Androgenetic alopecia or Telogen Efflvium ? What is my diagnosis?
QUESTON
I am female and in my early 20s. I have been crash dieting for the past 2 years (most extensively over the last 1 year). I was diagnosed with subclinical hypothyroidism in February although it was normal this month. HGB was 11.2. I’ve stopped my diets in March. Since then I’m experiencing a lot of hair fall, my hair comes out in my hands whenever I touch it, and when it shower there is a whole bunch of hair. I’m experiencing new hair growth, but my concern is my new hair falls out too.
I was told I have androgentic alopecia when I was around 16 year old and I was started on finasteride. But I wasn’t regular with taking my medicines. I got regular for the last 9 months. I experience pain in the scalp (hair roots) when I move my hair, especially at the crown and temples area (more after a headache) and this pain is associated with more hair loss. My medications are finasteride, biotin and B complex vitamins.
My new hairs fall out, and I’m really worried, if this will ever stop. I had really long and thick hair as a child, but I also have done a lot of hair straightening when I was losing weight. So I didn’t realize when did all this get aggravated. My hair is really scanty compared to the past.
Please advise what can I do. I tend to believe it’s because of a diagnosis of telogen effluvium
ANSWER
Many thanks for your question. I do think that you likely have androgenetic alopecia as one of the main reasons for your hair loss. I agree you could possibly have telogen effluvium but it is likely a much more minor contributor. It would be surprising with your history if it was a major contributor to the changes you have been experiencing since 15 years of age.
Let’s review all of this further.
However, before we go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s story
2) the findings uncovered during the process of the scalp examination including trichoscopy
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
I’d like to know a lot more about your story ideally but of course the magic of the “question of the week” is that I tackle questions with limited information.
So what is your diagnosis?
Based on what I have mentioned above, I can’t be 100 % confident of what’s going on entirely without seeing your scalp up close myself and knowing more about your entire story. However, I am of the opinion that the most likely diagnosis is androgenetic alopecia (AGA). There is quite likely a component of telogen effluvium (TE) too - so I agree wth you in that regard. However, I would suspect in your case that the main diagnosis is androgenetic alopecia.
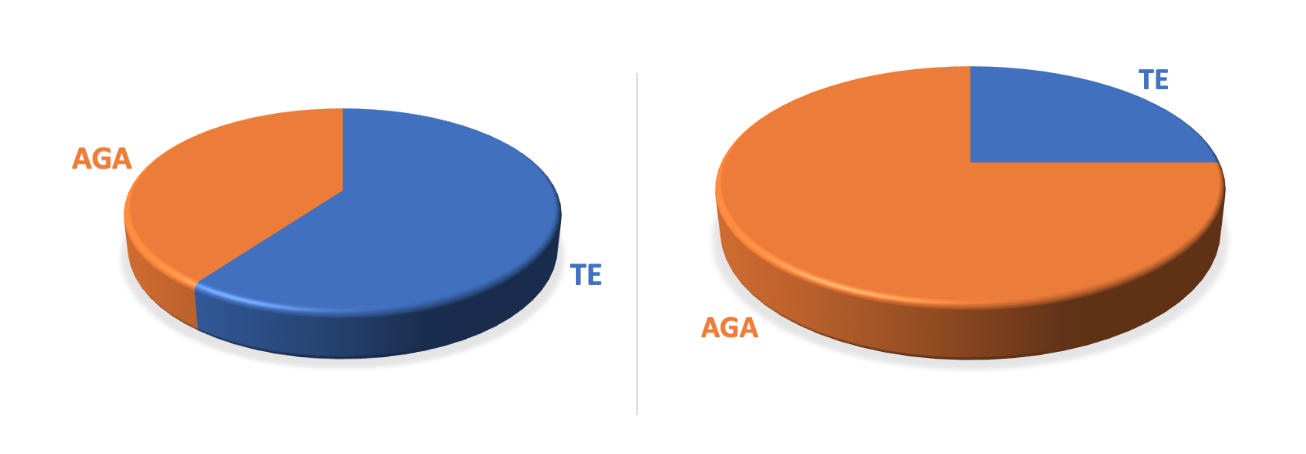
The challenge is knowing whether you have a bit of AGA and a lot of TE (like the pie chart diagram below on the left), or mostly AGA and a bit of TE (like the pie chart below on the right). I suspect you are mostly like the example on the right. Your doctors can help you figure out which diagnoses are present and whether the pie charts on the right or left are best representative of your hair.
