrow hair loss in androgenetic alopecia. So if this concern is present, one needs to reconsider the diagnosis.
b) Has their been any RECENT changes in nails? I often say that hair and nails are like cousins. New changes in the nails can potentially indicate that something is not quite right. Again, here, I am not referring to chronic nail changes but rather something new.
Changes in the nails are not part of androgenetic alopecia. So if patients have these areas also affected as a new and progressive change (not a chronic issue), it may be a sign that something different than androgenetic alopecia is present. It might be that this other condition is the main diagnosis and androgenetic alopecia is not the diagnosis at all - or it could be that androgenetic alopecia is present as well as a second diagnosis.
c) Has there been any RECENT changes in the patient’s health that have been overlooked like new fatigue, new weight gain or weight loss, new joint pains, new depression, new rashes, new menstrual cycle irregularities? Here, I’m also not talking about chronic health issues but rather new things. A patient with new health concerns may not realize that they are potentially linked to hair loss or may not even realize that they are abnormal. Changes in a patient’s health may point to a systemic issue that needs investigating.
d) What exactly is the speed of hair loss? Is the hair loss progressing weekly or daily or every few months? It’s important to start having patients take photos of the scalp (or the specialist can take them himself or herself). The speed of hair loss is important. Some conditions like androgenetic alopecia don’t change on a week to week basis but conditions like telogen effluvium and alopecia areata incognito certainly can change that fast. The speed of hair loss is important.
e) What medications are taken occasionally and what medications were started and stopped in the last 1-2 years? Sometimes in challenging situations we need to start thinking about medications that were taken 6, 9 and 12 months ago or even longer. Some medications can cause a classic telogen effluvium - meaning they cause hair shedding three months after starting the drug- but this is not the mechanism for all medications. We really need to get a sense of all prescription and non prescription medications.
2. Perform trichoscopy.
It should go without saying that trichoscopy should always be a part of the diagnosis of hair loss. However, if the patient’s hair loss seems rather complex, one needs to ask exactly what was found on trichoscopy. If there is evidence of anisotricosis (variation in the caliber of hair follicles) in the frontal scalp regions but no such variation in the back of the scalp, one needs to consider androgenetic alopecia. Other features, like perifollicular scaling, perifollicular redness, scalp redness, pustules, sinus tracts, tufting, casts, exclamation mark hairs, upright regrowing hairs, black dots, red dots, yellow dots, all need to be assessed.
3. Consider whether additional blood tests are going to be helpful.
These are several key tests that are important for anyone with hair loss. These include CBC, TSH (thyroid test) and ferritin (iron test). But dozens upon dozens of other tests are also possible to consider. Should we be performing more blood tests in a person with a complex diagnosis or where the diagnosis is uncertain? Possibly, yes!
Unfortunately there is no “standard list” that I can provide because the proper tests to order will depend on the specific characteristics about the patient. ANA, ESR, CRP, DHEAS, testosterone, free testosterone, 17-hydroxyprogesterone. estradiol, LH, FSH, prolactin, AST, ALT, creatinine, urinalysis, RPR, zinc, are to be considered on a case by case basis
4. Consider whether or not to rebiopsy now or in the future if something changes.
Sometimes, the right solution to a bizarre scalp biopsy result is just to perform the scalp biopsy again. Now, that’s not always the way to go, but I think that rebiopsying is not done enough in situations where a first biopsy report is unusual or unexpected.
I’m never of the opinion that one biopsy is “all” that every single patient will need. Sometimes we need to repeat a scalp biopsy if the result is unusual and sometimes we need to get a second opinion on the biopsy whenever a pathologist provides a report that is unusual and unexpected.
