Q6. Do you have acne or excessive hair growth elsewhere?
As we evaluate hair loss, it important to get a sense if there are clinical signs of hyperandrogenism (high androgens). Having hyperandrogenism does not necessarily mean the patient has AGA but does increase the odds just that much more.
Acne and hirsutism are two of the more important signs to enquire about. If there is any clinical evidence of hyperandrogenism, it will be important to have blood tests for testosterone and DHEAS. Only 10 % of women with AGA have hyperandrogenism so the finding of normal hormone levels still makes AGA possible. In addition, many women with hyperandrogenism do not have AGA at all so this is just a fact that gets considered as part of the bigger picture.
PART 2: IS THERE EVIDENCE TO SUPPORT A DIAGNOSIS OF ONGOING TELOGEN EFFLUVIUM?
It’s clear that a telogen effluvium was present in the past for you. The key question now is whether there is some kind of ongoing TE. The causes of telogen effluvium include stress, low iron, thyroid problems, medications, diets, systemic illness. So we need to understand more about these potential issues or ‘triggers’ for anyone who is shedding. In CTE, shedding can occur without a clear trigger.
Q7. Did you start and stop other medications or supplements?
Why do I need to know? Other medications and supplements can trigger shedding. Even taking some medications and herbal medications can give an ongoing shedding. I’m assuming in this scenario that minoxidil is the only product used. Clearly, if other products are used they need to be considered.
Q8. Have you had eyebrow changes, eyelashes changes, body hair changes, nail changes?
Why do I need to know? Eyebrow and eyelash changes and body hair changes don’t occur as part of AGA but can occur in TE. They can also occur in other immune based conditions. I am not suspecting any immune based issues but certainly it would be quite unexpected if you were experiencing a lot of body hair loss. If there was any eyebrow or eyelash loss, the key is to figure out if it affects both the right and left side symmetrically or whether one side is affected more. Eyebrows and eyelashes can reduce in density from telogen effluvium, alopecia areata, trichotillomania, seborrheic dermatitis as well as cicatricial alopecia (and other conditions). It would not be surprising if you have some minor eyebrow changes over the last 3 years but it should be quite symmetrical. If you do have eyebrow changes, some of the eyebrow changes could be due to the hypothyroidism.
Similarly, if there was an increase in body hair this too would be unexpected here and a possible sign of increased androgens. Increased hair on the thighs, abdomen and nipples can be a sign of hyperandrogenism and raise suspicions for PCOS (even if periods are regular). I would think that it issei's quite unlikely you would report this to be the case. This would be information that your doctors should confirm.
Q9. Have you had weight loss or weight gain? What is the current weight?
In the setting of a likely telogen effluvium, it’s important to know whether there has been weight loss that could be triggering a telogen effluvium. In addition, we need to make sure that your current weight is high enough (i.e. BMI is above 18) otherwise the result can be an ongoing TE from poor nutritional status.
In addition, weight loss and weight gain can be reflective of underlying medical conditions. So, if weight has fluctuated either way, it could be important.
Q10. Do you have any scalp itching, burning or tenderness?
Scalp symptoms are important to know for every single patient. Your scalp looks quite healthy so I would be surprised to learn there is any itching or burning or tenderness. I’m usually not too worried about a slight among of itching from time to time, but if there was burning or tenderness in the scalp, that would be worrisome. I don’t think this is very likely to be relevant here for your case but we need to always keep in mind that there are conditions that mimic telogen effluvium.
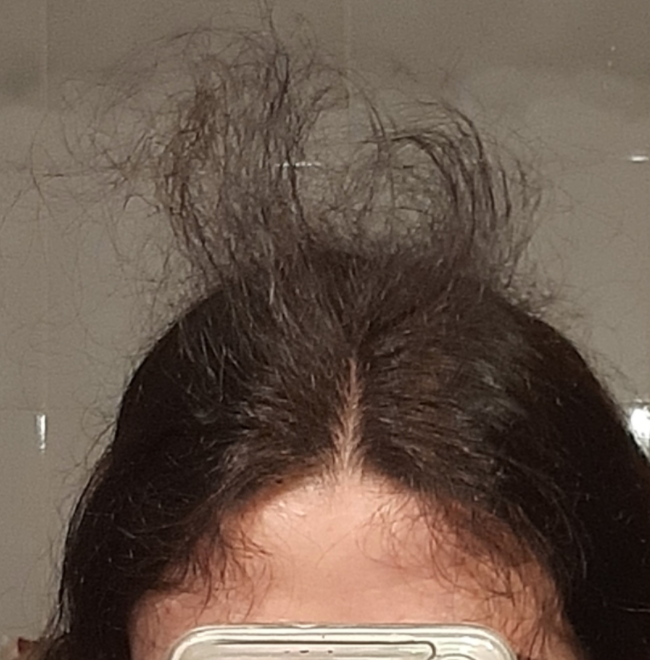
Q11. Do you feel you are getting hair breakage?
