Daily Shedding... with high DHEAS.... What should I be doing?
Why am I still shedding ?
I’ve selected this question below for this week’s question of the week. It allows us to discuss shedding issues in young women with high DHEAS.
QUESTION.
Dr. Donovan, I'm hoping you may be able to shed some light onto my hair shedding situation. I started experiencing increased hair shedding 6 months ago. Prior to the shedding, I'd started a birth control pill (low androgen) 2.5 months before, and Spironolactone 5.5 months before (for hirsutism). I experienced mild stress but it was nothing out of the ordinary. A month into the shedding, I began to experience tingling, crawling, and pain in my scalp. 1.5 months after the hair loss started, I went off of Spironolactone, and 2.5 months into the shedding, I went off birth control. My scalp became itchy as well.
I went to 3 dermatologists, all of whom diagnosed me with telogen effluvium. I recently had a biopsy done that stated telogen effluvium as well. I was also diagnosed with seborrheic dermatitis (which I've never had before in my life). I tried ketoconazole shampoo. I've had blood work done that stated my thyroid was normal, ferritin within normal range, (was 95 in October due to brief supplementation and then 26 in January), and I was deficient in vitamin D. My vitamin B12 level was too high, I'm not sure what that means.
I have symptoms of androgen excess (acne and excess hair growth on my face / body), dating back to my teen years (17), I'm 21 now, soon to be 22. The facial hair growth appeared in November of 2019 at age 20. I have elevated DHEAs (512), and had an ultrasound ruling out PCOS (no irregular periods, no polycystic ovaries).
Photo of the patient’s scalp.
Since the hair shedding began, I experienced massive emotional stress as a result. I was diagnosed with anxiety and depression - which I'm sure I've had for years but got extremely bad once my hair started to fall out. I am thin (weighing only 104lbs) but lost 10 pounds presumably due to stress of the hair loss. I've had two episodes of what was probably telogen effluvium in the past - one was related to low iron (ferritin of 7) back when I was 15, and one episode when I was 18 most likely due to a bad case of the flu. Those episodes only lasted 3-6 months and I grew all of my hair back.
This time, I've been consistently shedding for 6 months with no sign of improvement. My scalp is very tender, sensitive, flaky and itchy still. On an average day, I used to shed maybe 5-10 hairs, now I am shedding roughly 50-150 hairs - which is not normal for me. I'm at a loss for what could be causing this and what I can do about it. Any advice would be greatly appreciated
ANSWER
Thanks for the question.
I’d like to discuss several important things in the question you ask and the information you have submitted.
Before we do go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s story
2) the findings uncovered during the process of the scalp examination including trichoscopy
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
There is lots more to your story that I need. I would want to know about other medications you have started and stopped. I would want to know about other symptoms like joint pains, headaches, fatigue, weight loss, eyebrow changes, eyelashes changes, body hair changes, nail changes, and rashes.
The 2 key questions here in your case are:
a) Is the diagnosis ONLY telogen effluvium … and …. if so what is the trigger?
b) Is this a telogen effluvium with the starting stages of androgenetic alopecia?
Let’s go further into your story.
POINT 1. Many people who take birth control pills shed for the first few months.
First, I think there’s little doubt that at least one of your diagnoses is telogen effluvium. We don’t actually need to debate that. The debate we will get into in a moment is whether anything else is going on.
You have several reasons why you could have a telogen effluvium, including starting the birth control pill and starting spironolactone. A large proportion of women shed when starting these treatments, especially birth control pills. The shedding starts 2-3 months after taking the first pill and the shedding lasts 3-6 months provided the pill is continued every day. A lot of women shed when stopping these pills too, especially the birth control pill. The shedding starts 2-3 months after stopping the pill and the shedding lasts 3-6 months provided the pill is not restarted.
So what would I expect to hear from a 21 year old woman who starts spironolactone and then starts a birth control pill? Shedding.
And what would I expect to hear from a 21 year old woman who starts spironolactone and then starts a birth control pill and then stops these pills? Shedding.
What is your story? Shedding.
So in some ways, it’s possible this is entirely consistent with your story.
POINT 2: All patients with hair loss, acne and hirsutism and androgen excess need a proper work up. A work up should be done off birth control.
You have DHEAS 512 (which is 13.9 umol/L in SI units). Any female age 21 with DHEAS 512 and acne and hirsutism and hair loss needs a thorough endocrine work up in my opinion. We need to rule out PCOS and late onset CAH.
With the limited information you have provided here, it would be false to say that you “don’t” have PCOS.