It’s quite likely that with your history of hair loss since your mid teens and ongoing concerns that lead you to have very thin hair compared to the past that you do in fact have androgenetic alopecia. Your photos certainly suggest that anagenetic alopecia is present. Your hair loss does not appear to be completely diffuse in nature so there seems to be a component of localized “patterned” hair loss. Your reduction in central density with more preserved frontal hairline density (at the very front) is quite typical of androgenetic alopecia. It does appear there is a variation in the caliber of your hairs (or what is termed anisotrichosis) and this is very much in keeping with androgenetic alopecia.
It’s not impossible that you have telogen effluvium as well. You might possibly even have other diagnoses present as well. With your hemoglobin of 11.2 and fluctuations of thyroid hormones, and with the 2 years of dieting. it’s possible you have a telogen effluvium. Common causes of TE include stress, low iron, thyroid problems, medications, diets and illness in the body. You are your doctors can explore these and other potential triggers. It’s likely you do have a trigger but it’s unlikely you’ve had a TE for 6 or more years that just keeps going. But it may be a component of the hair loss and the TE may have made the underlying androgenetic alopecia (if present) worse. With a hemoglobin of 11.2, you will certainly want to speak to your doctors to determine what might be the cause. Low ferritin levels are one cause so you will want to speak to your doctor about these and other causes of low hemoglobin.
I do recommend that anyone with hair loss since the mid teens to have causes of hair loss thoroughly explored. You may have already had such a detailed “work up” or evaluation. It is important for adolescents and teenagers with androgenetic alopecia to have a hormone work up to evaluate for causes of increased androgens. Blood tests for testosterone and DHEAS are important and you yourself may have already had these ordered. All female adolescent patients with androgenetic alopecia and irregular periods that are still occurring at age 16, 17 and 18 years should be evaluated by their physicians to rule out polycystic ovarian syndrome (PCOS) as well as other hormonal issues like congenital adrenal hyperplasia (CAH). There are special blood tests that can be ordered.
See Article: Evaluating Patients with PCOS: What Blood Tests Should be Ordered?
Evaluation of PCOS in teenage patents can be more challenging and requires careful review of hair loss history, presence of acne, hair growth on the face, irregular periods and possibly ultrasound. Many healthy female adolescent patients who do not have a PCOS diagnosis have polycystic ovaries by ultrasound so the evaluation of possible PCOS in adolescents should involve a knowledgable specialist.