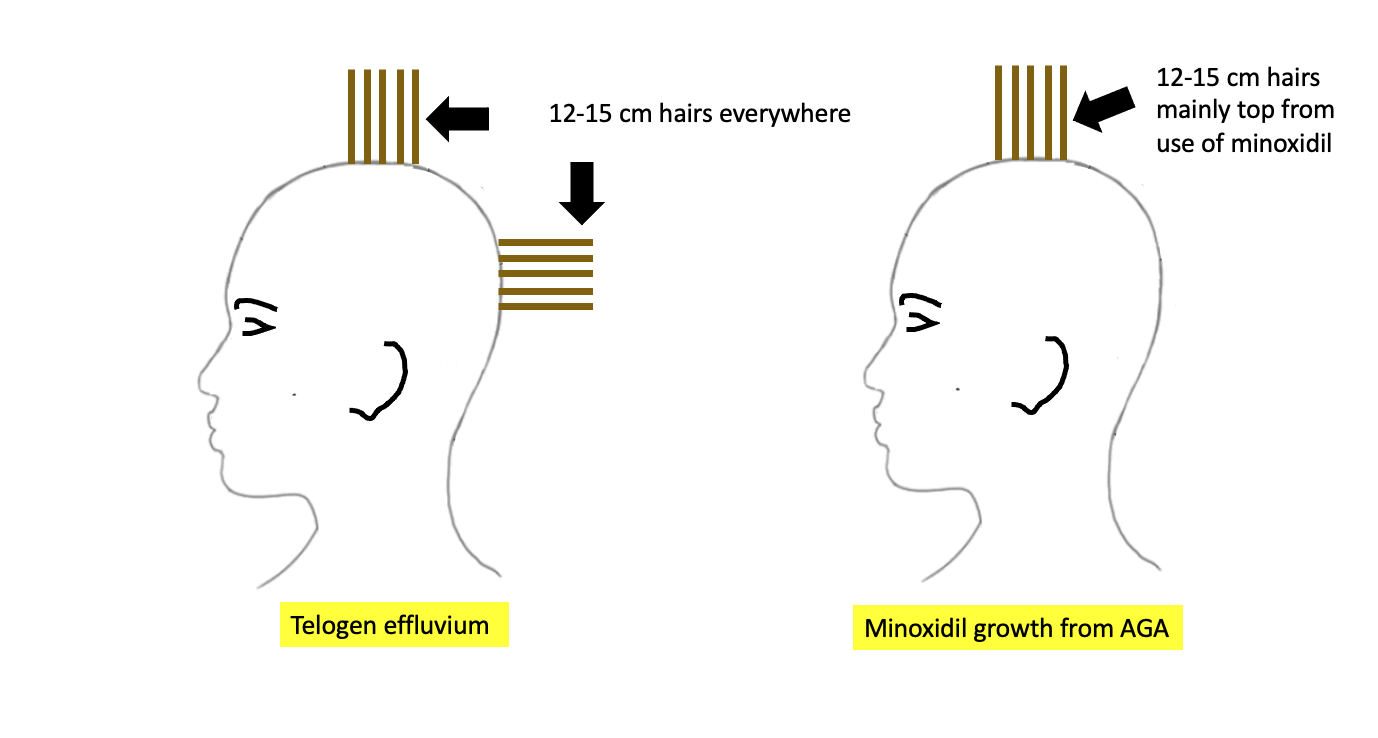
I am not appreciating much in the way of hair breakage, but it’s important to inquire about. Some patients confuse hair breakage with actual new growth so what you are seeing on the top of the scalp appears to be new growth. It’s not uncommon for patients to exclaim - “look at all my hair breakage!” In your case, this is not breakage from what I can see. However, if you felt there truly was increased breakage that would need further exploration. Breakage can come from heat and chemicals and can give the feeling of ongoing shedding and loss. A proper examination can completely exclude breakage, but I would be surprised if that’s even an issue here. your scalp and hair are healthy.
Q12. How low your ferritin dropped over this period ?