The correct way to say it is more likely “you have a low likelihood of having PCOS.”
Women with PCOS who are thin with low BMI often have regular periods and often have no cysts visualized on ultrasound examinations … but still have elevated androgens. This is a bit more advanced type of knowledge, but I think it’s important especially since you have hyperandrogenism. Anyone who claims there is zero chance you have PCOS is wrong. Anyone who thinks there is a very low chance you have PCOS is correct. I have seen many women with your story exactly who go from being thin to being heavier in their 20s and 30s and ‘develop’ PCOS. I’m not saying that is your case, but sometimes weight gain brings about insulin resistance that then promotes a fuller PCOS clinical presentation.
So what work up do you need? Well, I would advise a proper work up on day 3-5 of your cycle for my own patients that come to see me with a story like yours. The fact that you are off birth control again is a good time to do this. We can’t do these tests when women are on birth control.
The tests that I order on day 3-5 of the cycle for my patients with similar stories are: LH, FSH, estradiol, testosterone, free testosterone, SHBG, glucose, insulin, hemoglobin 1A1c, AM cortisol, prolactin, androstenedione and 17 hydroxyprogesterone, AST, ALT, and cholesterol. These should be done fasting and day 3-5 of the cycle. You have already had your DHEAS measured so there is not a lot of good reason to do this again unless someone suspected levels could be climbing. I would probably include it again for completeness.
What am I looking for in these tests?
a) a high 17 OHP level on day 3-5 that would lead us to a diagnosis of late onset congenital adrenal hyperplasia
b) a high testosterone, high fasting insulin, high LH that would point is towards a PCOS like state
c) A normal prolactin and AM cortisol that reassures us that no other issues are present
In your case, I would want more blood tests if I was your doctor. I would want to know if there is any evidence of insulin resistance that would push me towards PCOS. I would want to know if the other hormones were normal. I would want to know your free testosterone and SHBG. I would want to know your 17 OHP levels to rule out late onset congenital adrenal hyperplasia before moving on.
POINT 3: When it comes to ultrasound examinations, there is a lot that patients don’t realize.
When I hear that a patient had an ultrasound that showed no cysts, my first response is usually that I’m glad to hear that news. But there are a few points to keep in mind. First, it depends on whether the ultrasound examination was a transabdominal ultrasound or transvaginal. There is a big difference in the quality of the studies and what it all means. Transvaginal studies with modern ultrasound techniques are the most helpful. Many people don’t have these studies done. Transvaginal studies can pick up a lot of cysts that the transabdominal can not. Of course, it’s very unlikely this is even an issue with your story but it’s something that we need to keep in mind.
With your ultrasound, I would want to know where it was done (what center? what clinic?) and whether it was transabdominal or transvaginal? What was the volume of the ovaries noted in the report ? Were any ovary measurements more than 10 mL ?
POINT 4: In the early stages of hair loss, TE and AGA can look the same and have the same story. Rarely, they can have a similar biopsy too.
When I look at your photos, I immediately say to myself :
Could this person have AGA?
Could this person have TE?
Could this person have both conditions?
(Also …. whenever we use the word TE, we need to immediate shout out hey could this be diffuse alopecia areata …. but I don’t think that’s what this is. But I include this for completeness of this write up).
In the early stages TE and AGA look the same. Of course, an up close examination with use of trichoscopy is going to help in your situation. In fact, it’s critical this be done! If the back of the scalp is convincingly thicker than the front of the scalp, I am pushed more towards thinking this could be AGA (with your TE). If the back and front areas are similar density, we are more likely thinking about a sole diagnosis of isolate TE. If there is no evidence of “follicular miniaturization” or variation in the caliber of your hairs when your scalp is examined with trichoscopy, we are likely dealing with an isolated TE. If there is a convincing variation in the caliber of hairs, it could be an early AGA.
