Donovan Hair Academy Announces Picks for the Top 20 Hair Research Studies of 2023
In keeping with the annual year-end tradition, Dr Donovan announces choices for the top 20 hair research studies of the past year. This year’s public webinar will take place Dec 13 at 5 pm PST (8 pm EST). The 20 studies will be discussed at the webinar.
Registration is required for the webinar and this can be done using the links below:
REGISTER FOR THE TOP 20 HAIR RESEARCH STUDIES of 2023
A recording of the webinar will be made available at a later date on the DonovanMedical youtube channel and broadcast to the Evidence Based Hair Podcast as well.
DERMATOPATHOLOGY
Douglas A et al. Scalp Biopsy Influences Diagnostic Accuracy and Treatment in Black Women with Alopecia: A Retrospective Study. J Am Acad Dermatol. 2023 Jan 31;S0190-9622(23)00157-3.
ANDROGENETIC ALOPECIA
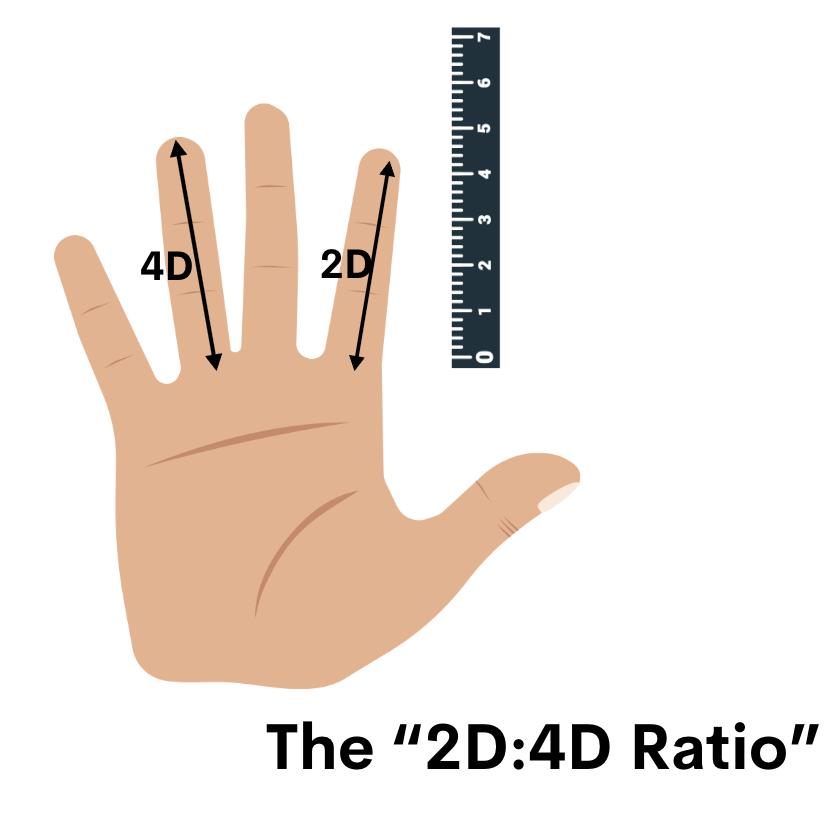
Gupta AK et al. The relative efficacy of monotherapy with 5-alpha reductase inhibitors and minoxidil for female pattern hair loss: A network meta-analysis study. J Cosmet Dermatol. 2023 Jun 29
Jimenez-Cauhe J et al. Safety of Low-Dose Oral Minoxidil in Patients With Hypertension and Arrhythmia: A Multicenter Study of 264 Patients. Actas Dermosifiliogr. 2023 Aug 29:S0001-7310(23)00679-8.
ALOPECIA AREATA
Gandhi et al. The Association of Alopecia Areata-Related Emotional Symptoms with Work Productivity and Daily Activity Among Patients with Alopecia Areata. Dermatol Ther (Heidelb). 2023 Jan;13(1):285-298.
