Localized Shedding with zinc supplements
I’ve selected this question below for this week’s question of the week. It allows us to discuss some of the finer aspects of zinc on the human body and how to approach atypical or unexpected reactions in the human body.
Here is the question….
QUESTION
I shed hair when taking zinc supplements. I cannot find any information on this at all. Most suggest zinc helps the hair cycle not cut it short and shed. The shedding appears to occur in locations that already had issues. It is not global (all over the body). Is zinc connected to the hair growth/shed cycle or is it inflammation? Thank you.
ANSWER
This is a terrific question. Not one that I encounter often - but a fascinating one. There’s a lot to review with this question, so let’s get to it!
Before we go further, I’d like to point out that the ideal way to diagnose hair loss is using what I termed the ”Diagnostic S.E.T.” I refer to these as the diagnostic “set” because theses 3 aspects all go together. These 3 items include:
1) the patient’s Story
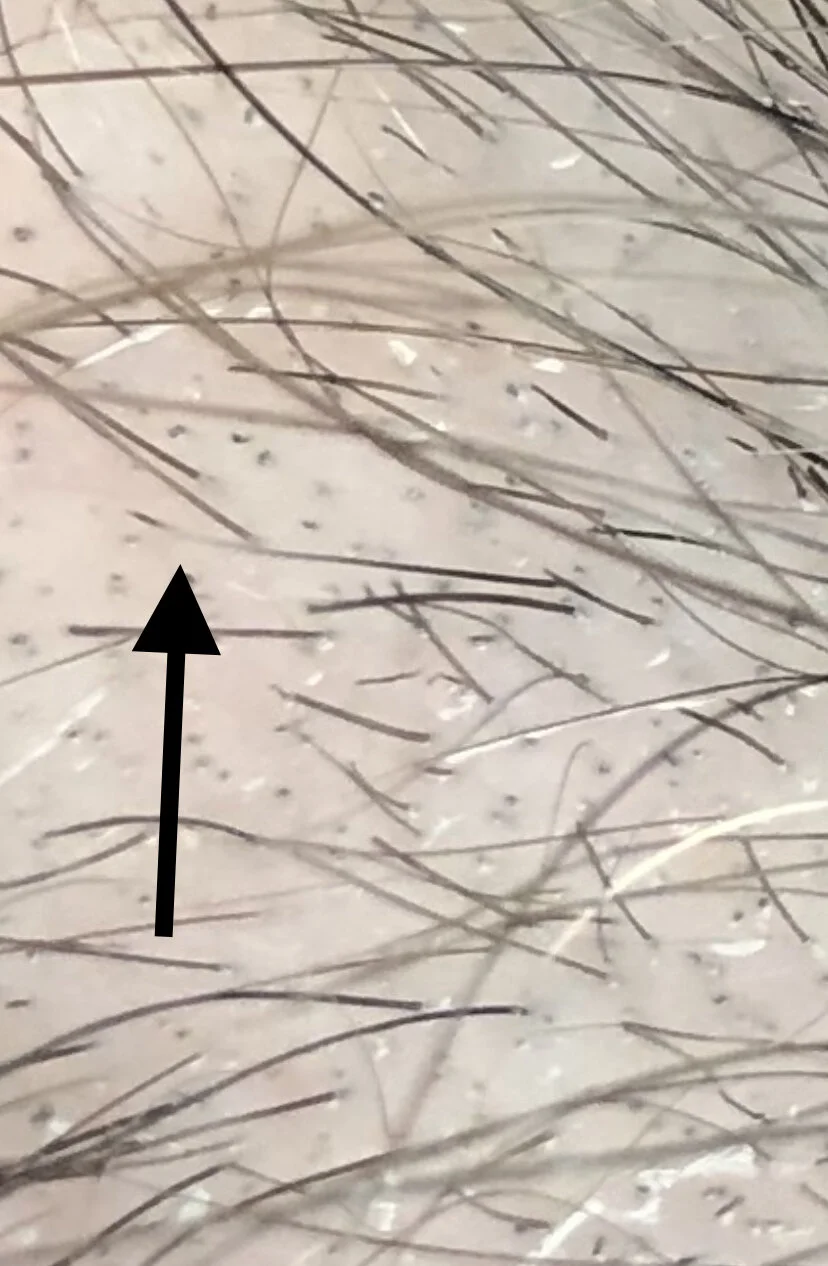
2) the findings uncovered during the process of the scalp Examination and
3) the results of relevant blood tests.