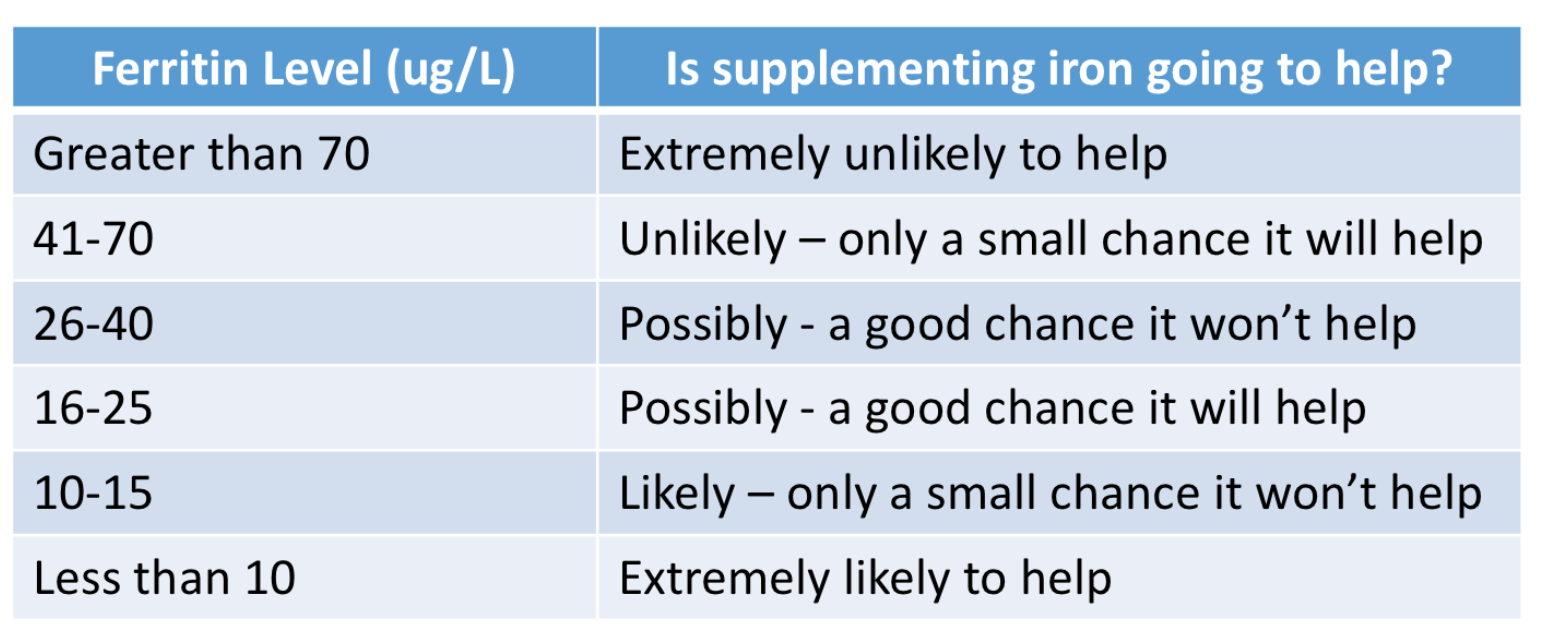
I understand that you have a history of low ferritin. It will be important to know what your ferritin level is right NOW. That is what will be relevant to ongoing shedding. A ferritin of 10 is likely associated with hair loss. A ferritin of 40 is probably not. Therefore, it will be important to know what the ferritin level is now and how it’s been changing over the last few years.
is it possible you’ve had a ferritin of 22 and it’s been responsible for your shedding for three years? Perhaps. The higher your ferritin level - the less likely it is that your iron is the culprit in your hair loss. But you have not given me the number so I don’t know the current level.
Certainly, if you have a ferritin less than 15, it’s probably a problem and probably one of the reasons why your hair is shedding. Taking iron supplements in these situations has a high likelihood of helping. However if your ferritin is currently 40, 50 or 60, it’s less likely that you currently have an iron problem.
Most women need ferritin levels in the 30-40 range for healthy hair. However, some women definitely need those levels to be higher than that and into the 50 - 70 range. If you have a history of low ferritin, it will be important for your doctors to review why you have low ferritin and how the levels have been changing over time and what they are now. Many women have low ferritin levels. However, when low ferritin is combined with low hemoglobin (which we call iron deficiency anemia) I’m much more concerned. Excessive bleeding from menstrual cycles, poor diet, celiac disease, gastrointestinal issues all need to be explored.
The following table gives an estimate of how likely it is that taking iron supplements will help your hair according to the ferritin levels.