Could my scalp biopsy be wrong?
By biopsy says I have Androgenetic Alopecia, but I don’t think so
I’ve selected this question below for this week’s question of the week. It allows us to review some concepts regarding the diagnosis of androgenetic alopecia.
Question
I’m a 23 year old female and shedding a lot of hair. I went to see 2 dermatologists and both were sure I have telogen effluvium but my scalp biopsy just returned saying I have androgenetic alopecia. It makes no sense to me or my doctors. Could the biopsy be wrong? I recently started a new job and have been super stressed. I lost 5 pounds and my ferritin was low at 34. Does it not sound like a telogen effluvium to you?
Answer
Thanks for the great question.
First off, it’s certainly possible a biopsy can be wrong. Your story does not carry a strong suspicion that your scalp biopsy is wrong, but certainly it could be. I don’t know your full story and I have not examined your scalp or seen your blood tests or biopsy results so I can’t really tell you what you have. There is only one way for me to tell you what diagnosis you have and that is by following the proper steps: I need to know the story, see that scalp and review the tests.
But how does androgenetic hair loss start out in many women? Well, with lots of shedding. What is the most common diagnosis that doctors miss in women who come into the office with concerns about shedding? Androgenetic alopecia.
I would need to know more about your story and see your scalp up close and see your biopsy results myself to say it your biopsy is wrong or not. If the terminal to vellus hair ratio on your biopsy result is less than 4:1 and telogen proportion is less than 12 % it is unlikely you are dealing with TE and more likely AGA.
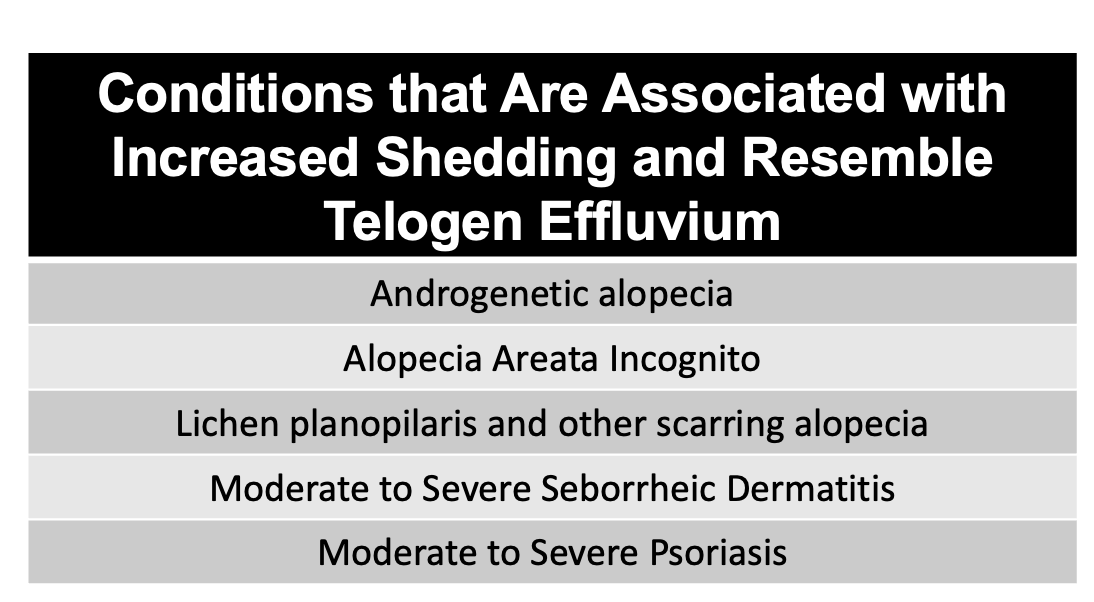
Conditions that Resemble Telogen Effluvium
Every day of my practice, I see patients who think they have telogen effluvium, or were told they have telogen effluvium but they don’t actually have telogen effluvium!
How can this be?
Well, many hair loss conditions given increased hair shedding. Unless a person knows all the features of these various other conditions and knows how to properly diagnosis them, it’s quite normal that the diagnosis will end up being ….. telogen effluvium.
Zebras, moose, reindeer and camels all sort of look like horses. Unless a person knows a thing or two about zebras, moose, cows, reindeer and camels, it’s understandable that he or she is going to call them a horse when they see them.
A wide variety of conditions are associated with increased shedding, including telogen effluvium, androgenetic alopecia, scarring alopecia (ie lichen planopilaris), and moderate to severe inflammatory scalp disease (such as psoriasis, seborrheic dermatitis and others).
Unless you know a thing or two about the proper diagnosis of androgenetic alpecia, lichen planopilaris, and other conditions, it’s understandable to default back to thinking shedding automatically equates to a diagnosis of telogen effluvium.
Well, it doesn’t.
Androgenetic alopecia presents with hair shedding. THere may not be any of the famous ‘miniaturization’ that people love to talk about in the early stages. The part width may or may not be widened but it usually is and the frontal part is a bit wider than the back. Trichoscopy (a magnification technique) is helpful to show the variation in hair caliber that is developing but sometimes it’s subtle in early stages. A biopsy (if done with horizontal section) can capture that the terminal to vellus ratio is dropped from the normal 7:1 down to under 4:1. Oil glands (sebaceous glands) are preserved and not reduced in any way. The proportion of telogen hairs in the biopsy is under 15 %.
Lichen planopilaris can look like androgenetic alopecia. Often the scalp is a bit red or pink and the patient has symptoms like itching, burning or tenderness. In the early stages, it’s quite subtle sometimes, The number one concern of the patient may be the increased shedding but often it’s that the scalp it itchy or burns in some unexpected manner. Trichoscopy (a magnification technique) again helps solidify the diagnosis in most cases. A biopsy shows that oil glands are disappearing (reduced) and may show that the hair follicle is under attack with inflammation and some hair cells are dying (a finding call lichenoid inflammation and necrosis).
Alopecia areata incognito looks just like telogen effluvium sometimes. In fact, it’s really better that we call this condition alopecia areata telogenica so we don’t forget it. Many people think of alopecia areata as a condition that causes hair loss is patches, or circles. That’s is true for many patients but that’s only one form of alopecia areata. Another form of alopecia areata is a rarer form that just causes loss of telogen hairs. Trichoscopy might show abnormally shaped hairs and empty tracts but often does not show the classic features that doctors learn about alpecia areata (like famous exclamation mark hairs). A biopsy will capture the well known inflammation at the bottom of the biopsy in an area of the follicle call the bulb.
Seborrheic dermatitis often doesn’t cause all that much shedding. The exception is when it’s severe enough. When it’s severe enough, seborrheic dermatitis certainly does cause shedding. In some ways this is a secondary telogen effluvium but the primary disease is the seborrheic dermatitis. Any inflammatory scalp condition can cause this including psoriasis and severe allergic contact dermatitis.
Conclusion
The most common misdiagnosis in women is androgenetic alopecia. I can’t say what you have but it does seem there is a lot of evidence pointing to androgenetic alopecia. If the history, examination, trichoscopy findings and biopsy all point to a diagnosis of androgenetic alopecia, then the diagnosis is AGA.
It’s normal to focus on iron as the cause of the shedding. A ferritin of 34 is probably not a major cause of shedding for most women. OF course, you’ll want to review prior ferritin levels and speak to your doctor about what your hemoglobin level is and how it too has been changing and perhaps give iron supplementation a go, but a ferritin of 34 doesn’t give shedding for 85 % to 90% of women.