Chronic shedding after Stopping Oral Minxoidil
Alopecia Areata Incognita, Androgenetic Alopecia and Chronic Shedding
I’ve selected this question below for this week’s question of the week. It allows us to review some concepts in the the diagnosis and treatment of chronic shedding in the context of androgenetic alopecia.
QUESTION
Good evening Dr. Donovan, I am in my late 30s, female, and have been suffering from androgenetic alopecia since 2009.
Since 2014, following a biopsy, I have also been diagnosed with alopecia areata incognita. I would like to ask you about a question that my dermatologists have not been able to explain to me.
I was treated the first few years with 2% minoxidil and later 5%. Over the years also courses of cortisone, oral, local and intramuscular, in order to control the alopecia areata.
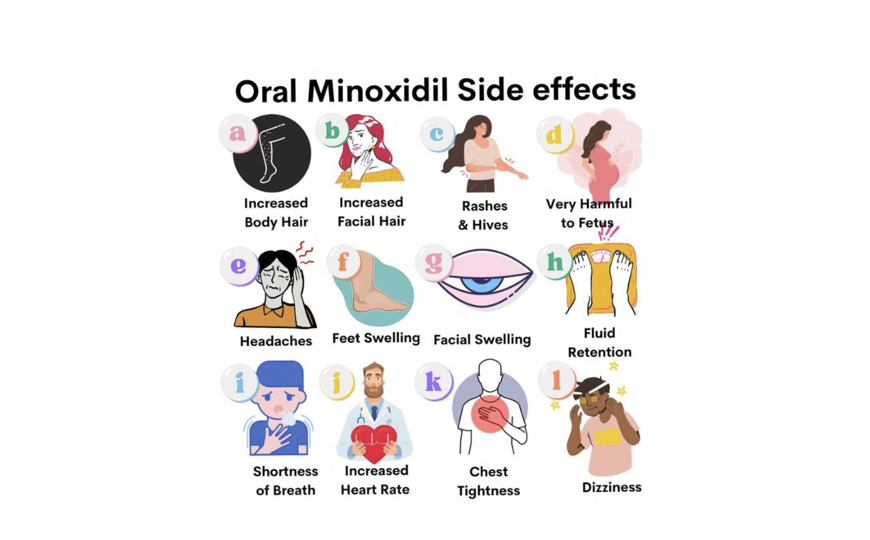
In 2019, in addition to the topical minoxidil that I’ve never stopped, I was prescribed oral minoxidil, gradually increasing to 2.5 mg. After 6-7 months I had severe insomnia and had to stop it.
In the years that followed, until last October, I made other attempts with oral minoxidil both by lowering the dose and by changing different pharmacies (in Italy it's only galenic). I always had to stop after a few months, I experienced several side effects (tingling in the limbs, tachycardia).
I never had problems with the topical version, but the oral one is not for me.
Since I was diagnosed with alopecia I have always had a strong hair fall, but during the 6 months of oral minoxidil the fall had disappeared almost completely! I was happy!
Already in the last few weeks I began to notice the loss of several short and fine hairs, which got enormously worse after the abrupt interruption due to insomnia. I have been losing 100/200 hairs every day and 300/400 when I wash them for more than 3 years.
70% of the hair that falls out nowadays is less than 2 cm or vellus.
I still have strong regrowth but they fall off quickly.
As you can imagine, in 3 years the volume of my hair has halved, especially at the top. At the moment I use topical minoxidil 5% and also finasteride 2.5 mg since 2022.
I'm afraid attempts at oral minoxidil have permanently messed up my hair cycle. Is it possible? Could it have triggered a chronic telogen effluvium? It will never have an end? Thanks for your attention and thanks if you want to answer me.
ANSWER
Thanks for the question. This is a challenging question. Thanks for describing things so carefully – you really understand these issues very well and I can tell you’ve given a lot of thought to all this!
It could be that there are three potential issues here:
a) the androgenetic alopecia has accelerated after the oral minoxidil was stopped
b) the alopecia areata incognita is active
c) there is a telogen effluvium present here.
