Should I increase my oral minoxidil ?
I’ve selected this question below for this week’s question of the week. It allows us to review some concepts in use of oral minoxidil in LPP and the timing of adding it to the plan .
Question
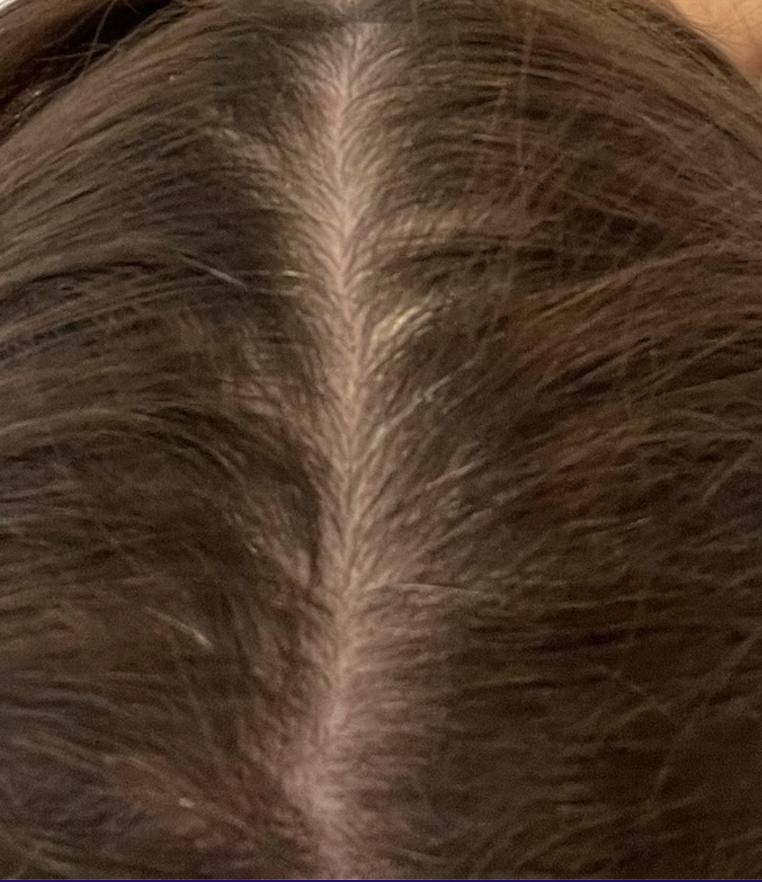
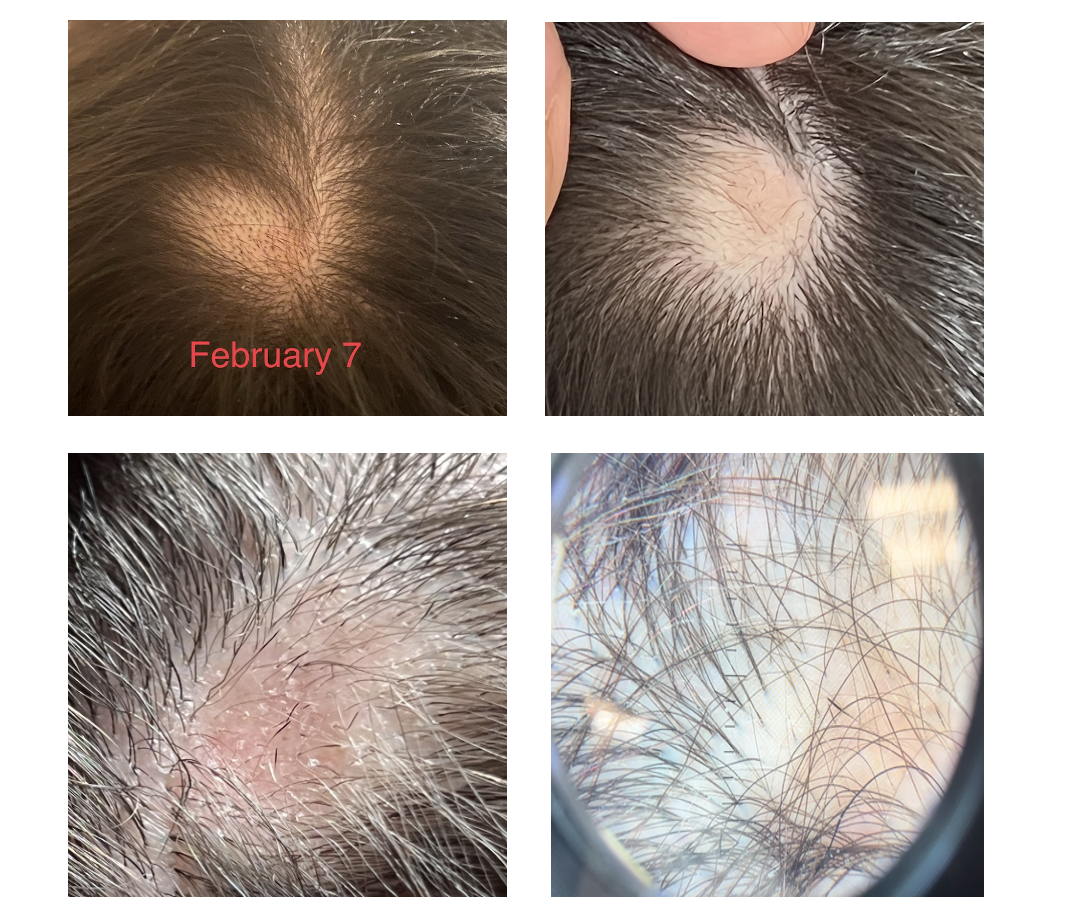
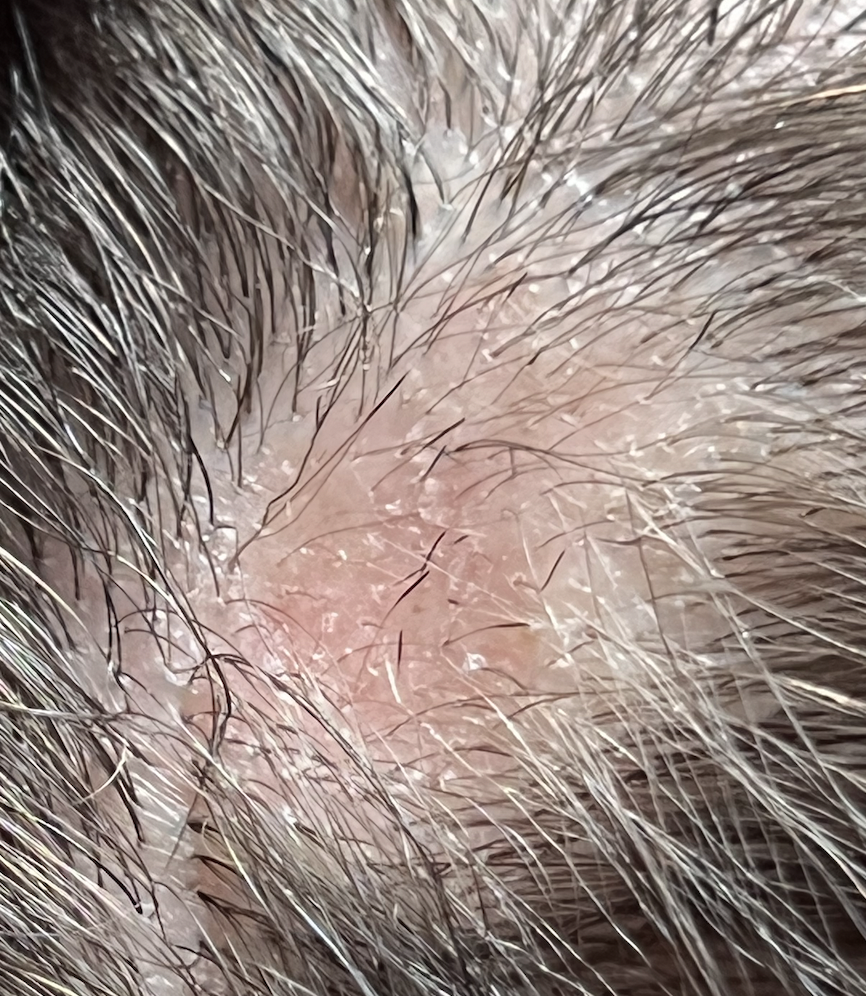
I was diagnosed with LPP in early January 2022. I am receiving monthly injections and take Doxycycline twice a day. My LPP is still active. In early April, I started taking 0.625mg of Minoxidil, increased shedding began three weeks after starting the minoxidil and it doesn't seem to be slowing down.
The shed is extreme and now terrifying.
I am supposed to be increasing my dose soon to 1.25 mg but am concerned. Is this normal to be going on this long and if so, when will it stop or will this continue at this rate?
Answer
Thank you for this question. In order to fully answer all parts of this question, I would need to know more of the story and see the scalp up close. I don’t have all the information but hopefully my answer will help. The short answer is the it’s normal to get shedding and likely it will last 1-2 months.
