Still losing hair despite my biopsy showing I have end stage scarring alopecia: Why?
Why does my biopsy show I’m end stage yet my hair loss is continuing?
I’ve selected this question below for this week’s question of the week. It allows us to discuss the important concept of end stage scarring alopecia and how it differs from “burnt out”. Here is the question….
QUESTION
Dr. Donovan, I’m 63 years old and I was recently diagnosed with something called end stage scarring alopecia. My doctor says I won’t get back my hair but says the good news is that my disease is over now and that I don’t need any sort of treatment to stop it from getting worse. In other words, the feeling is that the disease came and went. I find this hard to believe because I’m still losing more and more hair! Can you please help us understand what this disease is all about and what you recommend in these cases?
ANSWER
Thanks for the question.
Your question is a good one. I’d need to know more about your story to figure out if you’re losing hair still on account of the scarring alopecia or something else. If you are losing hair on account of something else, then yes - your doctor is right. You might not need treatment for the scarring alopecia component. But you would need treatment for the “other diagnosis.” I’d need to see your scalp and review your whole story to figure out the “other component.”
However, many times, patients with a diagnosis of end stage scarring alopecia are losing hair because of their scarring alopecia.
Let’s take a look at what end stage scarring alopecia - is and more importantly what it is not.
End stage scarring alopecia (ESSA) is term that’s often confused. It’s a term that pathologists use when describing biopsies of scarring alopecia that are so far advanced that one can no longer tell what kind of scarring alopecia that patient has. Inflammation is generally no longer present in the specimen so all the valuable diagnostic clues are gone. For example, the pathologist cannot tell if it’s lichen planopilaris or discoid lupus or folliculitis decalvans.
They can however tell it’s a type of scarring alopecia - but that’s where their help ends.
I dislike the term “end stage scarring alopecia” quite a bit because it generally causes more harm than good to many patients with hair loss. So many patients come to see me after losing hair simply because a biopsy told them their disease was end stage. The dermatologist figured that treatment was no longer needed and treatment was stopped. In some cases, treatment was not started because of this result.
A Common Mistake in the Management of End Stage Scarring Alopecia.
Let’s look together at a very common scenario I see - it mimics your story almost perfectly.
Step 1: A sample is taken from the scalp and submitted to the pathologist for processing.
Step 2: The pathologist looks down the microscope and see massive amounts of scarring and little in the way of inflammation and concludes it’s ESSA. Clues are missing. The pathologist assumes inflammation was once present in that area of the skin but now the disease is so far advanced that all clues are gone. Usually the report goes on to say that the disease is end stage and burnt out.
Step 3: The dermatologist gets the report and says “Oh my patient’s disease is no longer active”
Step 4: The patient and dermatologist share in the excitement that treatment is no longer needed because the disease is thought to be burnt out. The patient leaves the clinic and stops medications.
Step 5: The patient returns back to clinic in 7 months with more hair loss.
A Very Simple Way to Generate Better Outcomes in The Diagnosis of End Stage Scarring Alopecia (ESSA).
Your question is so important. We need to put an end the days when end stage means an end to treatment. This common view is sometimes simply not correct.
There is only one way to really know if a patient’s scarring alopecia is quiet and inactive and truly burnt out. It’s so simple too: a camera! If photos are taken 1 year apart (even better if two years ago) and show no changes in hair density and the patent has no symptoms and the patient’s shedding is low and there is minimal redness - the scarring alopecia is likely burnt out.
So here’s how the scenario really show play out:
Step 1: A sample is taken from the scalp and submitted to the pathologist for processing.
Step 2: The pathologist looks down the microscope and see massive amounts of scarring and little in the way of inflammation and concludes it’s ESSA. Clues are missing. The pathologist assumes inflammation was once present in that area of the skin but now the disease is so far advanced that all clues are gone.
