Sudden Loss of My Hair: What are possible reasons?
Why am I losing hair?
I’ve selected this question below for this week’s question of the week. It allows us to discuss several important features, including the different diagnosis of red flaky scalps with increased shedding, and the concept of “follicular prominence.”
QUESTION
I am in my early 40s, female and experiencing sudden hair loss that includes scalp & eyebrows (and even eyelashes, but to a lesser extent). I have lost about 25% overall density in the past 2 months. I’m not sure how many hairs I shed each day (too many to count!), but hair is constantly falling out. I usually wake up with a several scalp & eyebrow hairs on my pillow. Prior to then, my hair/scalp was healthy except for a mild episode of telogen effluvium about 10 years ago that resolved within a few months. I do not have any bald spots, the loss appears diffuse. My scalp is moderately itchy/tingly, flaky & slightly tender. I do not have any significant pain or burning. The itchiness & tenderness tend to be worse on the top of the scalp, but overall it is quite itchy.
Right around the same time my hair loss began, I developed small patches of dermatitis/eczema on a few areas of my face, underarms & body. I’m not sure if it’s related, but I’ve never had skin rashes before. I had blood tests (CBC, ferritin, hormones, ANA, ESR & TSH) and all came back within normal ranges (only testosterone at 20 and ferritin at 48 were slightly low).