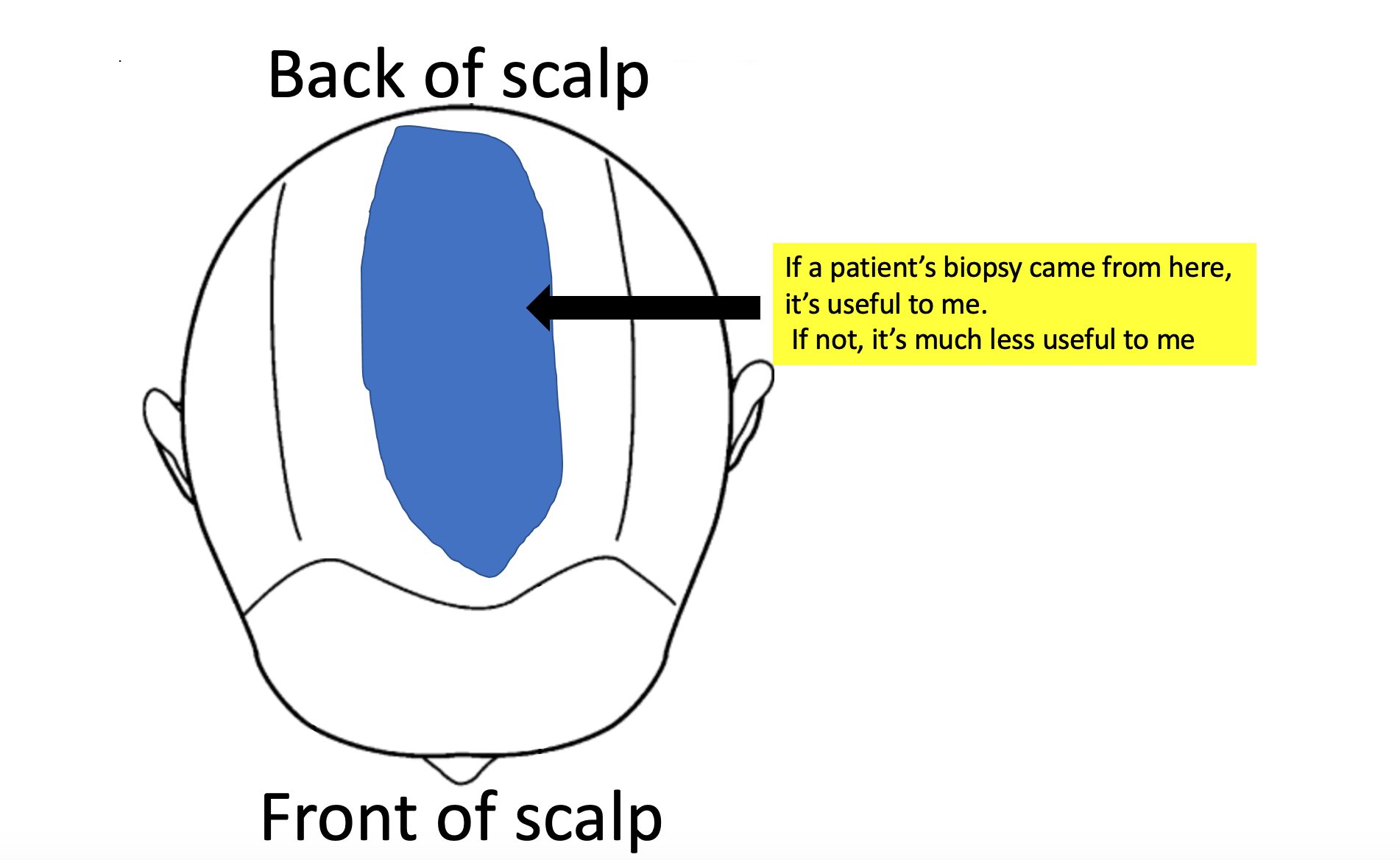
Biopsies can be tricky. There is so much more to doing a biopsy than just doing it and so much more to interpreting a biopsy than just reading the information that comes printed on report. My ability to accurately interpret a biopsy depends where on the scalp it was taken from!. It depends how it was processed (horizontal vs vertical section). It depends who read the biopsy (dermpath vs general path). If a biopsy was taken from the sides or the back or somewhere just to prevent the patient from having a visible scar, then the biopsy is often useless. Biopsies in your case need to come from the top.
Here is where I would need your biopsy to have been taken from for me to feel better about the situation:
Also, if someone is going to tell me all you have in your biopsy is a telogen effluvium, I’m going to hope that horizontal sections were used. It’s a huge stretch to diagnose a telogen effluvium confidently from vertical sections. In horizontal sections, the pathologist gets to see 20-40 hairs in order to give their best guess about what could be going on with the rest of the scalp. With vertical sectioned biopsies, they just get to see 3-6 hairs. I don’t want to leave my patient’s hair loss diagnosis to interpretations as to what is seen with 3-6 hairs.
POINT 5: TE and seborrheic dermatitis (and sometimes even AGA) give tingling and symptoms.