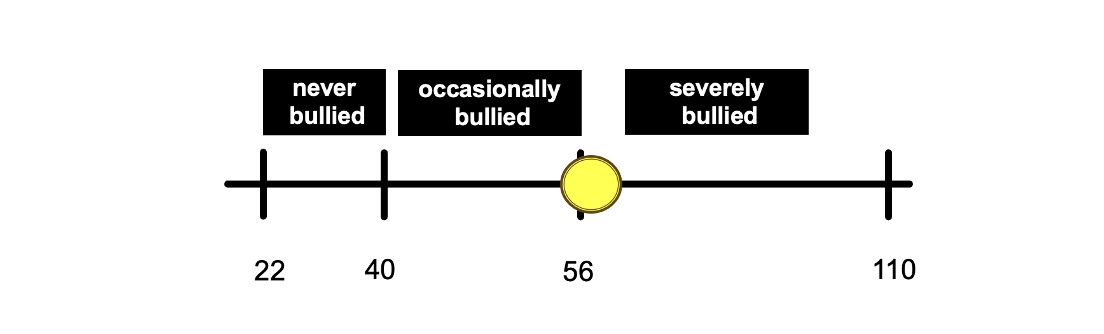
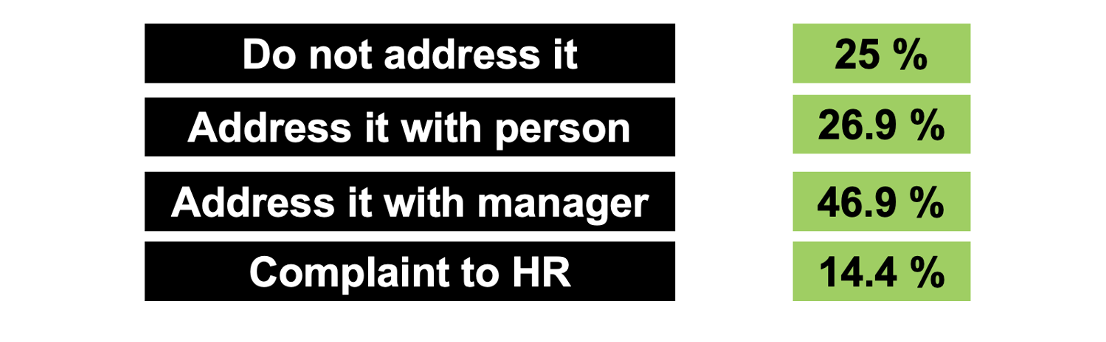
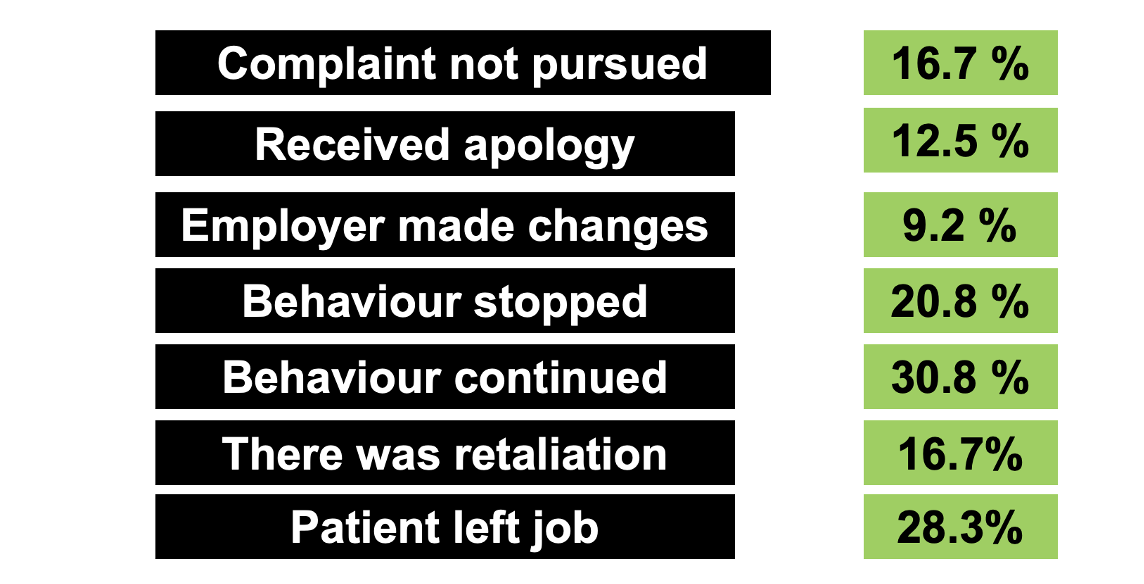
Li SJ et al. Experiencing Workplace Bullying in Patients with Alopecia Areata: A Cross-Sectional Survey Study. Skin Appendage Disord. 2023 Aug;9(4):258-261
Kazmi A et al. Switching between tofacitinib and baricitinib in alopecia areata: A review of clinical response. J Am Acad Dermatol. 2023 Apr 4;S0190-9622(23)00532-7.