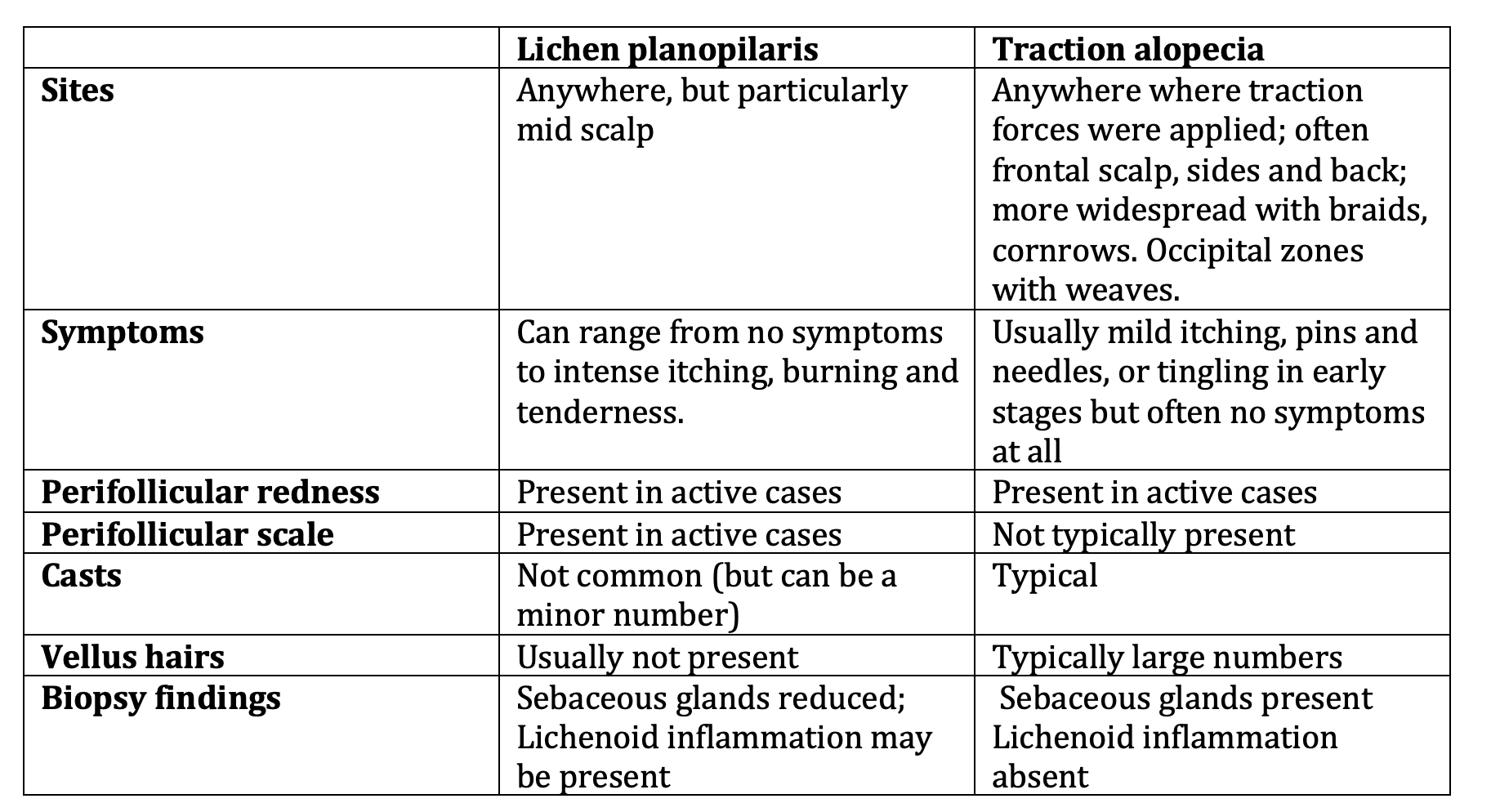
I will assume here that LPP is the diagnosis. What I do not know is whether issues like frontal fibrosing alopecia (FFA), androgenetic alopecia (AGA) or seborrheic dermatitis (SD) are also present.
That is important to know in fully answering this question.
It’s quite likely that the cause of shedding here is the oral minoxidil. This is quite typical and usually lasts 2 months.
What I don’t know there is whether you also have other issues which can contribute to shedding like androgenetic alopecia and telogen effluvium. You and your doctor will want to make sure no other issues that cause shedding are present.
