What options are left for my hair loss?
What should I do about my hair loss?
I’ve selected this question below for this week’s question of the week. It allows us to discuss the advanced management of non scarring alopecia.
Here is the question….
QUESTION
Dr. Donovan I have been following your blogs and articles for quite some time and decided to tell my hair loss story and hopefully get some answers. I am a 58 year old very healthy female with no nutritional issues and an avid runner for many years. At 48 my hair started thin but underneath and at the mid back scalp in a diffuse pattern. I was put on Yaz birth control and finasteride which helped tremendously for 3 yrs. At 51 my gynecologist took me off birth control at which time I started to see similar issues recur. I started topical minoxidil, traditional HRT but nothing worked. I saw a dermatologist and she diagnosed me with AGA and started me on Climen, HRT in addition to finasteride and topical minoxidil. Within a few months I saw another dermatologist who added spironolactone 100 mg. This combo seemed to bring back my hair growth and density within 6-9 months. After a year or so my creatinine levels were in the high range and my gynecologist advised me to stop the spiro. Within a year or so after stopping I noticed significant shedding, less density mid scalp to bottom of my hair and dry hair that looked like a broom. I had numerous PRP sessions, laser cap and started various combos of low dose oral minoxidil, topical and the Climen.
I have no visible scalp anywhere but a lot of different layers and short pieces of fine hair and no bottom to my hair. Dry hair of varying lengths mostly underneath hair. The hair has changed from long straight to short and curly with no density. Cutting has not made any difference in the fullness. From the ear down the hair is thin fine and basically see through. I do not know why there is no improvement in my condition. I have no itching or burning.
I am currently on oral minoxidil 2.5 mg once daily, Avodart, topical minoxidil, spironolactone 100 mg daily in addition to HRT estrogen patches and micronized progesterone 15 days every 3 months. I am still shedding enough to create concern and my hair won’t grow longer. The top of my hair is much fuller than the bottom which is wispy and thin. I have included my biopsy and photos for your review.
BLOOD TESTS
All blood results are normal and ferritin has ranged from 40-50. The only red herring is a positive ANA of 1:80 for 5 years with no symptoms. I would appreciate your opinion.
BIOPSY
Biopsy showed a non-scarring pattern with follicular miniaturization, anisotrichosis, and increase telogen hairs.
ANSWER
Many thanks for your question. Of course, I’d need the full story from A to Z , more photos and to review all your blood tests to give a complete opinion. It’s clear you have androgenetic alopecia (AGA) and a telogen effluvium (TE). In your case, I think it’s worth still looking for a trigger of your TE rather than explaining it simply by a chronic TE with no underlying cause. I think there are two important points to consider here:
1) Maximizing/Optimizing Anti-androgen Therapy
First - your hair loss has been quite responsive to anti-androgens in the past. Yaz and finasteride have helped you and Climen and spironolactone have helped you. I do think that it will be important to review with your dermatologists if there is more that can be done to maximize treatment in this big category of antiandrogens.. You are on spironolactone and dutasteride. Increasing spironolactone is not going to be a good option given your kidney (creatinine) concerns. However, brining on board other antiandrogens just might.
You and your doctors may want to carefully review if the drug bicalutamide might be considered. Bicalutamide can be used with dutasteride and spironolactone and it might even be introduced 2 or 3 times weekly if you are still going to continued on dutasteride and spironolactone. Bicalutamide is an antiandrogen (androgen receptor blocker) which is used for the treatment of male prostate cancer. It has been used off label in women for the treatment of hair loss, as well as other androgen related issues such as hirsutism (hair growth on the face). It tends to be just as well tolerated for most of my patients as dutasteride so side effects overall are low. Side effects include elevated liver enzymes, peripheral edema and gastrointestinal side effects (diarrhea, constipation, nausea). Other side effects like itching can rarely occur. General antiandrogen side effects like decreased libido, breast tenderness, breast enlargement, mood changes (depression) can occur although seem to be quite uncommon. These are the same side effects that dutasteride, finasteride and spironolactone can cause. Mood changes with bicalutamide are not common. Bicalutamide has not been associated with a decrease in bone mass (osteoporosis). An increase in liver enzymes (3 % to 11 % of patients) is quite rare although monitoring of liver enzymes for the first 2 months is recommended.
For my patients who are on anti androgens like duasteride and spironolactone already, I generally start ¼ pill (12.5 mg) for 2-3 months and then increase to ½ pill (25 mg) after that. Sometimes I start every other day. Liver enzymes are evaluated after the 4-6 weeks and then again at week 12.
2) Evaluating the Telogen Effluvium
The increased proportion of telogen hairs in your biopsy is very interesting in my opinion. I would need to know a lot more about your story and review all your blood tests, but it would seem based on the information you have provided that this needs to be explored further to make sure that we’re not missing a potential cause of shedding. There are an enormous number of triggers of shedding.
