Management of Lichen Planopilaris in Pregnancy.
How Might One Treat Lichen Planopilaris in Pregnancy?
I have discussed several important general points about the management of scarring alopecia in pregnancy in prior articles.
There are several key points to remember when treating scarring alopecia during pregnancy.
Often the activity of a scarring alopecia decreases rather than increases in pregnancy. While we certainly need to be prepared to help the patient treat her LPP more aggressively we need to be ready for the very high likelihood that the LPP activity will actually reduce through the pregnancy. In my experience, many patients have reduced LPP activity rather than increased LPP activity during pregnancy.
There must be a continued open dialogue between the dermatologist and the patient and the physician overseeing care of the mother and baby. That may be a primary care physician or obstetrician/gynecologist. Decisions are made together - this is truly shared decision making.
The lowest doses of medication is what one must strive for at all times. If a medication is not needed, then it shouldn’t be used at all. If a lower dose can be used instead, then it should be used rather than the higher dose. If one medication can do just as good of a job as two medications, then the better choice is to use one medication only. If a medication can be just as helpful once per week than twice per week, then once per week is the correct dose.
Treatments with years and years of having a good track record in pregnant patients should be used over new treatments with little evidence.
Ongoing dialogue with the primary care physician or ob/gynecologist, especially as treatment changes
If hair is not being lost, one might accept a slightly higher amount of scalp redness than they might otherwise if the patient was not pregnant. The key overall is to make sure that hairs are not being lost in a permanent manner.
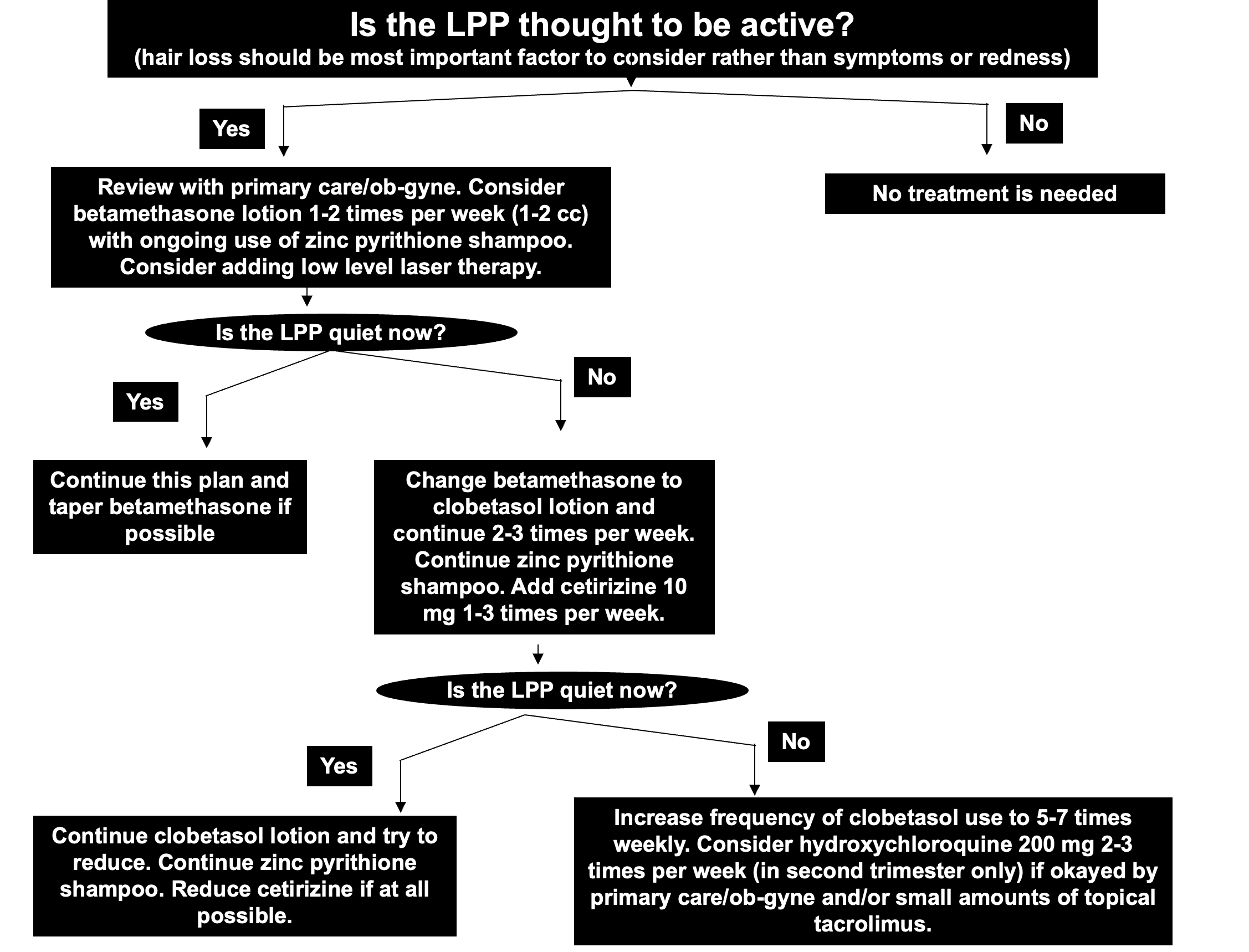
Typical Treatment Algorithm for Management of LPP in Pregnancy
The following diagram shows one possible algorithm that I recommend. Generally speaking if the LPP is active, I start with betamethasone lotion a few times per week. Betamethasone is quite safe. Zinc pyrithione is used occasionally as a shampoo to ensure that seborrheic dermatitis is not making the LPP look worse than it might be. Given the safety of low level laser and potential benefits in LPP, I often recommend patient’s add a low level laser device to the plan at this point. . In 2017, Fonda-Pascual and colleagues from Spain showed clear benefits for the use of LLLT in patients with lichen planopilaris. All patients had a reduction in symptoms, redness and scaling and there was a decrease in the disease activity after 6 months. If the betamethasone does not seem to be helping, I often move on to prescribing clobetasol lotion rather than betamethasone. Cetirizine (Reactine, Zrytec) can be added at 10 mg 1-3 times per week provided the ob-gyne or primary care doctor is okay with this. If this is still not seeming to be effective, I will increase clobetasol use to daily. I will then have a discussion with the patient and her physician teams about the possibility of adding low doses of hydroxychloroquine in the near future. I only recommend hydroxychloroquine if needed and only in the second and third trimester given the small increased risk of congenital malformations that have been noted with first trimester hydroxychloroquine use. Cyclosporine is generally not needed but would be something to consider in the event of a rapidly progressive case.
