What's the reason for my hair loss? What does my trichoscopy show?
Why am I experiencing hair loss?
I’ve selected this question below for this week’s question of the week. It allows us to discuss some of the finer aspects of interpreting trichoscopy and how the clinical history must be interpreted together with all trichoscopic analyses.
Here is the question….
QUESTION
I really hope you can help me with the diagnosis of my hair loss that I've been experiencing for a year now without being able to get a real diagnosis, doctors can't seem to find anything else than '' light dermatitis'', yet I can' t help but notice everyday that this isn't normal and I have no clue so far.
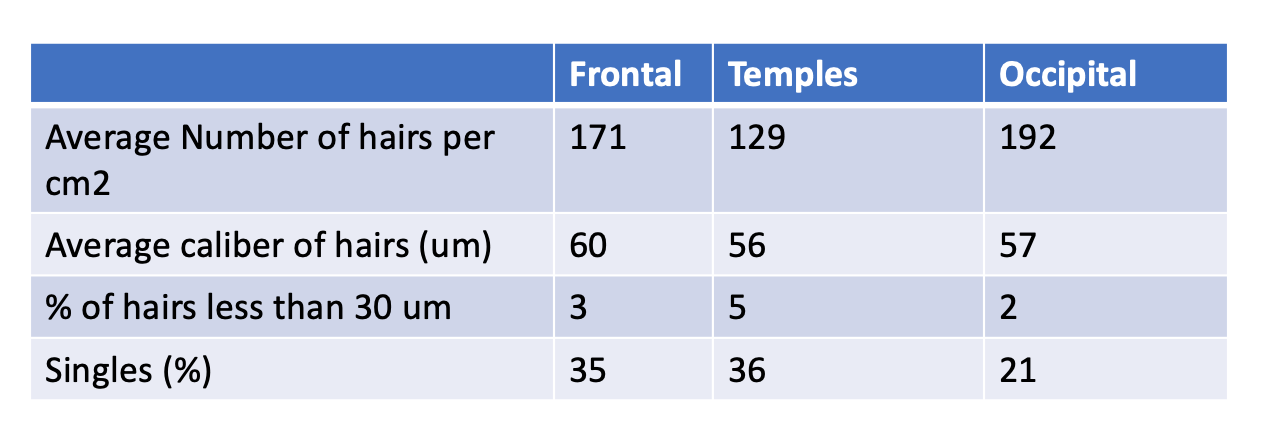
About a year ago I suddenly noticed that I had way less hair and I could see my scalp, which never happened before. A few weeks later I've started to notice redness in my scalp and itching that never left ever since. The itching seems to come and go without any logical pattern, and the more red and itching my scalp gets, the more hair I seem to lose. I did a trichoscopy 2 weeks ago, where you can see the results.
I'm quite desperate to get a real diagnosis because I don't think something innocuous would last that long and cause hair loss without stopping. Overall I am in good health. Blood tests were all okay
ANSWER
This is a great question because it allows us to talk about so many things.
Before we go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s Story
2) the findings uncovered during the process of the scalp examination and
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
I’d like to know a lot more about this story ideally but of course the magic of the “question of the week” is that I tackle questions with limited information.
I can’t be sure of what’s going on entirely without seeing your scalp up close myself and knowing your entire story. Your age, and details about your scalp symptoms all matter.
In my opinion there are 4 possibilities for what you have:
1. Androgenetic alopecia with seborrheic dermatitis (AGA + SD)
2. Androgenetic alopecia with mild telogen effluvium with seborrheic dermatitis (AGA + TE+ SD)
3. Mild telogen effluvium with seborrheic dermatitis (TE + SD)
4. Seborrheic dermatitis alone (SD alone)
I’d like to make a few comments about the type of thinking that is needed in case like this.
A few comments
1. It’s true that you have very nice trichoscopy pictures - but what’s also important is just getting a sense if the frontal density is truly the same as the back. There certainly is a suggestion that your frontal density may be less than the back (occipital area) despite all the numbers that you see in your measurements. If there truly is a significant difference in the density in the frontal and back then we need to think about a patterned hair loss (ie androgenetic alopecia).
2. A physician can get a better sense of density by parting the hair down the middle from front to back and comparing the part width in the front to the back. If the part width is wider in the front than the back that means there may be more hair loss in the front compared to the back - and this might be a suggestion that there is some degree of androgenetic alopecia.