The first letter of each of the three words 1) story, 2) examination and 3) tests spell out the word “S.E.T.” - again a helpful reminder of how the information obtained from reviewing each of these 3 aspects helps solidify a proper diagnosis.
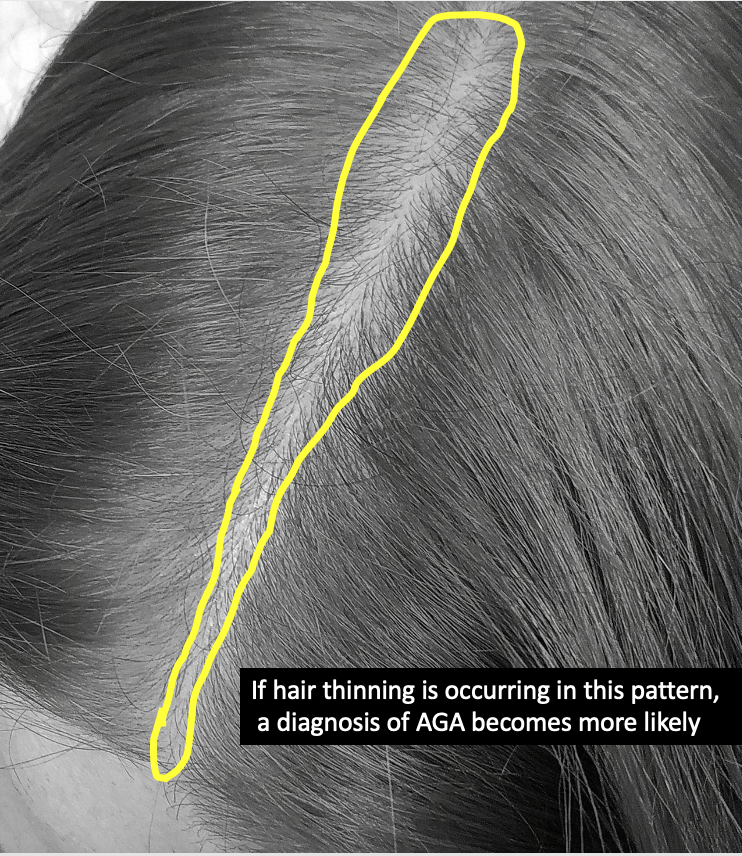
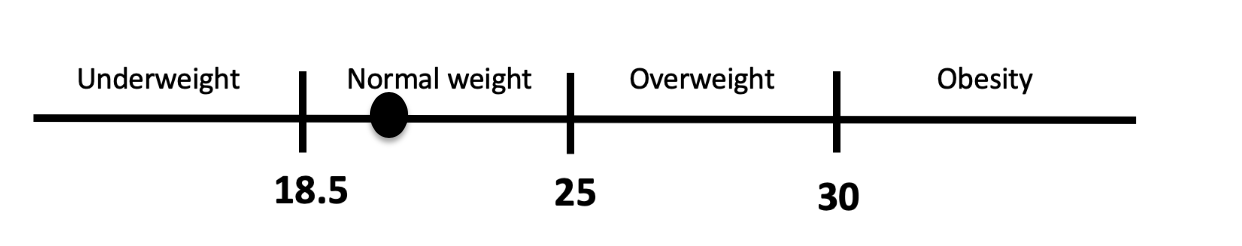
I’d like to know a lot more about this story ideally but of course the magic of the “question of the week” is that I tackle questions with limited information. It could be relevant if the patient takes zinc for one weekend because they heard it was good to boost their immune system or took zinc for one year to finish the bottle that they purchased one day on sale. It could matter if the patient is obese or thin, malnourished or well nourished and elderly or young. It could matter if the patients knows their actual zinc levels through blood tests or not. Finally, it could matter and probably does matter if the patient has early staged adnrogenetic alopecia, mid staged androgenetic alopecia or advanced androgenetic alopecia. All these things matter in fully answering these questions.