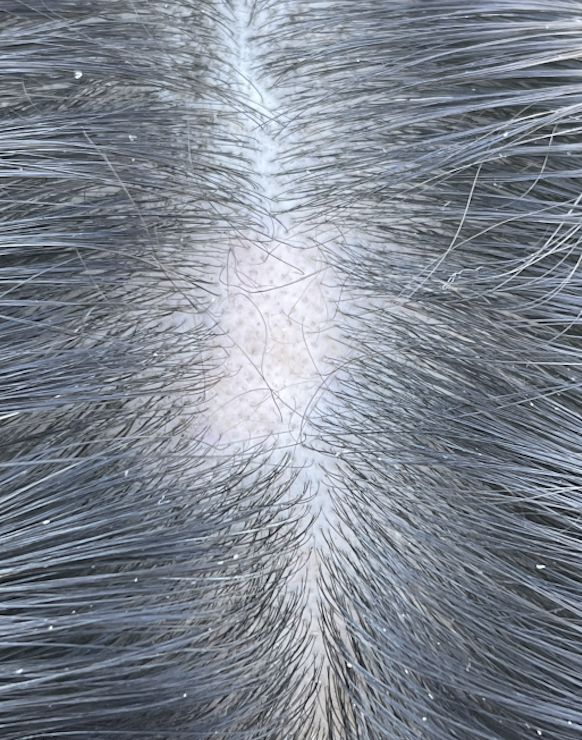
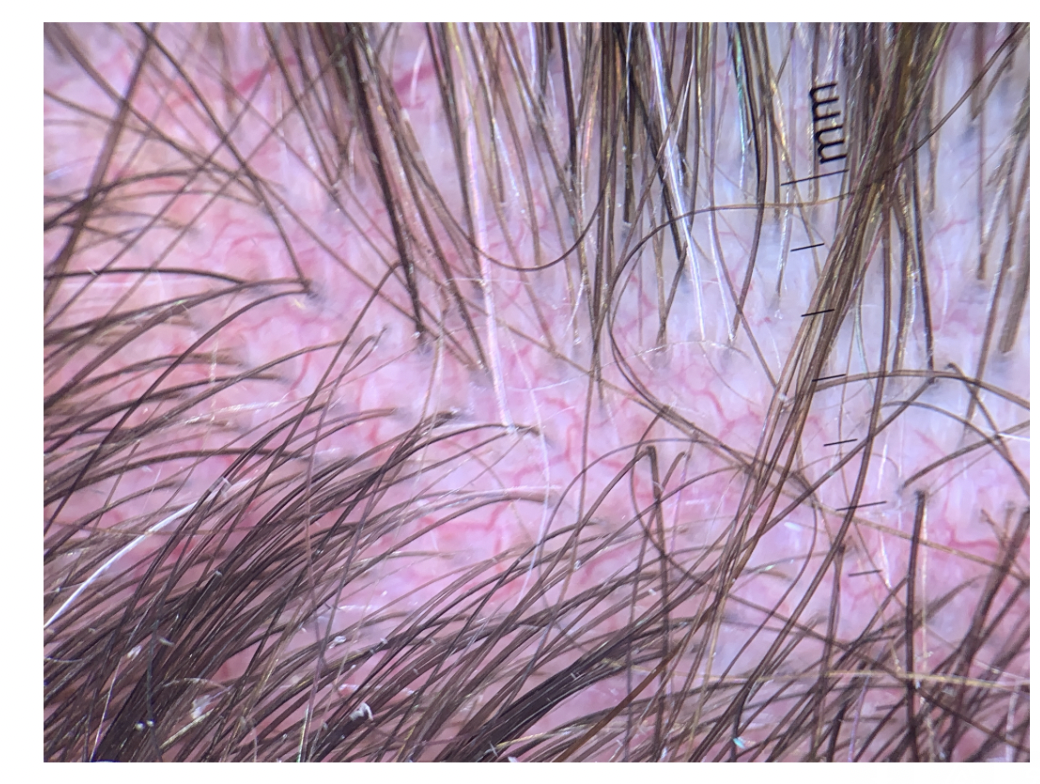
It would seem that with these short hairs you describe (70% less than 2cm) that we are dealing with some kind of advancing androgenetic alopecia. The presentation of androgenetic alopecia in the context of alopecia areata incognita can certainly be complex.
The first issue that will need to be addressed is the diagnosis and then treatment can be discussed.
It would be less likely that a true CTE is present here. The main issue here is an accumulation of short hairs.