I am not a fan of steroid injections in pregnancy. If we need to deliver more anti-inflammatory corticosteroid to the hair follicle, I prefer we do it by increasing the amount of clobetasol used and the frequency that it is used. Steroid absorption into the body is higher with steroid injections in my experience and more difficult to precisely titrate during pregnancy. It is a good option after delivery.
Topical steroids give us an ability to rapidly change the plan within a day or two. Steroid injections don’t allow us to change the plan for a month or two. During pregnancy, we need the flexibility to change course at an instant for optimal management.
I do not use PRP during pregnancy. Options such as doxycycline, tetracycline, minocycline, methotrexate, mycophenolate mofetil, apremilast, isotretinoin, minoxidil, antiandrogens, JAK inhibitors, azathioprine, TNF inhibitors are not permitted in pregnancy. These are all strongly contraindicated.
REFERENCES
Christopher V et al. Pregnancy outcome after liver transplantation: a single-center experience of 71 pregnancies in 45 recipients. Liver Transpl 2006;12(7):1138-43.
Clowse M et al. Pregnancy Outcomes in the Tofacitinib Safety Databases for Rheumatoid Arthritis and Psoriasis Drug Saf. 2016; 39: 755–762.
Costedoat-Chalumeau et al. Safety of hydroxychloroquine in pregnant patients with connective tissue diseases: a study of one hundred thirty-three cases compared with a control group. Arthritis Rheum 2003 Nov;48(11):3207-11.
Curtin SC, et al. Pregnancy rates for U.S. women continue to drop. NCHS data brief, no 136. National Center for Health Statistics. 2013.
Götestam Skorpen C et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis 2016;75:795–810.
Huybrechts KF et al. Hydroxychloroquine early in pregnancy and risk of birth defects. Am J Ob Gynecol. 2020 Sep 19;S0002-9378(20)31064-4.
Jabiry-Zieniewicz Z et al. Outcome of four high-risk pregnancies in female liver transplant recipients on tacrolimus immunosuppression. Transplant Proc 2006;38(1):255-7.
Jain A et al. Pregnancy after liver transplantation under tacrolimus. Transplantation 1997;64(4):559-65.
Kainz A et al. Review of the course and outcome of 100 pregnancies in 84 women treated with tacrolimus. Transplantation2000;70(12):1718-21.
Jain AB et al. Pregnancy after liver transplantation with tacrolimus immunosuppression: a single center’s experience update at 13 years. Transplantation 2003;76(5):827-32.
Jain AB et al. Pregnancy after kidney and kidney-pancreas transplantation under tacrolimus: a single center’s experience. Transplantation 2004;77(6):897-902.
Johansen CB et al. The Use and Safety of TNF Inhibitors during Pregnancy in Women with Psoriasis: A Review. Int J Mol Sci. 2018 May; 19(5): 1349.
Mitchell AA et al.; National Birth Defects Prevention Study. Medication use during pregnancy, with particular focus on prescription drugs: 1976–2008. Am J Obstet Gynecol2011;205:51.e1–8.
Nevers W et al. Safety of tacrolimus in pregnancy. Canadian Family Physician October 2014, 60 (10) 905-906;
Vellanki K et al. Pregnancy in chronic kidney disease Adv Chronic Kidney Dis. 2013 May;20(3):223-8.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.