With that behind us, let's return to our question of the week again.
WHAT’S THE MOST LIKELY EXPLANATION FOR SHEDDING WITH ZINC?
Well, the most likely explanation (given that I don’t know anything else about you), is that:
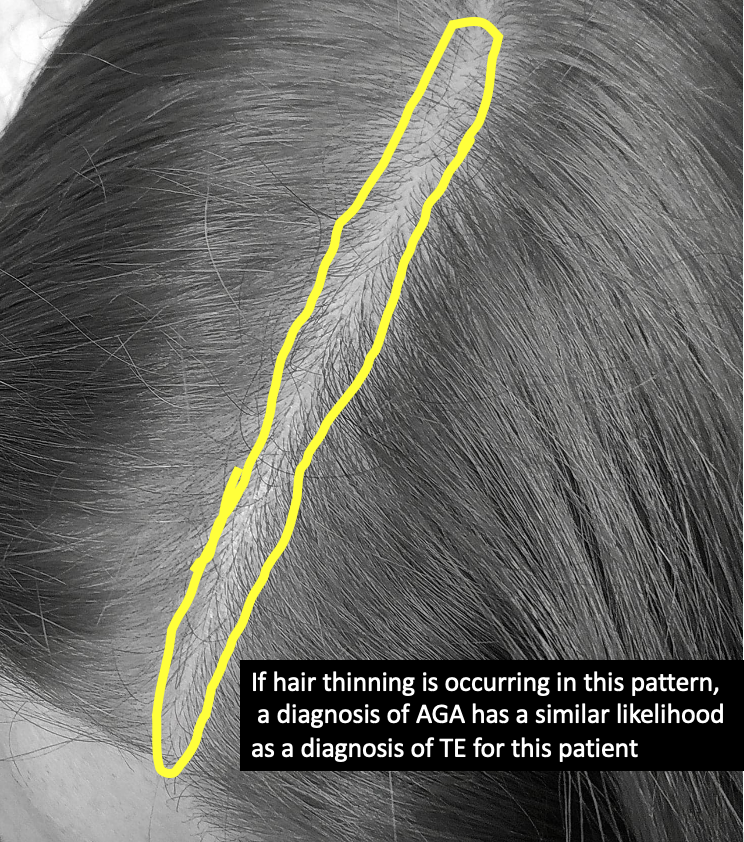
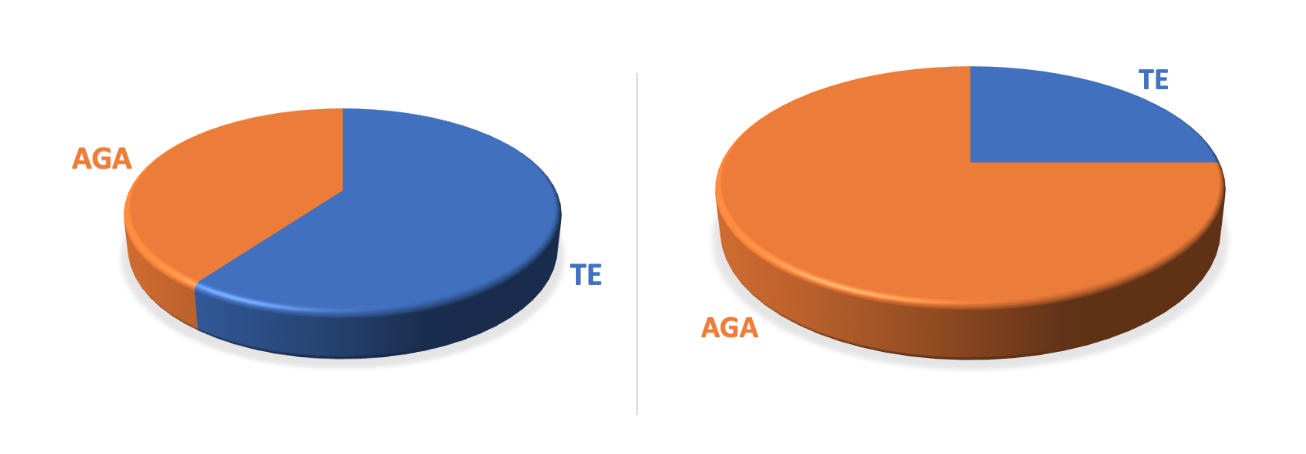
1) you have some male pattern balding and you are not using finasteride or dutasteride to treat your male balding and that zinc has trigger a mild effluvium of hairs that are in the early balding phase. We call this phenomenon immediate telogen release and it’s common with every treatment that acts on male balding including minoxidil, laser therapy, PRP therapy, finasteride therapy …. and sometimes zinc.