If you haven’t done it already, you’ll want to get blood tests for iron studies (ferritin), thyroid studies (TSH), zinc, and vitamin D. Other labs might be important to get but that will depend on your story and what the scalp examination shows.
You and your doctors can review if other issues that cause shedding might also be present. These include stress, low iron, thyroid problems, COVID 19 infections, other infections, other medications and weight loss. Of course, a sudden increase in the shedding can always be due to the LPP activity suddenly increasing. Whether that’s an issue needs exploration.
My personal preference when treating LPP is to get the LPP under control and then add growth stimulators like oral minoxidil, laser, PRP later on. There’s nothing wrong with adding them right now as you have – but my preference is to wait until the LPP disease activity has really been reduced to minimal levels.
So I add growth stimulators like minoxidil, PRP, laser only when the LPP has been brought under really good control.
Now back to your question. I think it makes sense for someone with your story to continue doxycycline and the steroid injections. You might back down on the steroid injections to every 6-8 weeks and add topical clobetasol. That’s just my preference but there’s nothing wrong with monthly injections. You’ll want to make sure you don’t have atrophy (indents) forming in the scalp.
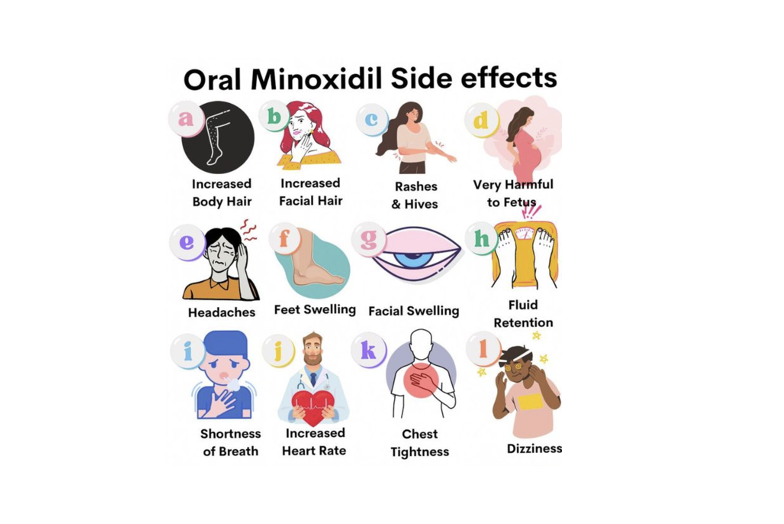
I think the oral minoxidil must continue as you may get hair loss if you stop right now and you may get hair loss if you increase right now. For my own patients with similar stories as yours, I generally advise to continue oral minoxidil for now at 0.625 mg and consider increasing the dose in the future.
I would not increase right now. But that’s my opinion.
I think the key question here is whether or not doxycycline and steroid injections are doing the job fully to shut down the LPP. If not, you might want to speak to your doctors about adding clobetasol or hydroxychloroquine (Plaquenil) or oral cetirizine (Zyrtec, Reactine, etc.) or low dose naltrexone.
You’ll want to make sure that someone checks if you have seborrheic dermatitis. If it’s present, you’ll want to add a dandruff shampoo to your plan. Zinc pyrithione, Selsun blue, ketoconazole and ciclopirox are all common options.
You’ve probably had many labs done, but you’ll want to make sure ferritin, TSH, CBC and vitamin D were done. You and your doctors can discuss others like cholesterol, glucose, hemoglobin A1c.
If there is any evidence of frontal fibrosing alopecia, dutasteride can be considered. Isotretinoin can also be considered in the future - but we don’t use this with doxycycline because of an interaction.
Once the shedding comes under better control (hopefully in a few months), it may be possible to increase the oral minoxidil dose to 1.25 mg. I would not do that now (yet) but that’s just my view.
Overall, my thoughts in a clinical situation (with limited clinical information) like this are to
1) Continue doxycycline
2) Continue steroid injections (reduce to every 6-8 weeks)
3) Continue 0.625 mg Oral minoxidil)
4) Considering adding one or more of the following: clobetasol, hydroxychloroquine, cetirizine
5) Treat any seborrheic dermatitis with anti-dandruff shampoos
6) Make sure labs are done for CBC,TSH, ferritin, zinc, ESR, cholesterol, glucose, hemoglobin A1c, vit D
7) Treat frontal fibrosing alopecia if it is also present (dutasteride may be used).
Be sure to keep close follow up with your dermatologist. I thank you for your question and hope this was helpful to you.