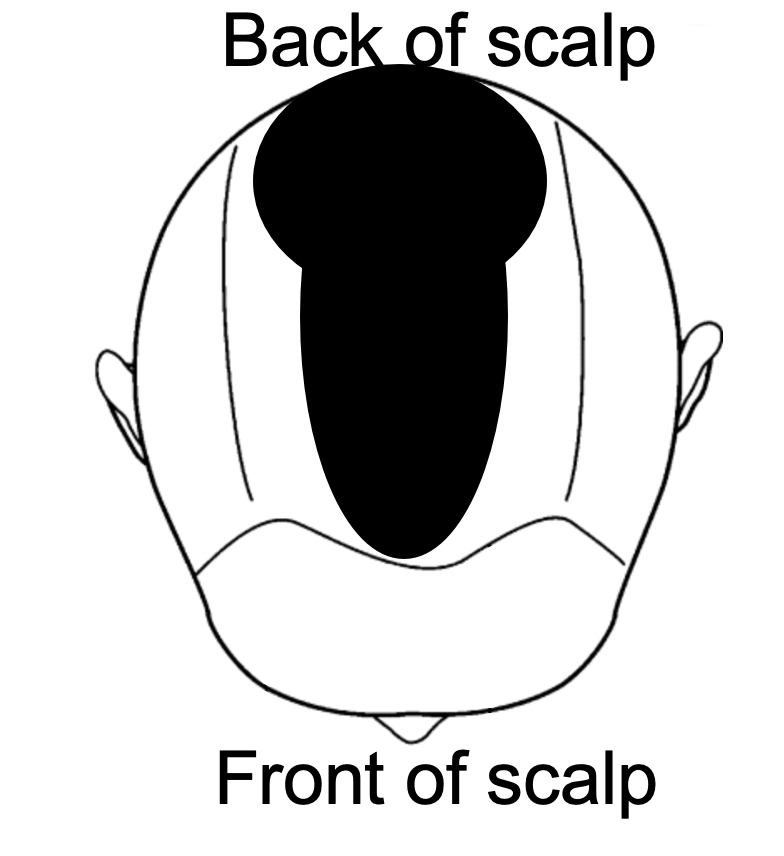
So what is the diagnosis?
The main question is what is the MAIN diagnosis now. Is it mostly androgenetic alopecia ? Is the alopecia areata incognita contributing a significant role right now (or is it quiet)?
Trichoscopy and possibly repeat biopsy could be helpful.
It is important to know what is the main diagnosis as that influences which treatment to consider.
It would seem that the most likely is that there has been an acceleration of androgenetic alopecia and this is the most relevant issue right now. However, trichoscopy and biopsy can guide things.
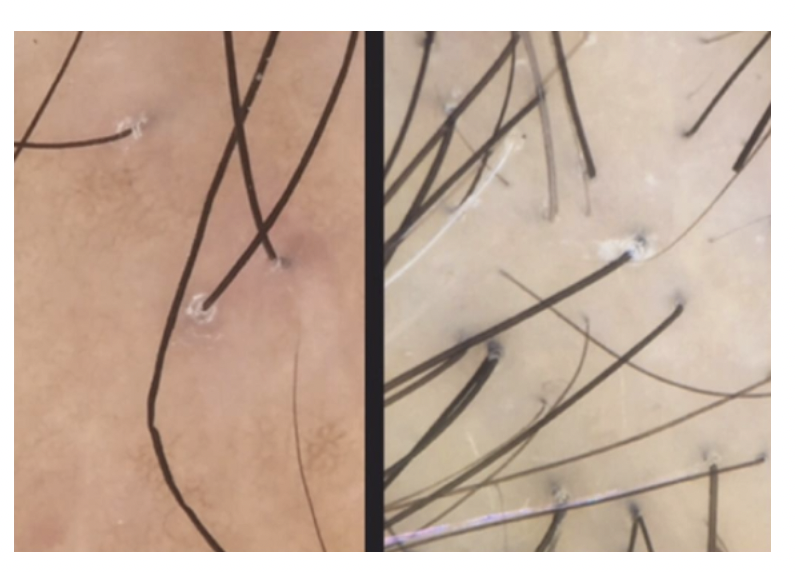
I’m also a big fan of hair collections in these complex situations. This is known as the “5 day modified hair wash test”. Hair collections allow us to see how many short hairs there are (like you have said) but also allow us to see how many ‘dystrophic’ hairs there are. These include abnormally shaped and broken hairs. If there are a lot of dystrophic hairs, then I am a little more likely to feel that a 1-2 month course of oral steroids is worthwhile to see if the shedding can be shut off. That in and of itself is a therapeutic trial and gives valuable information – if the shedding shuts off dramatically with a course of steroids, we know this is not all due to androgenetic alopecia.