I am healthy except for early perimenopause symptoms & high cholesterol. I started a new cholesterol medication about a month prior to the hair loss (which I discontinued in the case that was the cause) but the hair shedding has only worsened. My doctor was concerned about Frontal Fibrosing Alopecia due to the eyebrow loss and did two 4 mm punch scalp biopsies. One biopsy was non-diagnostic and the other showed female pattern loss:
I never noticed any hair loss prior to 2 months ago, but I suppose it makes sense to have some female pattern loss given my age. However I was told that probably was not the cause of the rapid shedding. After seeing the biopsy results and doing a scalp exam, the doctor thought the shedding of scalp/eyebrows must be telogen effluvium due to stress/hormones & the itching was seborrheic dermatitis. The only things mentioned during my scalp exam were inflammation and flaking (attached pictures of middle part) and some re-growth in my eyebrow area.
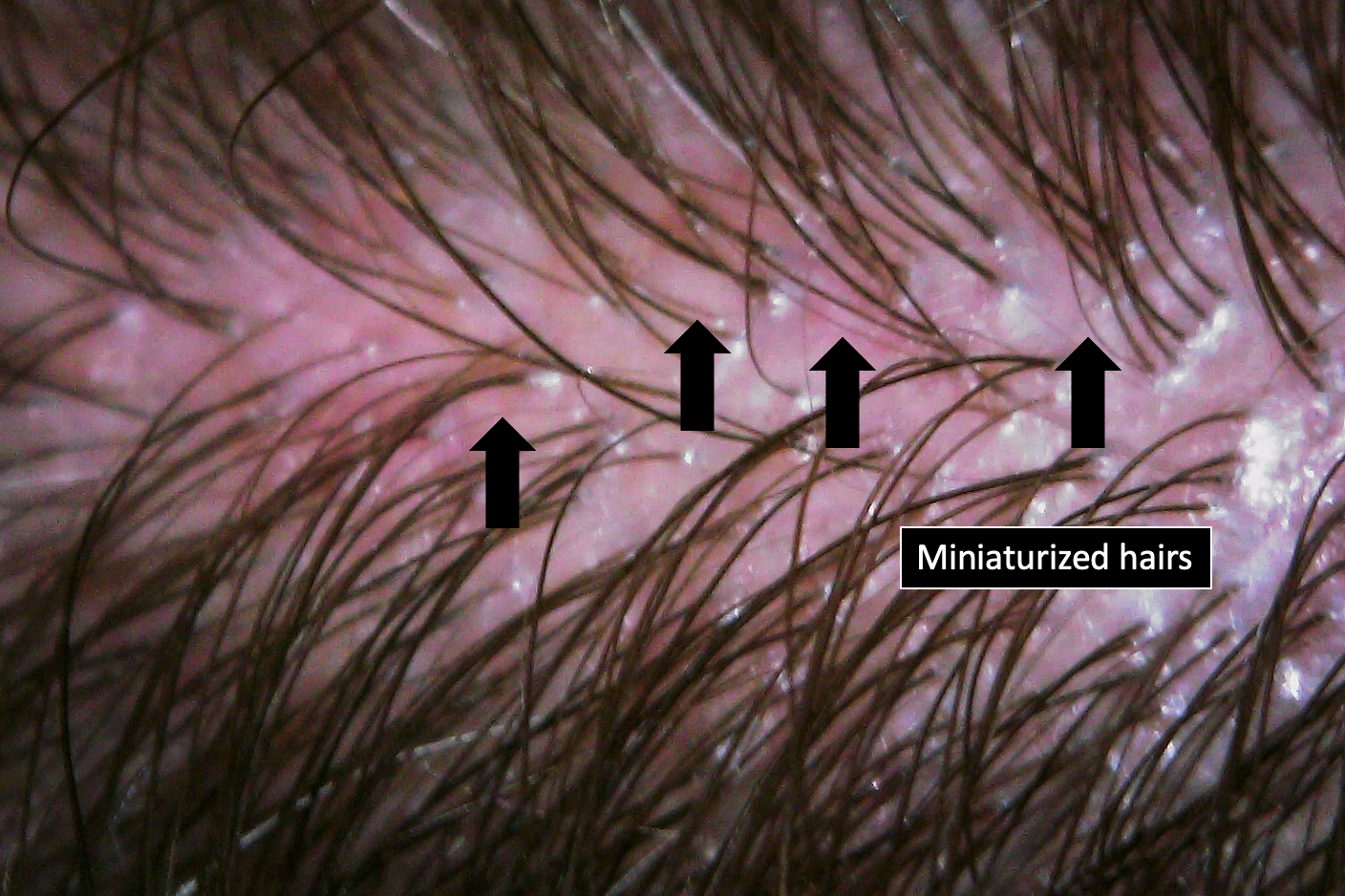
Image 1 of scalp from individual experiencing rapid hair loss.
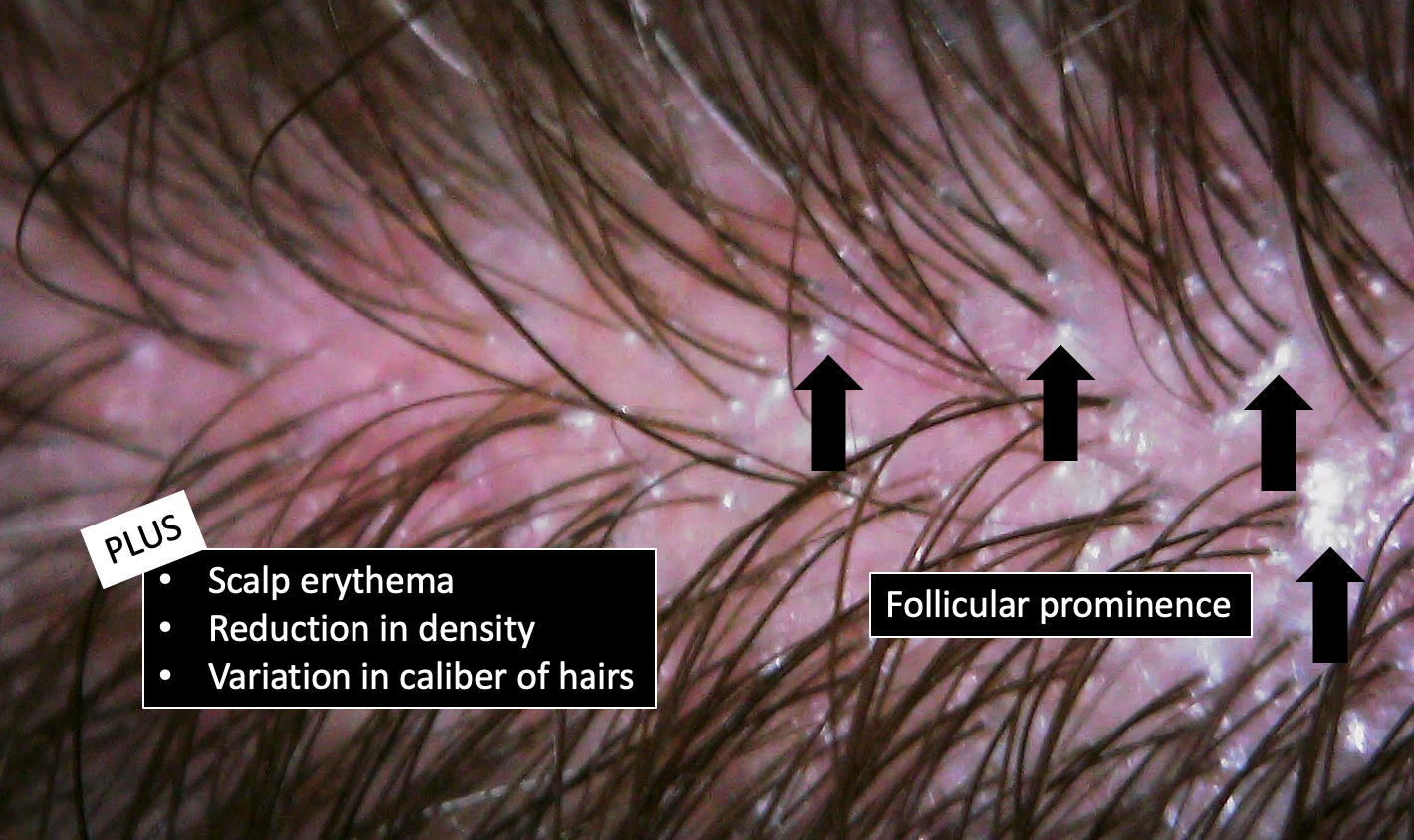
Image 2 from the scalp for individual experiencing hair loss.