With your current mediations being finasteride, some of the hormone tests may be inaccurate by simple fact you are on these drugs but it may still be worth discussing these diagnoses with your specialists if they have not been discussed before. If your periods have been irregular, you will want to discuss whether PCOS could be a part of your diagnoses. If your periods have always been regular and you have not had increased androgens in your blood tests, and yo have no have acne and hair growth on the face then your specialists may feel that PCOS is not a consideration.
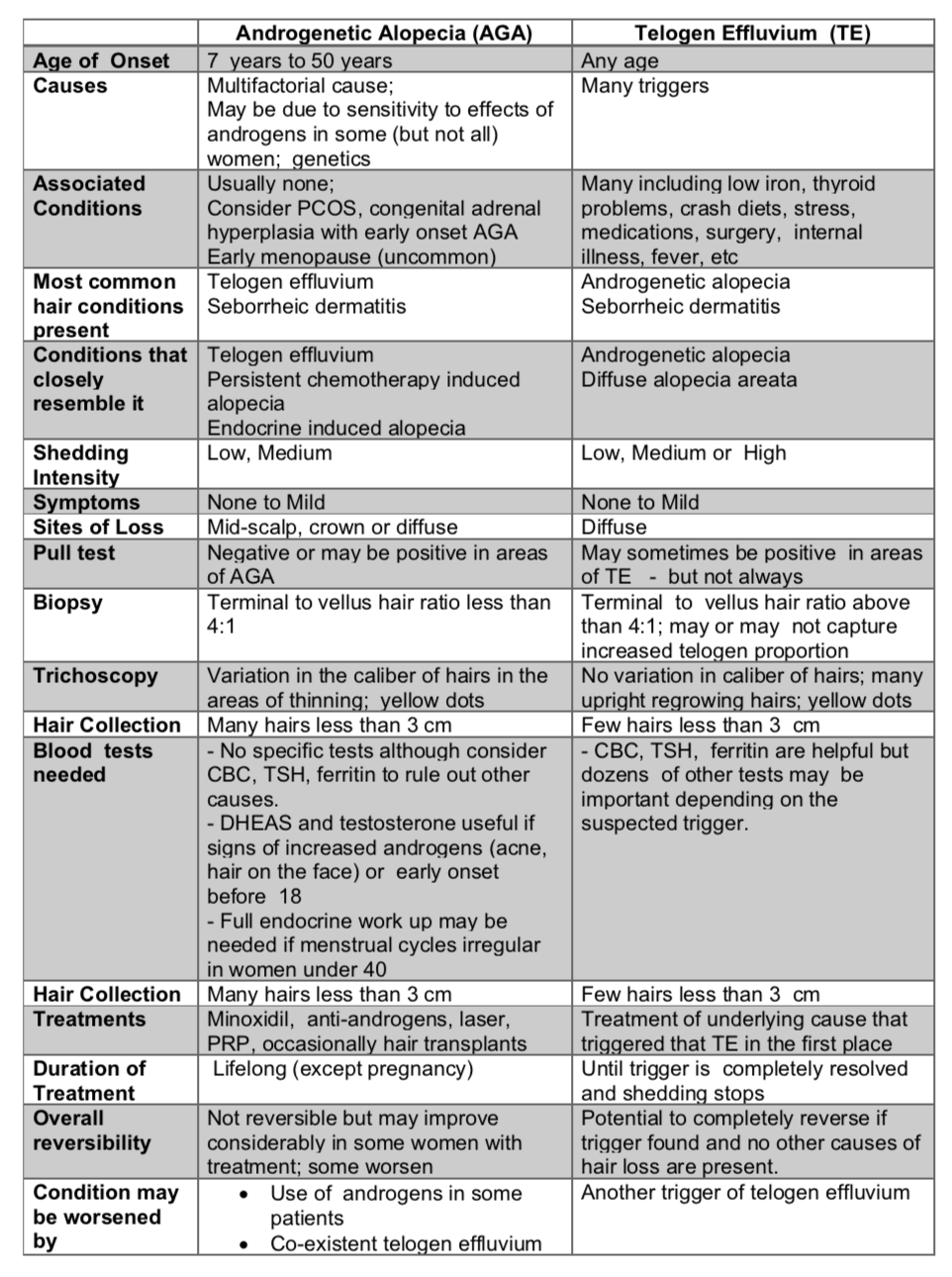
Differentiating Androgenetic Alopecia from Telogen Effluvium
I have included a comprehensive table below that compares feature of AGA and TE. In young women, TE and AGA have many features that overlap and mimic each other. Mild symptoms can be present in both although often other explanations like seborrheic dermatitis best fit with the reason for the patent to have symptoms. YOu’ll want to have all areas of your scalp carefully examined by trichoscopy to determine the specific reason.
There are several ways that your physicians can help solidify the diagnosis for you. In AGA, the story may suggest hair loss from the central scalp but sometimes if TE is also present the story appears confusing because some hair loss is also diffuse. AGA can give shedding and so can TE. Massive amounts of shedding are not seen in AGA. Trichoscopy can be performed by your doctors. In AGA, trichsocopy shows a variation in the size of hairs (as mentioned above). In TE, this variation is not present. A biopsy can be extremely helpful in your case if doubt still exists in your mind or the mind of your specialists. A terminal to vellus hair ratio of less than 4:1 on the biopsy suggests a diagnosis of AGA. This simply means the the biopsy captures a large proportion of vellus (tiny) hairs which is a feature of AGA. If a person does need a biopsy, it’s important that it be taken from the middle of the scalp as this is where the diagnosis of AGA is most accurate in women.
If you don’t wish to have a biopsy, a modified hair was test can be helpful to document the number of hairs and the proportion of small hairs. A high proportion of short 3 cm hairs by the modified wash test suggests a possible diagnosis of AGA.
Summary
I hope this helps, and thank you again for the question. I would appear that AGA is at least one of your diagnoses and TE could be too. A good history, examination of the scalp (with trichoscopy) and review of all your blood tests can help confirm the diagnosis. If there is any doubt, a scalp biopsy can be helpful.
You are right that TE may be present with your diet and low HGB. I would be surprised if TE was having the greater contribution compared to AGA with the story you have given.
If AGA is what you do have, you may wish to review all the options including minoxidil, laser, platelet rich plasma and other antiandrogens. Oral contraceptive are important considerations if PCOS is present. One must always remember that women using finasteride must never become pregnant while using this medication. Hair transplantation can be an option for some women but it may not be a good option if you hair loss is diffuse. Many females with early onset AGA are not good candidates for hair transplantation due to the diffuse nature of the hair loss.