Finally, in these sorts of situations, I often will order some blood tests. The exact tests I like to order depends on the patient’s full story. I don’t have your full story so it’s not possible to say all the tests that are needed. Tests for LH, FSH, estradiol are helpful as rarely the acceleration of AGA and poor sleep have been seen in some of our patients in the context of premature transition to menopause. A day 3-5 FSH that is within normal range is reassuring. In general, if menstrual cycles are regular, that is also reassuring that there is not likely a concerning hormonal issue.
I can only imagine that you have had many tests for TSH, ferritin. You probably don’t need those repeated.
What needs to be excluded here as well is that there is any sort of autoimmune issue arising or any sort of COVID related issue (longCOVID) that is present. Of course, that can only be ascertained by history. There are a variety of complex shedding issues that can occur and a full history to exclude autoimmune or hormonal issues is really important and necessary. I would not say that all patients with chronic shedding like this need an ‘autoimmune work up’ but certainly if there is abnormal fatigue, joint pains, Reynaud’s, photosensitivity, it does now become important.
Finally, I’m not 100% convinced that COVID shedding always shuts off perfectly so if a patient had COVID 19 in the past, this needs to be addressed.
But assuming the hair loss is androgenetic alopecia, I believe there are a few options to consider:
1. slowly increasing topical minoxidil 50% -100% above current levels.
2. adding oral minoxidil back to the plan at 0.25 mg once daily and very slowly moving to 0.5 mg
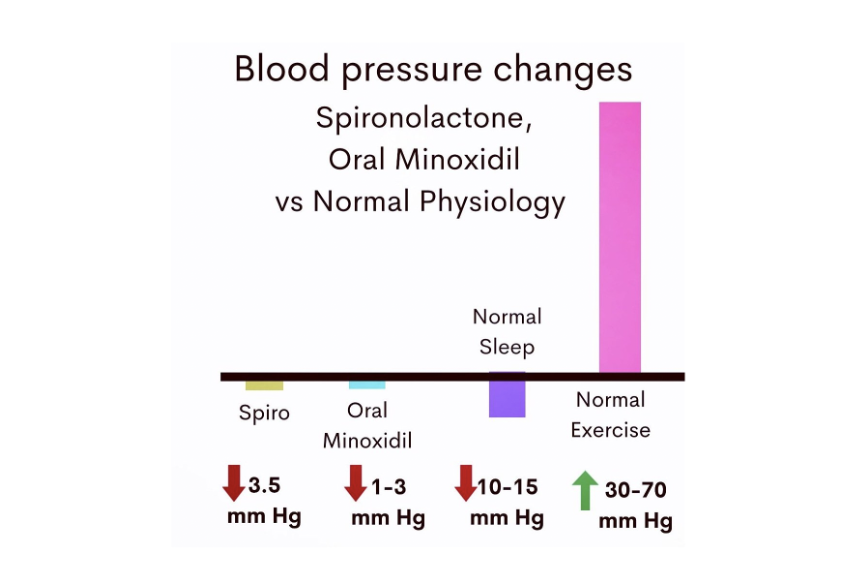
3. adding oral spironolactone 50 mg with the finasteride.
4. using topical minoxidil compounded with cetirizine 1 % or topical minoxidil compounded with latanoprost 0.1 % or retinoic acid
5. Considering PRP therapies or low level laser therapies
6. Considering topical minoxidil compounded with latanoprost 0.1 %
Option 1: Slowly increasing topical minoxidil 50% -100% above current levels.
It does seem that oral minoxidil helped you. The goal then is to attempt to use more without using so much that it affects your sleep or causes cardiovascular complications. It might not be possible but it is worth considering.