My concern is since one biopsy was non-diagnostic, could I have a more serious type of hair loss going on that I should be addressing? Does this sound like a telogen effluvium I should wait out or do you recommend any next steps if a biopsy doesn’t fit with all the symptoms or give a definitive diagnosis? Thank you!
ANSWER
Thanks for the great question. I’d like to discuss several important things in the question you ask and the information you have submitted. Let’s get to it.
Before we do go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s story
2) the findings uncovered during the process of the scalp examination including trichoscopy
3) the results of relevant tests - blood tests and biopsy tests
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
Certainly a more complete story is going to be needed in your case. As I go about reviewing your story, several conditions pop up into the list of possibilities for what’s causing your hair loss. These include one (or MORE) of the following (and likely there are more than one issue):
Androgenetic alopecia
Lichen planopilaris and its variants (fibrosing alopecia pattern distribution & FFA)
Telogen effluvium
Seborrheic dermatitis
Contact dermatitis
Other types of scarring alopecia
I do think with your story that another biopsy is going to be important as I do think lichen planopilaris with androgenetic alopecia together with some degree of seborrheic dermatitis is at the top of the list. Another biopsy (or two) can help clarify this.
Let’s go deeper now into the case that has been submitted.
You present with sudden onset of hair loss and a great deal of shedding. It’s sure sounds like a telogen effluvium at first glance. It’s easy to feel perhaps it’s a TE from the cholesterol drug. The problem with that is that the biopsy does not support that. Second, that’s relatively uncommon. However, biopsies are not really how we nail down a diagnosis of telgoen effluvium so it would be mistake to jump to the conclusion that there is no TE here. However, there is not a great deal of evidence.
You have redness, and itching and tenderness in the scalp and the middles areas are particularly affected. What is the most likely diagnosis in a 42 year old female with new onset itchy, tender, and red scalp especially in middle accompanied by markedly increased shedding? Lichen planopilaris by far. Is it the only possibility? Of course not. But LPP is at the top of the list and we can’t rest until we decide whether it stays on the list of gets removed from the list.
Let’s take a look at some of your “up close” photos a bit more.
1. You have miniaturized hairs.
Your photos show some degree of variation in the caiber of follicles. It’s not much but there is some. I suspect this is being captured to some degree on the biopsy in biopsy “B” where your terminal to vellus ratio was 4.5 to 1. This could suggest some mild female androgenetic alopecia. It’s mild and does not account for the shedding, itching, redness and tenderness you have.
2. Your images illustrate a phenomenon known as “follicular prominence”
Your up close images show what is termed follicular prominence. This is a phenomenon whereby the follicles create little elevations above the surface of the scalp at the point at which they emerge from the scalp.
