Platelet rich plasma (PRP) for LPP: Is it an option?
Does PRP help lichen planopilaris and other scarring alopecias? Maybe sometimes.. Does it help the disease alot? Rarely. Is is a good option for starting treatment for someone with LPP? No, it’s not.
That’s the jist of what really needs to be said and that’s where this article could end. But I won’t let it end there. In the present day, PRP is popular. If people are looking for a popular treatment, I say go for it. it If they are looking for a treatment that helps stop a disease and is effective, I’d say have seat and let’s chat. Popular vs effective - the choice is up to the patient.
To say that PRP is a consistently effective treatment for scarring alopecia is nonsense. In fact, even with the most potent of drugs we don’t always shut down this disease. Of course, we win a good amount of the time in treating scarring alopecia but not nearly enough.
PRP is popular nowadays because it is fairly safe (there are side effects of course that one needs to know about). Yes, it’s that patient’s own blood. Yes, it’s not a drug. Yes, it’s natural. I agree with all these points. Do I agree that it stops scarring alopecia on a consistent basis? No way. How do I know? I treat a lot of patients with scarring alopecia over the years and I have treated lot of patients with PRP over the years. But more importantly I have treated a good number of patients with scarring alopecia PLUS PRP over the years and never found it to really help that much.
The most effective treatments for lichen planopilaris are treatments that are found in the following list: hydroxychloroquine (Plaquenil), doxycycline, methotrexate, cyclosporine, topical steroids, steroid injections, tacrolimus, mycophonolate, isotretinoin, tofacitinib. Treatments like low level laser may also help a bit.
The most effective treatments for frontal fibrosing alopecia are treatments that are found in the following list: antiandrogens, isotretinoin hydroxychloroquine (Plaquenil), doxycycline, methotrexate, cyclosporine, topical steroids, steroid injections, tacrolimus, mycophonolate.
Conclusion.
When a patients says to me - “I want PRP for treating my disease” I say to them the following:
IF PRP treatment is something you want for treating your LPP, I will leave the ultimate decision to you. If you can answer the following 3 simple questions for me, you may in fact be a good candidate for considering PRP. If you answer no to any of the following, I would urge you to please rethink the plan:
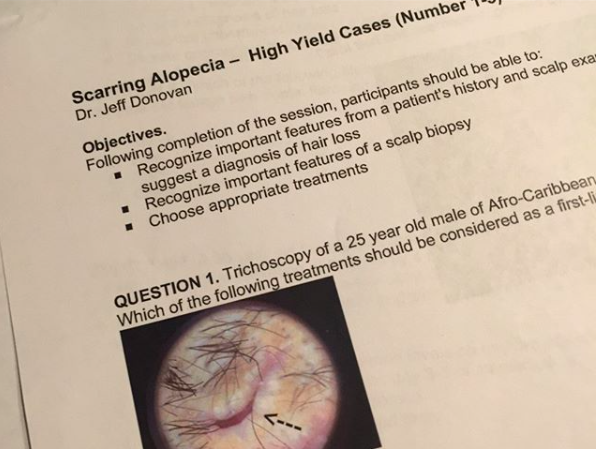
QUESTION 1: Can you say out loud at least 5 types of medications that are typically used to treat your type of scarring alopecia? Yes or No.
QUESTION 2: Do you take photos of your scalp (or does somebody take photos) consistently every 3-6 months? Yes or No.
QUESTION 3: Do you understand that PRP may be required every few months for life and that it is not a one time treatment? Yes or No.
If a patient answers yes to ALL of these three questions, there is a good chance they have the background understanding that puts them in a position to make an informed decision about PRP for treating their scarring alopecia. Of course, I’d also like the patient to be able to state in question 1 how well the treatment is expected to work (i.e. percent of patients they are expeccted to help) but these 3 questions are pretty good screening questions.
IF a patient can not answer ‘yes’ to these three questions or answers no to even one of them, I would say to the patient - perhaps rethink the plan (PRP).