What is "trichotillomania" ?
Trichotillomania refers to hair loss due to an individual pulling out his or her hair. It was about 120 years ago that dermatologist Dr. François Henri Hallopeau introduced the term "trichotillomania" to describe a patient who pulled out his hair.
Trichotillomania occurs in both adults and children. My patients are often surprised when I tell them that trichotillomania is fairly common. In fact, about 3-5 % of women and 1-3 % of men will pull out hair at some point in their lives. Many patients deny pulling out their hair at first meeting, so the diagnosis can be challenging and experience is needed to know when a patient visiting your office is likely to have trichotillomania.
What hairs are pulled out?
Individuals with trichotillomania may pull out any hair on the body. Scalp hairs are the most common hairs to be pulled followed by the eyelashes, eyebrows and pubic hair.
What do patients experience?
Patients with trichotillomania experience a sense of "tension" or "unease" before hair pulling occurs or while they are trying to resist the urge to pull the hair. After the hair is pulled, individuals feel a great sense of relief or satisfaction.
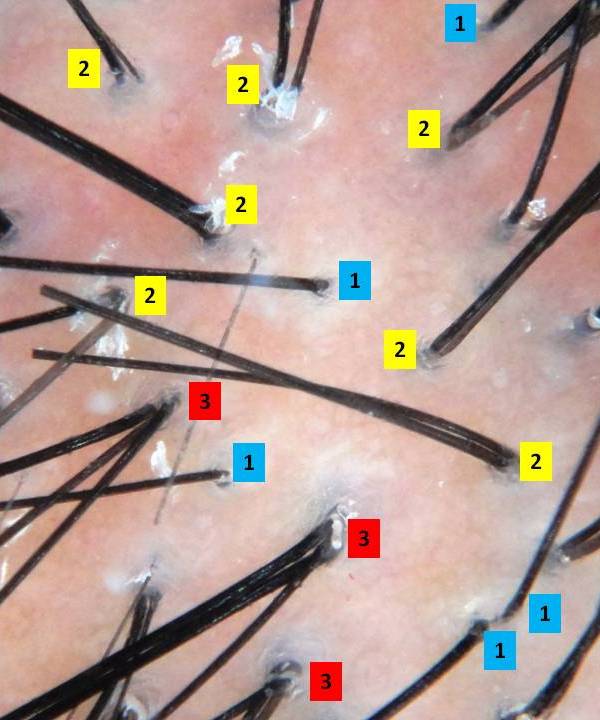
How does a physician come to the diagnosis of trichotillomania?
According to the American Psychiatric Association's "Diagnostic and Statistical Manual of Mental Disorders" (DSM-IV), there are five key features that need to be met before a patient is said to have trichotillomania.
First, the patient pulls out their hair to the point at which it causes noticeable hair loss. Second, the patient normally has some sense of tension or unease before they pull out the hair or while they are trying to resist pulling out the hair. Third, there is some pleasure or sense of relief after the hair is pulled out. Fourth, the hair pulling has to lead to some impairment in how the patient functions in social situations or at work or at school. Finally, if the hair pulling is better explained by some other mental disorder, then the diagnosis of trichotillomania is not given.
These are helpful guidelines, but it's possible for a patient to have trichotillomania without all five of these features present. There is some contraversery amongst doctors as to whether these five criteria are too restrictive.
Can trichtillomania occur in children?
Yes, In addition to adults, trichtillomania can occur in children and adolesecents. In fact, it's probably more common in chidlren than adults. In very young children (under 6) it tends to be more of a habit phenomenon. These younger children sometimes drop the habit of pulling their hair as time goes on. However, trichotillomania occuring in young pre-teens and teenagers tends to be more concerning. This hair pulling is often associated with underlying depression or anxiety and may last a long time. It may affects school and home life. These children often need psychological or psychiatric help.
How much hair can be lost?
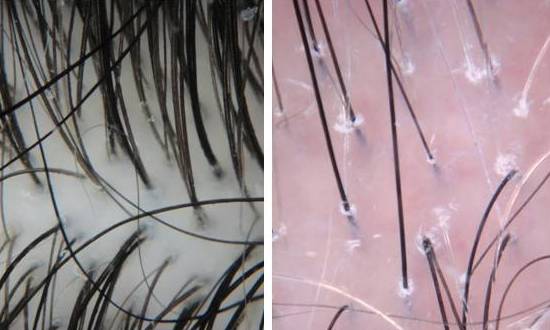
Trichotillmania can lead to small amounts of hair loss or rarely complete loss of all hair on the scalp.