2) The second explanation is that you actually do have diffuse loss of hair on the scalp and you are just noticing it more in the areas that are already thin. In this scenario, the male balding has nothing to do with the discussion, it just so happens you notice hair loss more in areas that are already thinner.
3) The third explanation is that you have something else going on that is not related at all.
It zinc related to my hair loss? A Closer Look at the Naranjo Scale
Before we go further, I’d like to introduce you and readers to a wonderful system of determining how likely it is that a person’s rare observation is linked to the drug or supplement they are taking. It’s called the Naranjo Scale. I always refer to the Naranjo scoring system when some observation a patient is experiencing is uncommon because it helps to get a better sense of just how plausible things really are. If someone tells me their new supplement is causing hair loss, I might pull up the Naranjo Scale. If someone tells me their new cat is causing them hair loss, I might pull up the Naranjo Scale. We’ll take a look at this scale in a moment.
Now, it seems pretty obvious that if you say that when you take zinc you get more shedding that I believe you that zinc is causing your hair shedding. First off, I believe you. I have seen this phenomenon before so I’m not introducing the Naranjo scale as a way to prove whether you are correct in your observation or not. Rather, the Naranjo Scale helps us look at causation with a little greater precision - something a bit more scientific.
The Naranjo scale involves use of 10 simple question. You might want to try it yourself. The questions are below and I’ve worded each questions specifically to pertain to zinc although the Naranjo scarring system itself pertains to any drug not just zinc. You answer “yes", "no" or "don't know" and different points are assigned to each answer (-1, 0, +1, +2).
Typical Questions in the Naranjo Scale
1. Are there previous conclusive reports of zinc causing hair loss from areas that already have an issue?
Yes (+1) No (0) Do not know or not done (0)
2. Did the shedding appear after zinc was given?
Yes (+2) No (-1) Do not know or not done (0)
3. Did the shedding improve when the zinc was discontinued ?
Yes (+1) No (0) Do not know or not done (0)
4. Did the shedding appear when the zinc was readministered?
Yes (+2) No (-1) Do not know or not done (0)
5. Are there alternative causes that could have caused the shedding?
Yes (-1) No (+2) Do not know or not done (0)
6. Did the shedding reappear when a placebo was given?
Yes (-1) No (+1) Do not know or not done (0)
7. Was the zinc detected in the blood at higher levels?
Yes (+1) No (0) Do not know or not done (0)
8. Was the shedding more severe when the zinc dose was increased, or less severe when the zinc dose was decreased?
Yes (+1) No (0) Do not know or not done (0)
9. Did the patient have a similar shedding to the same or similar zinc pills in any previous exposure?
Yes (+1) No (0) Do not know or not done (0)