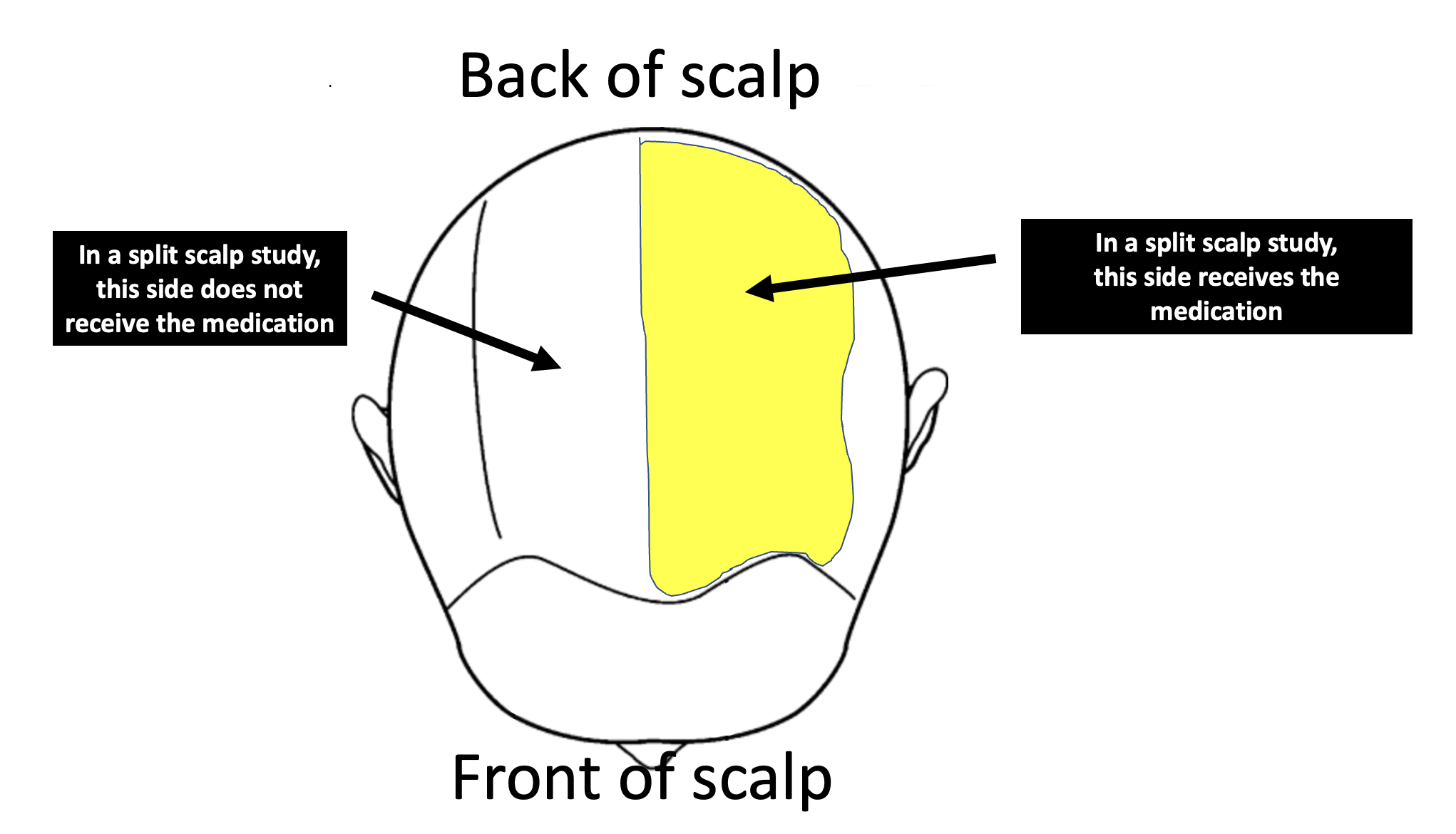
5. Consider “split scalp” studies - including whether a trial of steroid injections has a role.
I am a big believer in what I call split scalp studies. So, what is a split scalp study? Well, it’s a type of a study whereby treatment is given to one half of the scalp only and the other half is untreated.
A common use of split scalp studies is to perform steroid injections on one half of the scalp and leave the other half untreated. If hair grows profoundly with the steroid injections on the treated side we know that the this hair loss is responsive to steroid injections and likely there is an inflammatory component to the hair loss that needs serious consideration.
6. Consider a trial of “specific” treatment
In some situations where the diagnosis is really challenging and nobody can agree, it’s helpful to start a very specific treatment. By “specific” I mean something that targets a specific issue. The most specific the treatment the better.
If people are debating about low iron as being the cause of the hair loss, then I am a big believer in bringing up the iron levels in whatever way possible and seeing what happens. If ferritin levels go from 28 to 59 with iron supplementation and the hair does not improve one bit…. then guess what? We probably need to stop the debate about iron being an issue. It’s not. It’s time to move on to more productive discussion !!
Sometimes, I also consider another specific treatment - oral steroids. I wouldn’t say this is something I do daily or weekly, but every once in a while we need to have some definitive information as to whether inflammation is at the heart of the patient’s problem. If shedding stops with 4-8 weeks of prednisone or dexamethasone (at the right dose) … then we have been handed some pretty profound information. This hair loss is being caused by some sort of inflammation. I’m not a huge fan of giving people prednisone or dexamethasone but dozens of medical hair loss mysteries have been solved by a methodical use of oral steroids in this manner.
I’m usually talking about a prednisone taper (at 0.5 to 0.75 mg per kg daily starting doses) or dexamethasone taper (at 0.1 mg per kg on Saturday and 0.1 mg per kg on Sunday). If one is going to use an oral steroid then one needs to perform the test right. Starting 10 mg of prednisone to see what happens is likely not going to be helpful. There are risks of oral steroids so one needs to do this at the right time. But nothing stops inflammation as reliably as prednisone.
Some other examples of specific treatments include Clobex shampoo, oral doxycycline, oral hydroxychloroquine. I must emphasize that it’s not appropriate to use these in every tough case. But these tools are invaluable when used appropriately in the right clinical setting. Androgenetic hair loss and alopecia areata incognito won’t respond to hydroxychloroquine but an unusual telogen effluvium from suspected autoimmune disease just might. A patient whose shedding stops profoundly with hydroxychloroquine is a patient that you have proven has an immune mediated telogen effluvium.