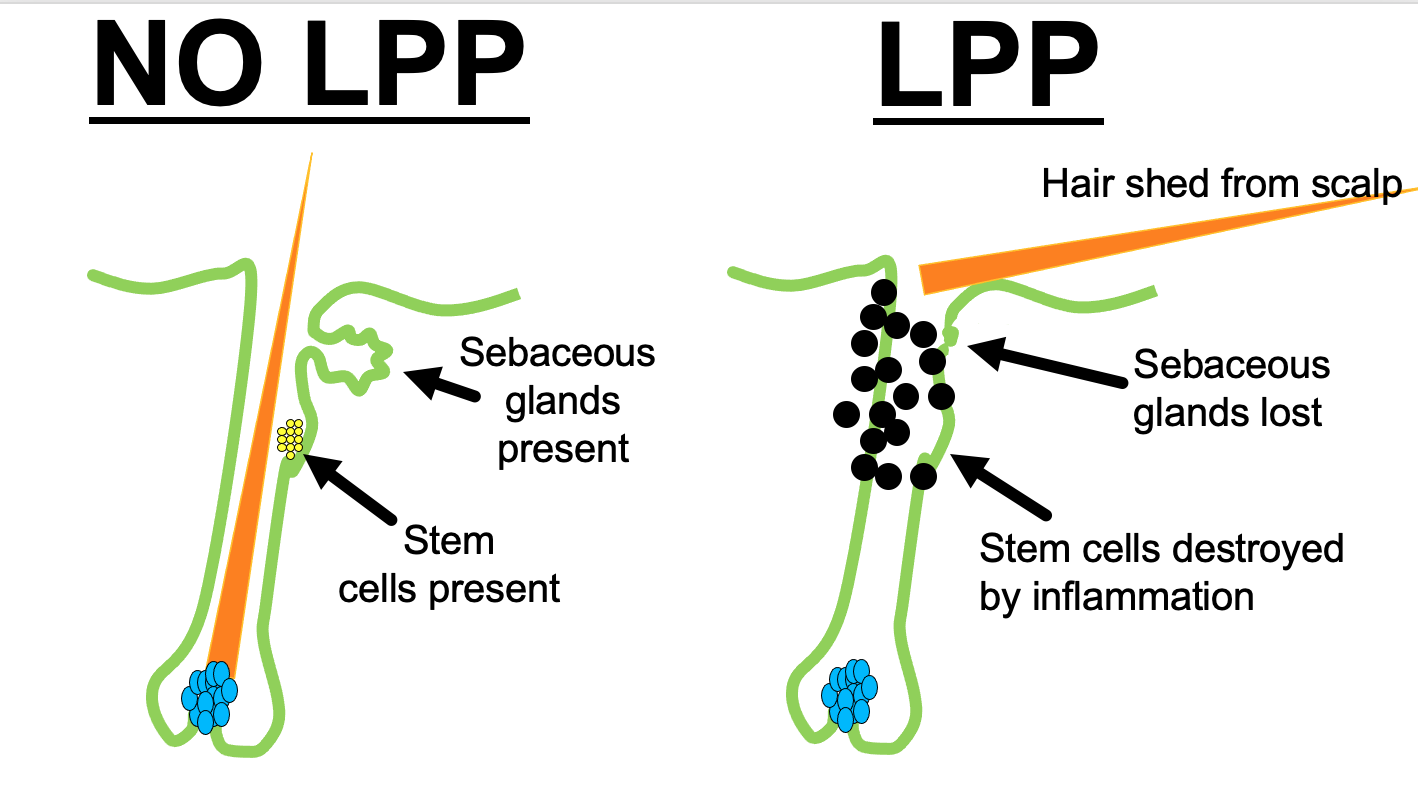
Put into a cartoon-like representation, here is what’s happening:
Now, let me say that follicular prominence is by no means conclusive of a diagnosis of LPP. But what it does mean is that LPP remains at the top of the list in this case until someone definitively proves it’s not LPP. We’ll go into that more in a moment. Follicular prominence is an early finding in LPP and is due to a reactive hyperplasia of the follicular epidermis.