With the biopsy result you have in your possession, I’m much much less worried about the tingling, crawling and pain. Of course, I wish you did not have it. But I’m not suspecting anything inflammatory that would make me want to act with a much different course. This is assuming your biopsy came from an area that was tender) I’m always worried when a patient says they have scalp pain. But this worry evaporates to a large degree when the biopsy from that area shows non-scarring alopecia. If your biopsy was from a random area and not from a tender area, then it becomes more difficult to interpret what it means.
Pain and tingling in your case can come from seborrheic dermatitis. it can come from TE, It can come from depression. It can come from allergy or irritation from a current shampoo. it can come from irritation of allergy from other cosmetics.
We still need to keep an eye on this pain. I often encourage my patients to commit to treating their seborrheic dermatitis with a rotating schedule of shampoos. Zinc pyrithione one day. Ketoconazole the next regular shampooing day and selenium sulphide shampoo the next shampooing day. Shampooing must be done 2-3 times per week and left on 2 minutes. I advise my patients to not over do the time as this often just dries the hair and scalp out further. Also, putting a prescription topical steroid on the scalp like betamethasone valerate lotion 0.1 % aa few times per week right after showering is often helpful (of before bed). 10 drops to 15 drops of betamethasone valerate lotion two times per week for a few months is very safe and anyone who says otherwise has little understanding, knowledge or training in the area.
If the pain is still present in 3-5 months, this needs to be looked into further.
POINT 6: What to do next depends on the blood test results and your prior response to spironolactone.
What exactly to do next and how do help your shedding depends partly on your next set of blood test results. If you have elevated 17 OHP on your blood tests, you may want to see an endocrinologist. If you have high LH or evidence of insulin resistance you’ll want to see a really experienced endocrinologist for evaluation of PCOS. Not all women with PCOS are overweight and in fact, women with PCOS who are thinner or have low body mass index often have regular periods and no cysts on ultrasound.
If you tolerated spironolactone well (in the past) and tolerated birth control well, it may even be an option to return to these and stay on these. Did it control your acne? Did it stop hirsutism? Did you feel good on it? Anyone starting these medications has a chance to get shedding so I’m not necessarily worried by a story of shedding. You stopped too soon to really get any sense what the long term outcome was. If there is any evidence of AGA with an up close examination, this could be a good option again. If not, you might want to treat your acne and hirsutism differently - perhaps topically.. The other option is to wait longer in hopes the TE resolves. Continuing iron and vitamin D and shampooing your hair diligently with these anti dandruff shampoos is going to be important no matter what is going on up on the scalp.
Finally, with any TE, we need to always keep in mind that maybe we have not found the trigger. If your ferritin was low and your hemoglobin was low (less than 12.0), a work up could be important. I often test for example a celiac panel in patients with BOTH low HGB and low ferritin. I’m not worried about your high B12. I would want to know about other medications you have started and stopped. As mentioned above, I would want to know about other symptoms like joint pains, headaches, fatigue, weight loss, eyebrow changes, eyelashes changes, body hair changes, nail changes, and rashes. Sometimes we consider ordering autoimmune tests in women with shedding but only if the history points us to ordering these. Ordering these tests ‘just to cover all bases’ is usually not a good idea.
Summary
I can instantly tell by your question that you’ve read a lot and thought a lot about your issues and what all this information means. Congratulations for that. That is important. You need to figure out if late onset CAH is a possibility or not ….. and whether insulin resistance/PCOS its truly off the list or not. In my opinion, these blood tests on day 3-5 are important to you. I’m glad you are off the birth control pill now because it allows you to get these tests done.
If your biopsy was taken from the area I have noted above, then that’s probably very helpful provided it was analyzed in the lab with horizontal sections. . The key point now is figuring out if there is any possibility of an evolving androgenetic alopecia that just could not be picked up in the early stages with the work up you had. A biopsy with horizontal sections and a good trichoscopic examination by a specialist who understands hair loss will uncover these answers.
Regardless, photos should be taken every 3 months. Not every day and not every week. If there is any kind of evolving pattern of hair loss, a photos will also capture these changes over time.
If TE is truly what you have and there are no underlying concerns, doing minimal additional things could be the best plan. However, if your hyperandrogenism is part of a bigger endocrine issue (like PCOS or CAH), getting advice from an endocrinologist would be a good way to proceed. These blood tests will be a really important guide. Some women just have elevated DHEAS and some women with elevated DHEAS develop AGA but some don’t. I never recommend patients start treatment because of what the labs say - treatment is started because of what the skin or hair is doing.
Thanks again for sending in the question. I hope this helps you are your team of specialists.