7. Consider a trial of “non-specific” treatment.
Sometimes in these challenging cases we need to just start a non specific treatment that cheers hairs to start growing. We start and then see what happens. These treatments are non specific because they help many conditions. Examples of non specific treatments are low level laser, topical minoxidil, oral minoxidil and platelet rich plasma (PRP).
If hair grows with these treatments it does not always prove a person has one diagnosis over another but it does prove the hair loss is responsive to treatment. The end result may be a patient who is increasingly pleased with his or her hair and that’s a pretty important.
8. Consider referral to doctors outside of your field - if appropriate.
Sometimes it’s helpful to have another view on the situation or at least some aspect of the situation. Does the patient have a rheumatologic condition that you’re missing? Does the patient have a endocrine issue that you’re missing? If there is any doubt and hair loss has been going on for some time without a definitive diagnosis and definitive treatment strategy we need to start thinking outside of our box if it is appropriate and get help form others.
Don’t get me wrong. Here, I’m not taking about referring to other doctors just for the sake of referring but referring for a specific question. Here’s some examples:
a) Dear rheumatologist, This patient of mine has profound fatigue with borderline ANA of 1:80 and C4 that is low. Does this represent a rheumatologic issue in your opinion?
b) Dear nephrologist, This patient of mine has extreme thirst with marked electrolyte disturbances and rising creatinine levels. Are we missing a kidney issue in your opinion?
c) Dear gastroenterologist, This patient of mine has chronic diarrhea which she has been told is irritable bowel syndrome. She has ongoing weight loss and I’m sending her to the eye doctor to rule out uveitis. Her cousin has ulcerative colitis and her mother has rheumatoid arthritis. Do you feel this warrants colonoscopy to rule out inflammatory bowel disease?
d) Dear gynecologist, This patient of mine has somewhat high FSH and low estradiol with irregular periods, mood changes, low libido, and suspected osteopenia. Do you she has a form of ovarian insufficiency?
e) Dear endocrinologist, This patient of mine has been diagnosed with polycystic ovarian syndrome in the past and is on metformin. She has features that make be concerned about Cushing syndrome and I’m wondering if we are missing the diagnosis of Cushing syndrome. Her 24 hour urine is negative but her recent low dose dexamethasone suppression test is abnormal. Would you kindly provide your opinion? Is this a form of Cushing syndrome?
9. Consider serial photography or examination every 3 months for 1 year
One should never underestimate that value of repeat examination in challenging cases.
Consider the patient who is felt to have androgenetic alopecia. She has not started any sort of treatment and comes into the appointment with phots from the past 12 months. If the density improves slowly over time one can be certain that androgenetic alopecia is not the sole diagnosis. Androgenetic alopecia never improves on its own so if patient’s density improves slowly over time all by itself a patient might have (1) androgenetic plus a telogen effluvium that now resolved (2) no diagnosis of adnrogenetic alopecia at all or (3) androgenetic alopecia plus antoher condition that improved.
Photos are valuable !
Serial scalp and hair examinations also help give time for certain conditions to now be more apparent. If there is any doubt about a scarring alopecia, it will likely become more apparent over time if no treatment is started. In other words, if specialists are debating the diagnosis, and it is decided not to start any sort of treatment, it is likely that a tiny patch of scarring hair loss will develop over 6-18 months of observation if the diagnosis of scarring alopecia is actually the diagnosis. If it’s not a scarring alopecia no such scarred patch is going to be seen with repeat observation.
Even if a patch doesn’t form, there will possibility be some change in the eyebrows, eyelashes and body hair that suggests to the specialist that a scarring alopecia is forming.
We should not downplay the benefit of serial scalp and hair examinations in challenging cases. The diagnosis often becomes more and more clear over time.
Conclusion and Comment
Some hair loss cases a challenging. In a good number of cases, however, the diagnosis is not as challenging as we think it’s just that we have blinders on and don’t wish to accept information that is in front of us. We’re pretty resistant as physicians and hair specialist to accept a diagnosis of androgenetic alopecia in our younger patients and so many patients go from specialist to specialist carrying around a diagnosis of telogen effluvium when in fact the diagnosis is androgenetic alopecia. We do have our blinders or biases.
But in cases where the diagnosis is challenging and there is a lot of debate among specialists, we need an organized approach to get answers for the patient. First, we need a really good history and really good clinical examination. We can’t be afraid to rebiopsy or get other dermatopathology colleagues to look at the biopsy that was already done. We need to consider whether other blood tests are needed.
There are very powerful treatment trials that can be considered in complex cases - including the split scalp studies and various specific therapies like iron supplementation, oral steroids, oral doxycycline and oral hydroxychloroquine. These are advanced techniques and reserved for specific situations but can be incredibly helpful.
Repeat photography of the scalp and even repeat scalp examinations at various intervals are incredibly valuable when the diagnosis is not clear. The diagnosis often becomes clear over time!!!!!
Finally, we need refer patients to other colleagues when something just doesn’t feel right. There are about 20 different medical specialists that can get involved in challenging cases and we need to ask for help when something doesn’t seem right.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.