King B et al. Efficacy and safety of ritlecitinib in adults and adolescents with alopecia areata: a randomised, double-blind, multicentre, phase 2b-3 trial. Lancet. 2023 May 6;401(10387):1518-1529.
George P et al. Incidence Rates of Infections, Malignancies, Thromboembolism, and Cardiovascular Events in an Alopecia Areata Cohort from a US Claims Database., Dermatol Ther (Heidelb). 2023 Aug; 13(8): 1733–1746.
Wang C-W et al. Clinical characteristics and immune profiles of patients with immune-mediated alopecia associated with COVID-19 vaccinations. Clin Immunol. 2023 Oct:255:109737.
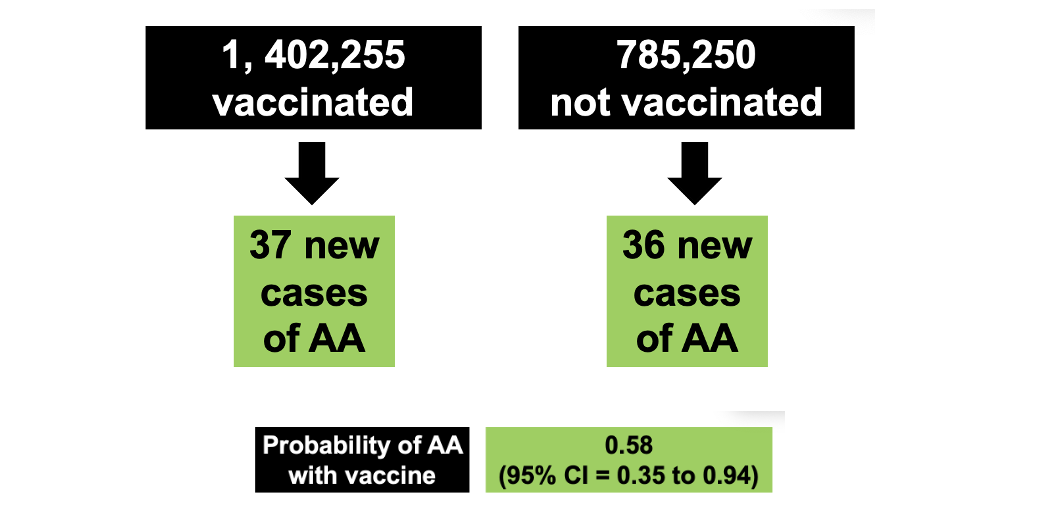
Chen J et al. The Incidence of Alopecia Areata in a COVID-19- Vaccinated Population: A Single-Center Review. Cureus 2023
TELOGEN EFFLUVIUM
Michelini S et al. Telogen Effluvium in SARS-CoV-2 Infection: histological aspects. J Eur Acad Dermatol Venereol. 2023 Mar 8.
TINEA CAPITIS
Gold, JA et al. Inadequate diagnostic testing and systemic antifungal prescribing for tinea capitis in an observational cohort study of 3.9 million children, United States. J Am Acad Dermatol. 2023 Feb 15;S0190-9622(23)00189-5.
COSMETIC DERMATOLOGY
Landau M et al. Nonscarring alopecia after temporal lifting technique with dermal fillers. JAAD Case Rep. 2023 May 12;37:30-34
GENERAL SCARRING ALOPECIA
Kim SR et al. Association of Primary Cicatricial Alopecia with Subsequent Cardiovascular Disease. J Invest Dermatol. 2023 Nov 19:S
LICHEN PLANOPILARIS
Lim SH et al. Prevalence and Incidence of Comorbid Diseases and Mortality Risk Associated with Lichen Planopilaris: A Korean Nationwide Population-Based Study. Clin Exp Dermatol. 2023 Jul 11;llad235
FOLLICULITIS DECALVANS
Matard B et al. Folliculitis decalvans and dystrophic epidermolysis bullosa: a significant association. Br J Dermatol 2022 Dec;187(6):1026-1028.
DISCOID LUPUS
Fredeau L et al. Risk factors of progression from discoid lupus to severe systemic lupus erythematosus: a registry-based cohort study of 164 patients. J Am Acad Dermatol. 2023 Mar;88(3):551-559.