Step 3: The pathologist generates this report:
“The histological findings here support a diagnosis of advanced scarring alopecia. The pathological findings in the current specimen that was submitted are advanced to such a degree that it is not possible to differentiate this scarring alopecia into a specific subtype type (lymphocytic, neutrophilic, etc). This has traditionally been called end stage scarring alopecia in the past. Clinicopathological correlation is needed to accurately determine if these histological findings actually imply inactive disease (ie. so called burnt out scarring alopecia) or whether the patient may in fact have ongoing and progressive hair loss in this or other areas of the scalp. The clinician is advised to take note that histological findings of end stage disease may not always correlate with the patient’s disease truly being burnt out. Close monitoring is advised.”
Step 4: The dermatologist gets the report and says “Oh my patient’s disease seems end stage - I’m going to follow him or her closely and see if this is what’s really happening in the scalp or not”
Step 5: The patient and dermatologist review the unknowns of ESSA. Photos are taken before leaving with a plan for the patient to return in a defined period. The patient may or may not continue treatment.
Step 6: The patient returns back to clinic in a defined period for review of photos, symptoms and signs (shedding, redness).
Step 7: A decision is made but the clinician as to whether the scarring alopecia really is “burnt out.”
Summary and Conclusion:
I appreciated your question. I can’t say whether your scarring alopecia is burnt out. This requires a clinical evaluation. If you are losing hair because you have a thyroid disorder then yes, it’s possible your scarring alopecia is burnt out and you now need to address the thyroid disorder. However, it’s certainly possible that the scarring alopecia is not truly burnt out despite a biopsy coming back showing end stage scarring alopecia. A biopsy is just a piece of the skin. It could be that a sample take from another area shows disease activity. Or it could be that the biopsy truly is lacking inflammation but other disease processes that go along with the scarring alopecia are causing the hair to be progressively lost.
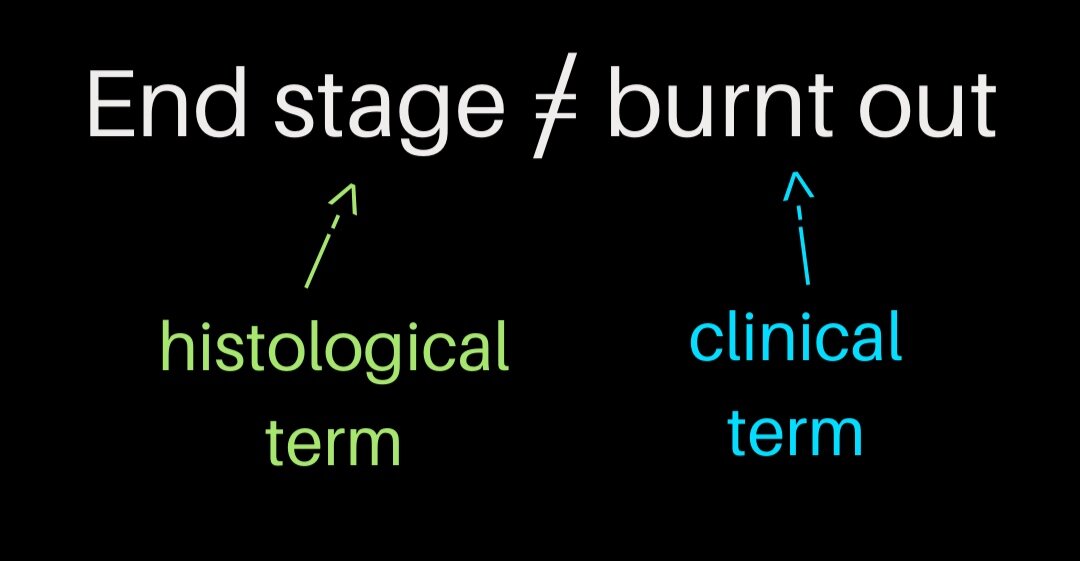
End stage scarring alopecia is a pathological term. It is best made in the pathology department. Burnt out is a clinical term - it is best made in the clinic with the patient in front of the doctor.