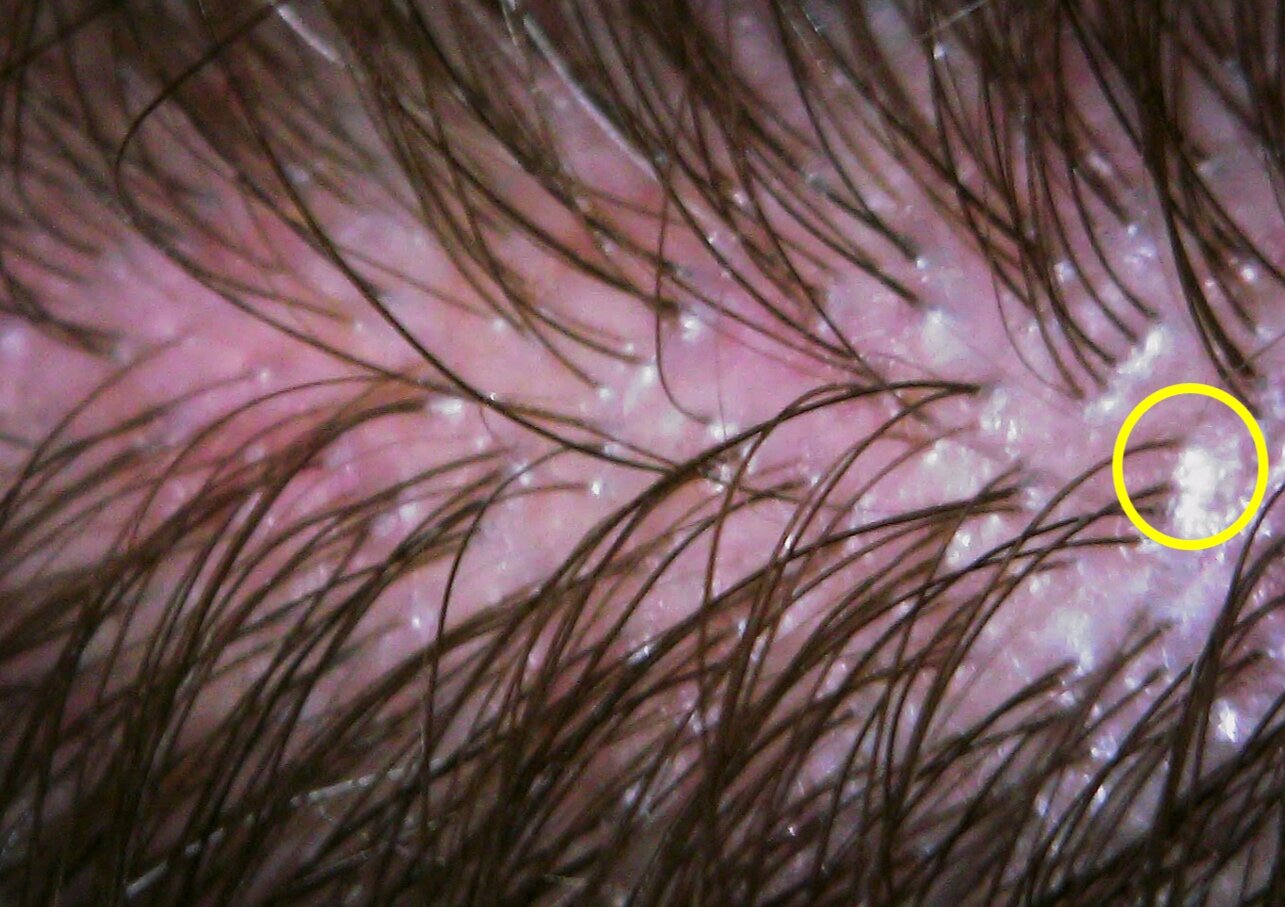
3. Your images show some scaling as well as possible loss of the follicular openings.
As you have pointed out in your submission to the “question of the week” program, you do indeed have scaling - or as you described a somewhat ‘flaky’ scalp. There are many reasons for people to having flaking, but I do note that some of your scale tends to hug the hair follicle quite closely. We call this “perifollcular” scale (a term that simply means scale that occurs around hairs). Perifollicular scaling can be seen in several conditions but certainly LPP is on that list.
Your scalp also shows areas where there is no hair. We call such areas of no hair “atrichia.” These areas of atrichia are shown in yellow in the diagram above. Focal atrichia can be seen in more advanced androgenetic alopecia, but your androgenetic alopecia is certainly not advanced so that can’t really apply. The tiny follicular openings or “pores” can not be clearly seen in these areas in yellow raising the possibility this could be an area of scarring. That’s by no means definite but it needs to be explored further by your doctors.
4. Your images show two types of possible scaling.
There may be two reasons for your scaling or ‘flaking’. The redness and somewhat yellow color and somewhat whitish color scaling calls into question the possibility that there is some degree of seborrheic dermatitis present on the scalp. However, the marked shedding, the follicular prominence and close “perifollicular scale” indicates that seborrheic dermatitis alone as the diagnosis makes little sense. It’s likely a component.
Some of the scale, as shown in the image above, is strikingly tubular - like tubes around the hair. The scale rises up around the hair. This type of scale is unexpected in seborreheic dermatitis alone. It’s again by no means pathognomonic of a scarring alopecia but it’s an important finding.