10. Was the adverse event confirmed by any objective evidence?
Yes (+1) No (0) Do not know or not done (0)
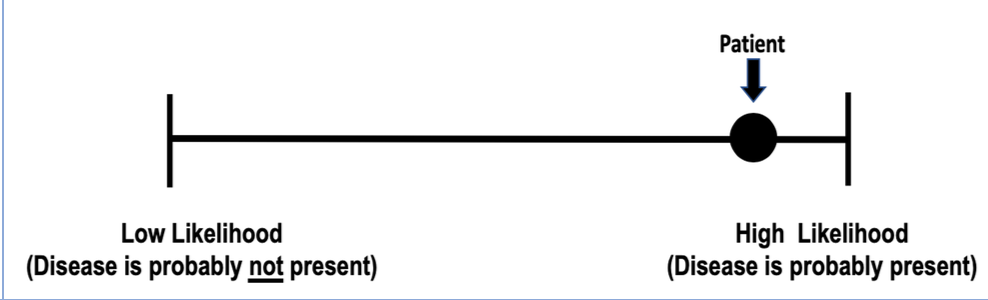
Determining the Naranjo Score
Scores for the Naranjo Scale can range from -4 to + 13. A score of 0 or less means the likelihood of the drug causing the side effect is doubtful, a score 1 to 4 indicates it is 'possible', a score 5 to 8 means it is 'probable' and a score 9 to 13 means it is 'definite'. The website http://www.pmidcalc.org/index.php provides a free online calculator for clinicians to calculate the Naranjo Score. It is easy to use and has been embedded below as an example. Individuals wanting to know if a specific drug caused hair loss should be sure to speak to their dermatologist. For you, I’m guessing you are somewhere between 5 and 8 and probably and 6 or 7. This just simply reinforces that what you are experiencing is probable.
What are the effects of zinc on the body and on hair ?
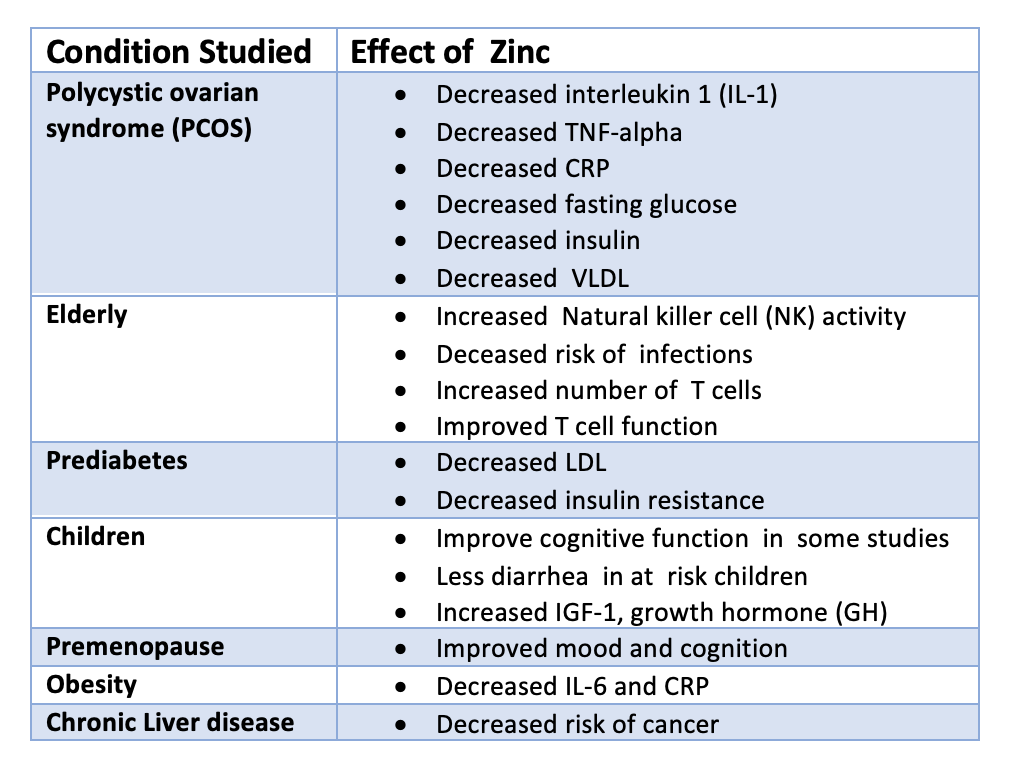
Zinc is well known to affect the human body in about 50 different ways. Actually, it’s best to say that there are at least these are the 50 different ways that have been studied. There are probably 250 ways that zinc affects the human body - we just haven’t studied them all. Here are some of the more common effects of zinc under different conditions. You can see that zinc has a profound effect on many hormones, inflammatory markers and immune system components.