3. It does seem that your blood tests have been normal so we’ll assume that. This does not mean that a person can not have telogen effluvium or androgenetic alopecia with normal blood tests. In fact, most people with hair loss have normal blood tests. I have not seen your blood tests of course, but I would hope that you have had CBC, TSH, ferritin, 25 hydroxyvitamin D. If your periods are irregular you should have a hormonal panel. If you have other symptoms, you might need other testing too.
4. There appears to be clear differences with the photos in the frontal areas compared to the occipital (back) areas including more single hairs and less density. While this could be simply suggesting diffuse loss as in a telogen effluvium, we need to consider the possibility that this could represent a pattern to the loss (and female pattern alopecia also called androgenetic alopecia).
5. Your average hair caliber seems to be lower than expected at 60 um. This depends on your background and your type of hair but it certainly does make me wonder if there is some change happening that affect caliber especially a diffuse process like a diffuse AGA. Of course, androgenetic alopecia is one of the more common hair loss conditions that affect caliber. Your data from the trichoscopy is not definite so I can’t completely rule in or rule out this particular diagnosis.
6. If you do not have much in the way of increased shedding, I would favour a diagnosis of AGA. If there is a lot of shedding that you have, it still could be AGA but a mild effluvium (TE) certainly does not need to be considered. Your story of suddenly “noticing” that you have less hair is more typical of AGA than TE. The degree that you are shedding today and the degree that you have been shedding in the past 6-9 months would sway me someone as far as how likely a diagnosis of TE really is.
7. I do favour options 1 and 2 but it’s by no means definite based on the information you have given. It will be helpful to follow the trichsocopy measurements over time. If you have a TE like in option 3, the measurements and numbers will likely get better over time. If it’s an AGA (option 1 and 2), the numbers will not likely improve and may get slightly worse in 6-12 months. Photos will also be very helpful. If it does become clear that the density in the frontal areas is slightly less than the back of the scalp, one needs to consider androgenetic alopecia.
8. If you are concerned a scalp biopsy or a 5 day modified hair wash test might help. Sometimes in the very early stages a a biopsy only slightly helpful so I am not of the opinion that you must have a biopsy. However, if the terminal to vellus ratio of your biopsy is shown to be less than 4:1 it indicates androgenetic alopecia is likely to be present. If the terminal to vellus ratio is above 4:1 is suggests that TE alone (option 3 or 4) is more likely. A biopsy can also capture any rare mimickers of redness such as lichen planopilaris, although I do not suspect that is what is going on (the density and changes are far too similar in the 3 areas to really support early LPP - and the story I have so far and the trichoscopy does not really support that diagnosis). A modified hair wash test can give a sense of how many hairs are being shed and whether any of these are small. What’s interesting in your photos is that it does appear that there are more vellus hairs in the photos from the frontal area than the measurements state in the information you were given. I am personally a big believer not only in looking at the measurements these computers give but also in looking at the images myself and looking at the scalp myself and getting sense if the measurements the computer gives makes sense or not. The presence of thinner and thinner hairs (miniaturized hairs) and the presence of thinner and shorter hairs (vellus hairs) is what androgenetic alopecia is all about.
9. I do think that there is likely a component of seborrheic dermatitis complicating the picture here. Your dermatologist can review with you at your next appointment. The trichoscopy would suggest this as well. SD is not typically a major cause of hair loss but can give a bit of shedding if severe enough. If you do have SD, it is mild and may contribute to symptoms like itching and tingling from time to time and then there will be periods where the scalp feels good again. The involvement of the temples is quite typical of SD and your photos are noticeably most red in the temples. There are no signs of scarring alopecia in the trichoscopy images provided but again a biopsy can help further clarify.
FINAL SUMMARY
Thanks for the great question. With the information provided, I can’t say one way or another exactly what is the diagnosis. However, a scalp biopsy or 5 day modified hair wash test could take you that much closer to understanding the diagnosis if there is really debate. I am suspicious about their being androgenetic alopecia here but I can’t tell for sure and ideally would want to see the scalp in a situation like this. Once you have the proper diagnosis, you can plan treatment. In addition, it is going to become much clearer over time what the diagnosis is especially if you do repeat trichoscopy measurements in 6 and 12 months. The frontal density and caliber of the hair in the frontal area will decrease and the number of single hairs is going to increase in the frontal if AGA is truly what is present. For now, treating the seborrheic dermatitis is quite reasonable. I would normally recommend that efforts be put into confirming the diagnosis with certainty. Some of the treatments for TE overlap with AGA treatments including laser and topical minoxidil and oral minoxidil so one can certainly get started with a plan once the diagnosis is made. Certain other treatments however, like anti androgens, are only effective in AGA and will not be effective if TE is the true diagnosis.
Thank you for your question.