They key to evaluating shedding is to perform a search for possible triggers and if anything comes up suggestive that it could be a trigger - then this needs to be pursued fully.
Your ANA result may or may not have any relevance. It’s low and many people in the population (5-7%) have a low level ANA like this without any consequence. However, given that you are still shedding I think that you and your doctors might consider pursuing further evaluation in this area. Because your ANA is positive, further work up might be discussed with your physicians if it has not been already. The exact tests to order depends on your history (your medical story), but might include ENA, ESR, C3, C4 and CK. If there is any suggestion of rheumatological disease, referral to a rheumatologist would be advised. With chronic shedding, I always encourage patents to make sure their age appropriate screening examinations have been done. You and your primary care doctors can review if colonoscopies, and mamograms are up to date.
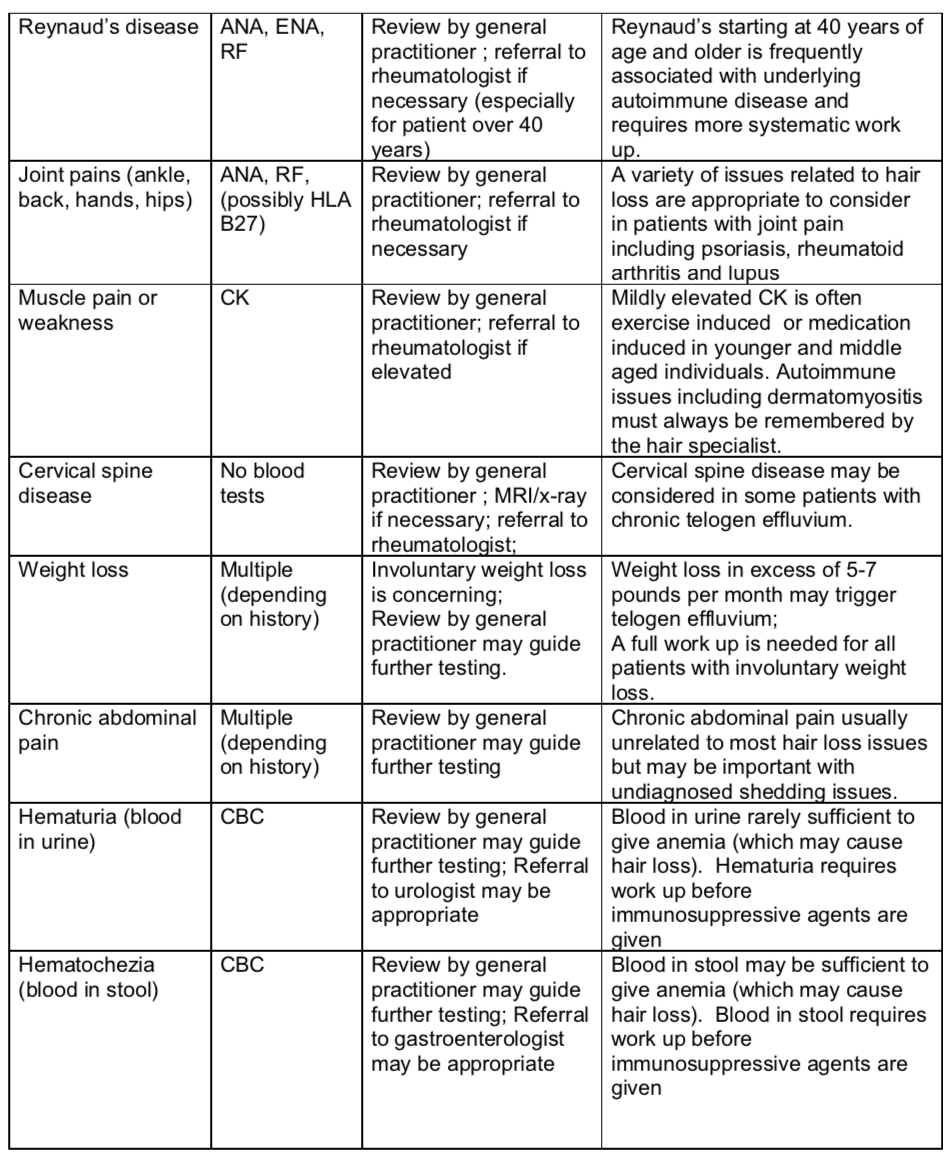
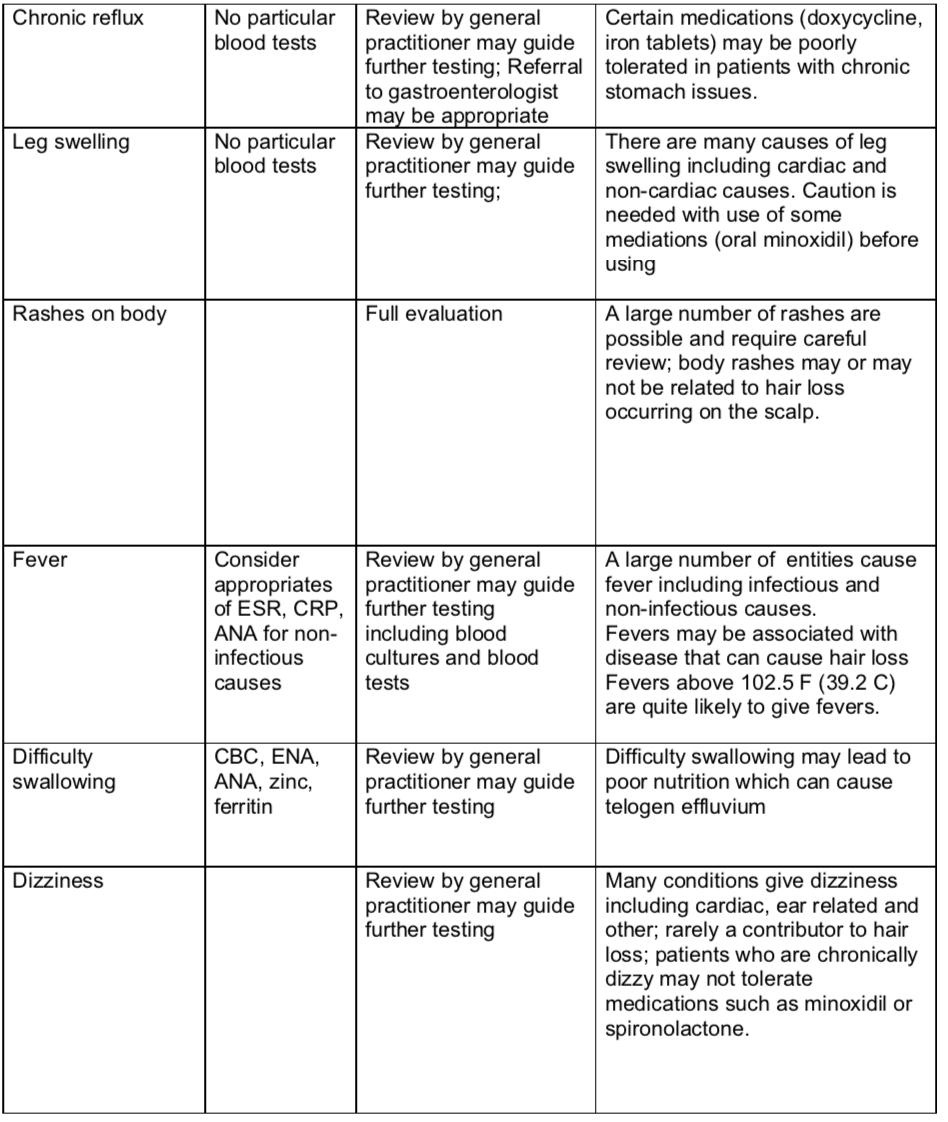
The full causes of telogen effluvium including stress, low iron, thyroid problems, medications, diets, weight loss and internal diseases. I understand based on your comments above that your iron and thyroid labs are normal. I’m assuming your vitamin D levels were normal. The remainder of your TE triggers need careful evaluation. If there are any other mediations you have started, those need to be reviewed. Furthermore, if there are any other symptoms those need careful evaluation as well. The symptoms I ask about are shown in the table below. One really needs to go head to toe when dealing with chronic shedding issues. If anything comes up - it gets explored fully. The issues that I’m most interested to ask about in a patient with positive ANA and increased telogen proportion on biopsy are whether the patient has dry mouth, dry eyes, joint pains, fatigue, weight loss, and muscle weakness.
Conclusion/Summary
Thanks again for submitting your question. I hope this was helpful in some way. I think overall you need to figure out if any more detective work needs to be done as far as your shedding goes, or has it all been done. Sometimes the detective work has all been done and we’re left with AGA and shedding. In these cases, treating the AGA fully as mentioned above is going to be important. Use of a multivitamin is going to be important. In tough cases, I may add biotin 2000 -5000 micrograms daily and a good antidandruff shampooing regimen. Of course, if there are any deficiencies that were identified they need to be fixed.
If something does turn up positive on the investigations I mentioned above, it needs to be explored fully and completely. If the clinical picture does suggest an autoimmune issue, then low doses of hydroxychloroquine are used.
If anything changes in the scalp in terms of new symptoms, massively increased shedding, a repeat biopsy should also be considered.