Is there are cure?
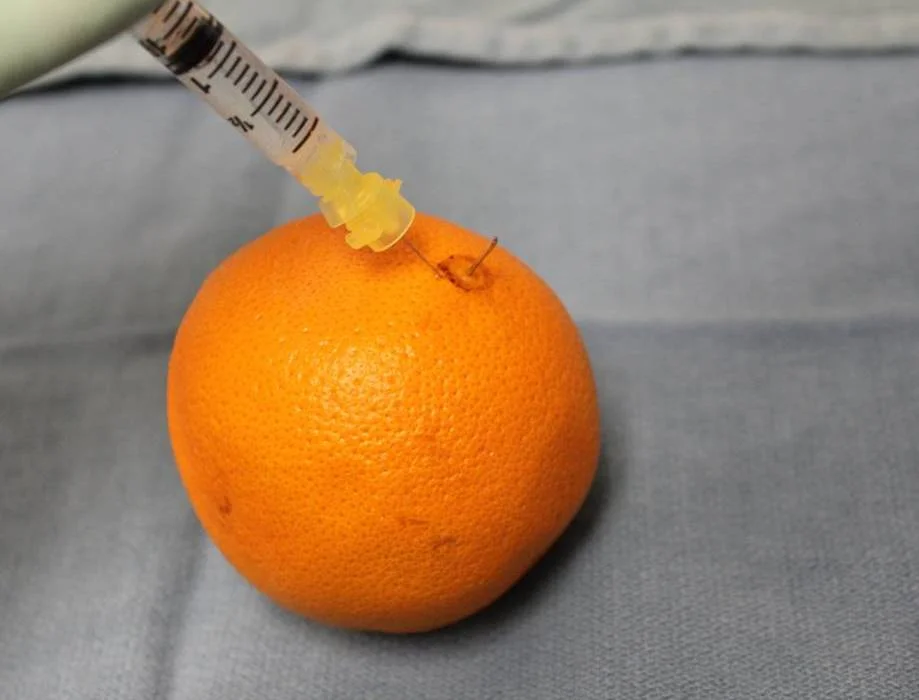
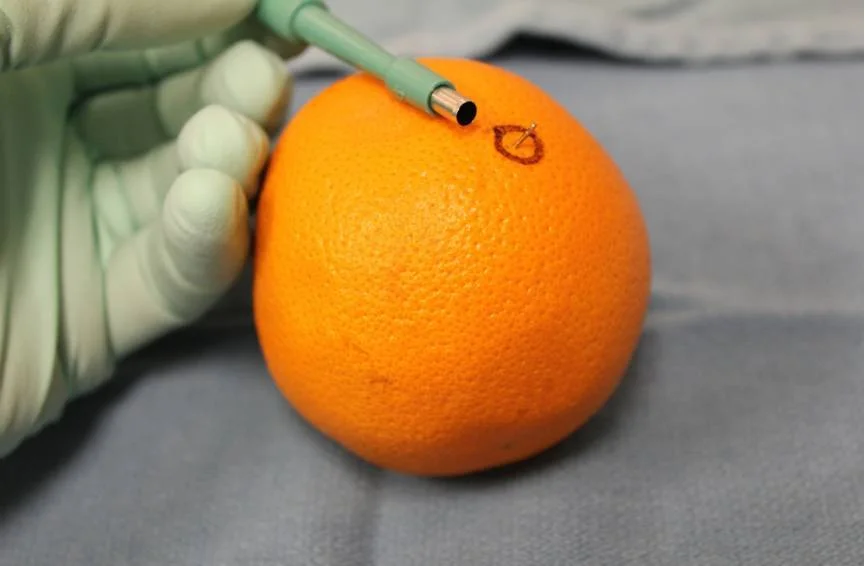
At present there is no cure. Medications and psychotherapy provided by a psychiatrist or psychologist can be helpful in some cases. Wigs, hair pieces and other forms a scalp camouflage may be used by patients with trichotillomania. Hair Transplantation can also be performed in patients who are stable and have stopped pulling. (see article on Hair Transplantation for Trichotillomania).
References
1) American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders. Fourth Edition. Text Revision Washington, DC: American Psychiatric Association.
2) Woods et al. Understanding and treating trichotillomania: What we known and what we don't. Pschiatr Clin N Am 2006; 29L 487-501
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.