On the Use of Scalp Magnification by the Public and Untrained
Warnings on the Use of Scalp Magnification
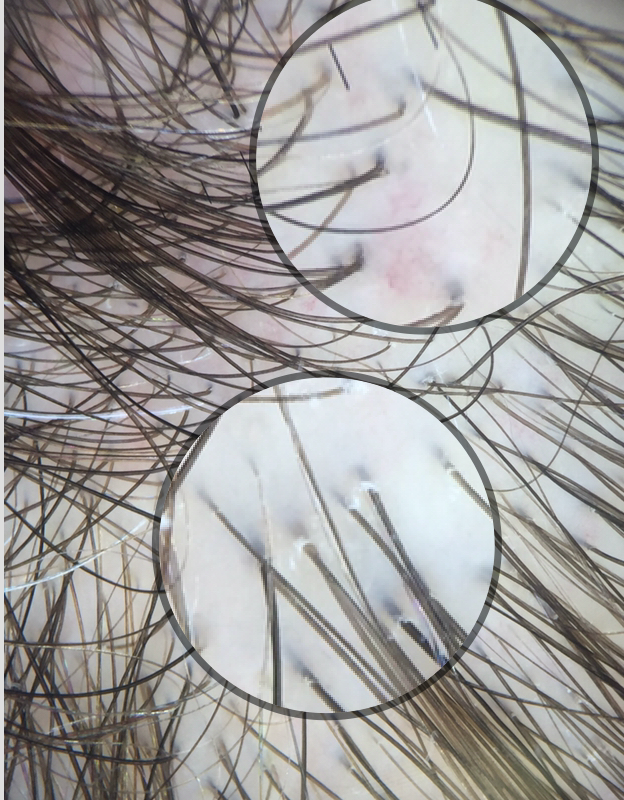
Magnified Scalp Examination
Looking at the scalp up close is interesting and fascinating. Nowadays, for relatively inexpensive prices (under $50 USD), anyone can purchase a handheld microscope to look at the scalp up close. Some clinics have fancier devices.
For simplicity, I’m just going to refer to the various forms of scalp examination using some type of magnified lens as Magnified Scalp Examination (MSE). For those who wish to be precise, there is some difference between a magnifying glass, a magnified device and a polarizing dermatoscope. But for the sake of discussion, I will refer to all as MSE.
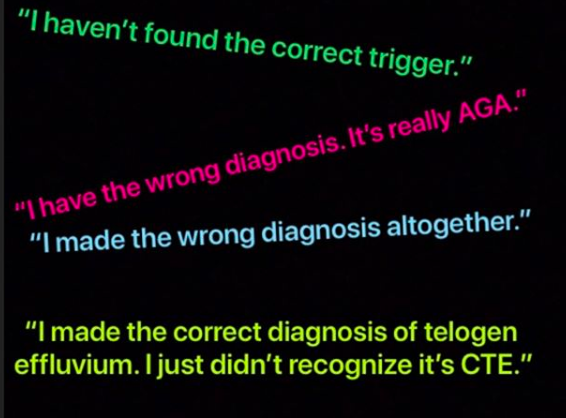
The Misuse of MSE by Professionals
Let me be the first to say that MSE is frequently misused both knowingly and unknowingly. It’s a topic not talked about often, (and in fact I’m really not sure it’s ever been talked about). There are certainly a proportion of salons, clinics, offices, establishments that use MSE with a client in a somewhat deceptive manner. Generally the client or patient is examined with the MSE device and told and even shown that follicles that are “plugged” or follicles that are “dying.” The purpose of course of giving this assessment is often to encourage clients to do something on an urgent or semi-urgent basis to “unplug” hairs or prevent more hairs from “dying.” Frankly, it usually means encouraging the patient to buy something that the establishment offers for sale. Sadly, all too often what is seen is not really a plugged follicle and the concept of hair death is exaggerated.
Worse yet, many clinics not only sell patients a variety of treatments but then use MSE at various follow up appointments to convince a patient that they see “new hairs sprouting” and may even use a MSE device to show the patient or client the new hairs. (In case readers did not know, the human scalp is ALWAYS full of some new hair growth and one can always find a new hair or two).
Training in MSE
I’m not against professionals using various forms of MSE, but sadly many have very limited training and really have limited understanding of the hundreds and hundreds of patterns and findings that can be seen. I’m sorry to say that MSE frequently becomes simply a marketing tool.
But I would like to add that patients like it when their professionals use MSE. Patients even expect it and in many cases state how pleased they are that “someone took the time to really look up close.” The quality of the advice is often overlooked. But the entire show is too often deceiving and the script is too often the same. (“look at your plugged pores and dying hairs”).
MSE is appropriate of course in many situations and when used appropriately can be a great teaching tool for patients. Patients with genetic hair loss looking at a camera image can appreciate that their follicles are getting thinner and thinner. They may be redness and inflammation. When two areas of the scalp are compared 'before' and 'after' it can become very clear that an improvement or worsening has occurred. This is how MSE is best used.
The Misuse of MSE by the Public
There is a huge increase in the number of people in the general public buying various forms of MSE equipment on the internet and using it in their homes home for the purpose of self-diagnosis. There’s nothing wrong with this provided it is only used for general interest. Using MSE for self diagnosis has its problems.
See previous article: The Self Diagnosis of Hair Loss: A DIY Project to Avoid.
Too often, patients who buy MSE devices for personal use use these devices in a manner that only increases their anxiety and confusion. There is nothing wrong with being inquisitive and taking charge of one’s own health. However, when it comes at the expense of one’s emotional health, it’s dangerous.
Ten years ago, I don’t think there was even one patient who ever emailed or brought in photos of the scalp they obtained with MSE. Now it happens at least weekly. Patients see things “up close” with their MSE devices and convince themselves they have a particular condition when they do not.
The examples are numerous. The patient who sees a single skinny hair on the scalp and convinces herself she has female balding (when in fact it’s a normal finding). Or how about the patient who sees scale around a hair and convinces himself he has scarring alopecia (when in fact the finding represents simple dandruff). Consider too the patient who sees a strange hair and convinces herself she has alopecia areata (when in fact the hair has no significance in this case). Today I received further emails from patients who had performed MSE at home only to encounter confusion.
It’s okay to be curious. But what often happens in these cases is that the patient’s emotional health is jeopardized by their use of MSE. One can not underestimate the stress that patients feel when they think they have a particular condition.
Conclusion
MSE is wonderful. Let me be the first to say that without my dermatoscope, I would not be able to practice hair dermatology in the same way. Patients also love MSE - which makes them vulnerable to its misuse.
If one attends clinics, salons, offices that use various MSE devices, that is wonderful. But one needs to be weary of any clinic offering extensive advice based on the findings of MSE, especially when using terminology that involves discussion about 'plugged follicles' and 'dying' hairs. Such terms are too often meant to scare and confuse. When discussion is focused on hair density changes, inflammation, miniaturization, hair follicle calibre measurements (in micrometers), the likelihood that a valid assessment is being performed goes up considerably. Of course, it's still no guarantee and all patients must be aware of the basics of the "buyer beware" concepts.
To use a MSE without appropriate training is unprofessional. To use an MSE device to deceive is unethical and possibly even illegal in some jurisdictions. More work is needed by professional organizations worldwide to establish ethical guidelines for the public in multiple areas of evaluating and treating hair loss.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.