5. Your images show redness around the hairs.
Redness around the hairs is known as “perifollicular erythema”. It’s quite a non-specific finding but it does remind us that the immune systemic is likely causing some sort of issue in and around the hairs. It’s not a random inflammation anywhere in the scalp - it’s focused on the hairs. We see perifollicular inflammation in many conditions.
6. Your biopsy shows loss of sebaceous glands in biopsy A
Perhaps one of the most important findings in your story is the reduction of sebaceous glands that your pathologist reports in biopsy A. It’s for this reason that LPP is still very much on the list of possibilities.
Loss of sebaceous glands is very much a part of what scarring alopecia is all about. All of the scarring alopecias no matter the cause show loss os sebaceous glands at some point in their evolution. In LPP, reduction in sebaceous glands occurs relatively early in the disease course.
The following cartoon shows what we see under the microscope in LPP. We see loss of sebaceous glands along with inflammation in the upper part of the hair follicle. So what does your biopsy A report ? Loss of sebaceous glands and inflammation in the upper part of the hair follicle (known as the infundibulum).
Does this prove it’s LPP? No, but is is certainly pointing in that direction. Other features we often see in early LPP are not reported in the biopsy report. These include a specific type of inflammation known as “lichenoid inflammation.”
So what’s left to confirm the actual diagnosis ?
I do think in your case another biopsy is going to be helpful. The diagnosis of lichen planopilaris is still at the top fo the list. The discussion around whether this is frontal fibrosing alopecia too depends on whether the frontal hairline is involved. But one thing is for certain - if you do have FFA, you also have LPP because of the involvement of the mid scalp and crown areas.
If you or your doctors are against rebiopsying, you certainly could ask the pathologists to perform a very special stain of your biopsy to look at elastic fibers. This elastin staining technique is very helpful in these challenging cases like you have. It the special test shows your elastic fibers are destroyed, this is likely a true scarring alopecia.
But most likely a repeat biopsy is going to prove really useful.
Where to biopsy?
I do think that if another one (or maybe two) 4 mm biopsies is going to be done, it should be done from an area that shows perifollicular scale, follicular prominence and perifolicular redness. Ideally, this should be from an area of the scalp that is itchy and tender and ideally from somewhere in the middle or crown of the scalp. If the biopsy can be taken from an area that shows all these features that’s even better. The biopsy must contain hairs and ideally if it can include some areas of no hair, that’s great too because that’s where the pathologist will very clearly see the sebaceous glands are lost (if they are indeed lost). Taking from the sides or back is less helpful in my opinion although is often done to ‘hide’ a scar. I don’t recommend this. Some examples of where to biopsy are shown here:
A possible biopsy site: the area on the right shows scale and follicular prominence. This would be preferred over the area on the left side.
A second possible biopsy site: the area shows follicular prominence.
Conclusion
I hope this helps and good luck on the journey to find the precise diagnosis. I do think that one can not rest until LPP is ruled in or ruled out in this particular situation. I certainly favour this diagnosis (along with some androgenetic alopecia and mild seborrheic dermatitis). But it’s not 100% of course.
There are other considerations here too like an allergic contact dermatitis but your biopsy does not show this and the loss of sebaceous glands would not occur in a contact dermatitis. However, this too can be a great mimicker. I don’t really think this is an issue here but one needs to respect this great mimicker, especially when other rashes are present on the body.
Studies have not shown differences in cholesterol profiles between patients with LPP and those who do not have LPP. My own thought is that there is a connection - and I’m always a bit suspicious when young women show up with high cholesterol, itchy red scalps, follicular prominence and shedding. There may be more of a link to the metabolic dysfunction and lipid metabolism issues that we realize. Be sure to follow up on your cholesterol issues.
I do think that repeat biopsies are key here snd that the pathologist should include some elastin stains as well to get a sense of whether the delicate elastic network is destroyed or not. This too can point your doctors in the direction of LPP.
If your testosterone is low, you might consider estradiol, LH and FSH testing to see where in the perimenopasual spectrum you are (if you are at all). Perhaps you’ve already had these tests done. There is a link to earlier menopause in a small proportion of women with some types of scarring alopecia and so these tests should be done as they are quite easy to do. A high FSH and lower estrogen level would be suggestive of this.
If there is any uncertainty that still exists after all these results come back, a trial of topical steroid, steroid injections can be considered in combination with mild allergen free antidandruff type shampoos. If that fails to help other systemic agents can be considered as well.
I wish you the best and thank you for submitting your question.