DISSECTING CELLULITIS
Cajas-Garcia MS et al. Distinct presentations of scalp dissecting cellulitis manifesting with furrows and gyri. J Eur Acad Dermatol Venereol. 2023 Feb 3.
CENTRAL CENTRIFUGAL CICATRICIAL ALOPECIA
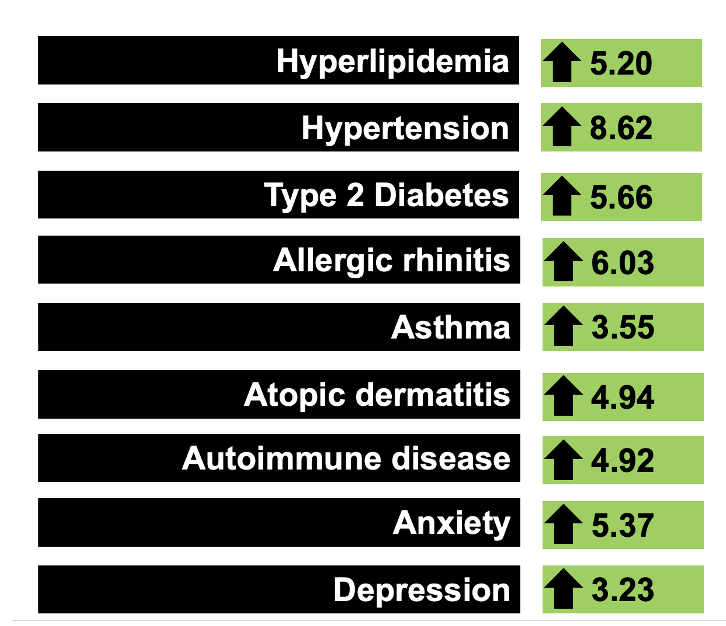
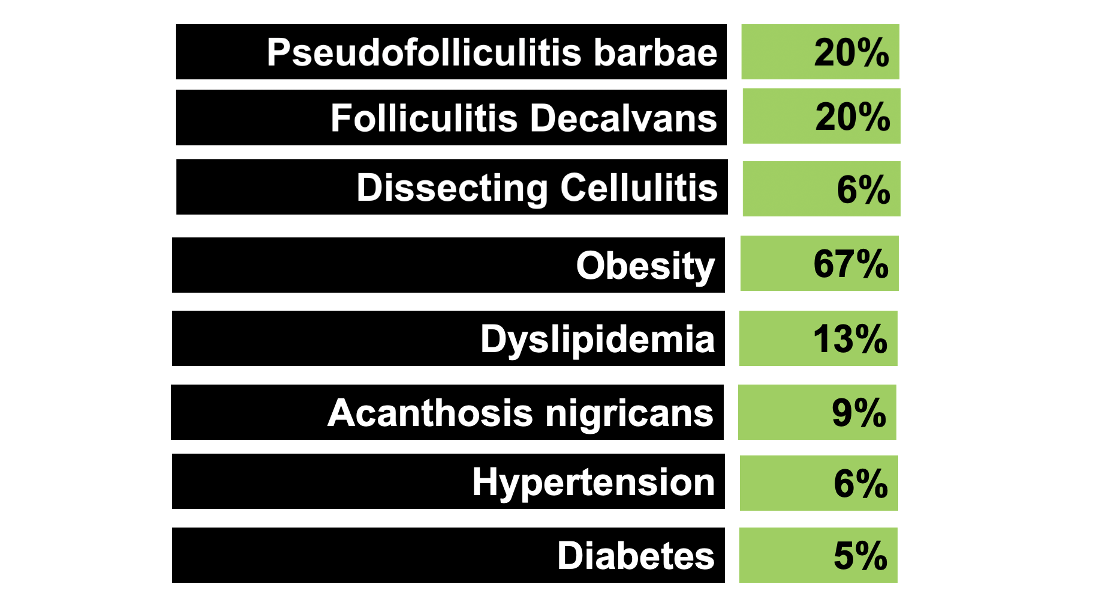
Joshi TP et al. Comorbidities in patients with central centrifugal cicatricial alopecia: a case-control study. Int J Dermatol. 2023 Nov 23.
ACNE KELOIDALIS NUCHAE
Lobato-Berezo A et al. Acne keloidalis nuchae: An international multicentric review of 79 patients. J Eur Acad Dermatol Venereol. 2023 Nov 1.