The first step may be to use more topical (local) minoxidil. I’m not sure how much you use but it may be worthwhile in these situations to increase to twice daily or simply use more.
I can’t comment specifically in your situation but some of my own patients will use 5 % Rogaine foam a full cap (or more) under appropriate supervision.
Using more may make sense.
These agents may also help any alopecia areata incognita component if it is present.
Option 2: Adding oral minoxidil back to the plan at 0.25 mg once daily and very slowly moving to 0.5 mg.
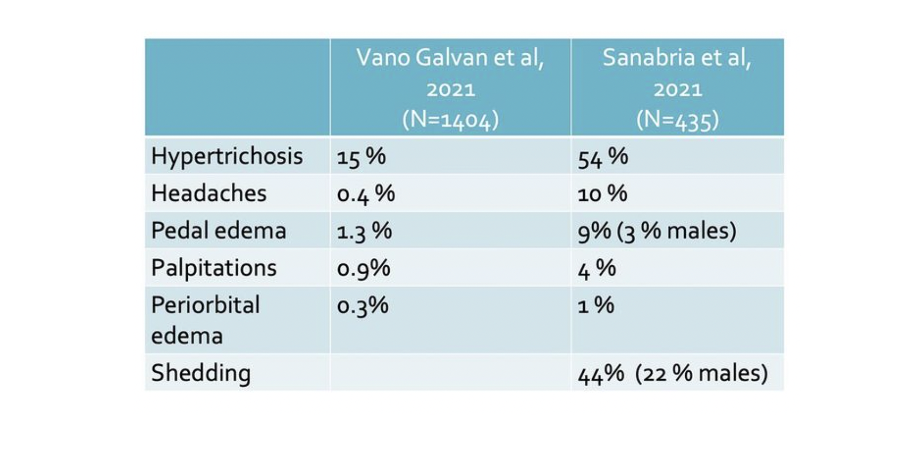
I have had patients with sleep problems with 1.25 mg and higher doses but some patients have noted significant improvement in sleep with 0.25 mg or 0.5 mg taken in the morning. Not all patients find the lower doses improve sleep, and in fact, studies by Sanabria and colleagues did not find that there was a clear trend towards lower doses being associated with lower chances of sleep problems. These small doses may help some patients (especially when combined with other treatments like those discussed in option 1, 3, 4, 5, 6).
These agents may also help any alopecia areata incognita component if it is present.
Option 3: Adding oral spironolactone 50 mg with the finasteride.
If the cause of the acceleration of hair loss is truly the androgenetic alopecia, then more aggressive treatment of the AGA makes sense. This includes more minoxidil or more antiandrogens, or PRP or laser.
Spironolactone and finasteride have different mechanisms of action and some patients can combine them. You and your doctors can review if this makes sense or not but it could add further benefit for some patients.
Option 4: using topical minoxidil compounded with cetirizine 1 % or considering topical minoxidil compounded with latanoprost 0.1 %
There are options to add additional ingredients to the topical minoxidil. For some patients, adding more retinoic acid helps. For others adding cetirizine or latanoprost could help.
These agents may also help any alopecia areata incognita component if it is present.
Option 5: Considering PRP therapies or low level laser.
There are options to add PRP or laser for some patients. Both of these may (theoretically) help alopecia areata incognita and androgenetic alopecia. These are probably less effective than the options outlined in 1-4.
Final Comments
Thank you again for the question. I do think it’s likely that the AGA has accelerated after stopping the oral minoxidil. In situations like this, I do find that use of hair collections really helps me (as I can find dystrophic hairs and get a good count of telogen vellus hairs). Sometimes a hair collection helps me identify rare situations too – like a late onset loose anagen hair syndrome, for example.
You are very knowledgeable about your hair and I would encourage you to discuss a variety of these options with your doctors and take each treatment step by step if it is decided that a treatment does make sense to start.
It may be that you never want to return to oral minoxidil again, but it may be that you wish to consider very small doses.
Photos will be important to document progress and so will hair collections (whether formal ones or informal ones).
I thank you very much for sending your question our way and hope this was helpful.
REFERENCE
Sanabria B, Vanzela TN, Miot HA, Müller Ramos P.Adverse effects of low-dose oral minoxidil for androgenetic alopecia in 435 patients. J Am Acad Dermatol. 2021 Apr;84