Nowadays, do-it-yourself (DIY) projects are very popular. A "DIY" Project is an activity that one undertakes without directly seeking the help of an expert. You're probably well aware that DIY is particularly popular among individuals interested in home renovation. There are countless numbers number of books and videos to guide the lay person to renovate their home from top to bottom, inside and out. DIY need not be limited to home decor; the concept of DIY extends broadly into so many aspects of our lives nowadays. The internet is full of DIY projects.
On account of the internet, DIY also extends into medicine. The public is increasingly looking to take control of their health and in the same light to have more autonomy to decide how they receive advice on their health. We are all familiar with the power of modern search engines. My patients often joke about what they learned form "Dr. Google". However, the reality is clear: patients are spending more and more time looking for reliable information from the internet. We know that a vast majority of patients search for health information online. Various studies have suggested that 25-50 % of individuals seek the internet for self diagnosis.
I'm not a great fan of self diagnosis (i.e. DIY diagnosis) when it comes to hair loss. In my opinion, attempting to self diagnose the cause of one's own hair loss is rarely wise. Unless an individual has had a comprehensive review of their medical history, a full examination of their scalp (including use of dermoscopy) and had blood tests, they have not yet begun to properly investigate their hair loss.
.
Why are we self-diagnosing anyways?
There are many reasons why individuals want to diagnose their own medical health, including hair loss. It's certainly much faster and more convenient to look on the internet than take the time to go to a doctor. For many, it may also present a considerable cost savings as well. For others, there is a tremendous amount of fear that surfaces when one needs to face their own health issues with a doctor. It's easier for a person with hair loss to avoid this by trying to solve one's health issues themselves. For others, looking at information on the internet provides a much needed sense of autonomy over health-related decision making. The public increasingly wants control over their health and how decisions get made and who makes them. When it comes to hair loss, however, it's often a false sense of control.
Why I don't encourage self-diagnosis
I realize that patients generally want to try to figure out the cause of their own hair loss by themselves. Fundamentally, this is good. Most of us are naturally interested to understand our own health. What concerns me is when individuals attempt to diagnosis their hair loss without the help of an expert (by definition, a DIY Project). There are several considerations I'd like patients to think about as they consider going down one of these paths to self diagnosis.
DIY Consideration 1. All Humans have Bias
'Bias' is a term that means that we have a tendency to make certain decisions based on our previous life experiences. Essentially, the way our brains are wired based on all our collective life experiences and previous knowledge makes it more likely for us to make certain decisions than others. For example, when you see your child fall to the ground crying while playing with a group of children, your instinct may gear you up to look for the exact child that could have pushed your child. This is bias. The reality could be that your child could have tripped on an untied shoelace. We are wired to think certain ways.
When it comes to thinking about the causes of our hair loss, we have biases. For example, most of us really don't want to be diagnosed with genetic hair loss, so our bias could easily cause some of us to consider other diagnoses as the top choice. For example, you remember a family member with balding or someone you saw in the grocery store with hair loss, and your own emotions tell you that this is not what you want to have as a diagnosis. You have a natural bias to think you might have another diagnosis than genetic hair loss.
"There is absolutely no one in my family with balding, so my hair loss must be from stress"
This is bias. Bias is all around us. We are all humans and we are all filled with bias. But as a physician, I am likely filled with less bias when examining a patient's hair loss than the patient is
Bias often leads to Forgotten Information
It's normal to be biased because after all, we're human. Bias can sometimes be a good thing, and certainly the instinctive reactions that come with bias sometimes do help us. In the example above, the bias we have when we hear our children cry helps us protect our children. But time and time again, I have witnessed how bias leads to some components of information to be forgotten.
The the past few years, I have made it a priority to have patients in my clinic complete a very detailed questionnaire about their hair loss long before meeting me. Most of my patients complete this questionnaire in the comfort of their own home, days or weeks before their appointment date. My hope in doing so is to reduce the bias that comes from face-to-face meetings with a physician. Although it's true that 'white coat syndrome' itself can influence what patients remember about their health, there many other aspects of the visit to the clinic introduce bias.
Since introducing the questionnaire some years ago, there has been a significant reduction in phone calls and emails after the appointment from patient's that 'forgot' to tell me certain pieces of information. My hope is that, by using this questionnaire, we're cutting down on bias that exists in standard patient-doctor interviews.
Physicians Have Bias Too
I too am filled with bias. When a close friend asks me about their hair loss, my 'gut reaction' is that I don't want them to have some systemic illness that is contributing to their hair loss. I don't want the strands of hair they pull from their scalp to be due to some serious disease. I need to recognize that I have bias and do my best to remove this from the decision making algorithms.
In fact, when discussing hair loss with friends and family, it's really best that I remove myself from the situation altogether. Legally and ethically, most physicians are not permitted to offer diagnostic or treatment advice to their closest friends and family. Medicine has recognized that physicians have bias and they are not able to properly evaluate an individual who close to the physician. If one of my family of friends has hair loss, I'm supposed to ask them to see a colleague. Sounds strange, but real bias is real!
DIY Consideration 2: Not everyone knows about the 'zebras'
Self diagnosis (hair loss DIY diagnosis) is also dangerous because there is often an assumption by the individual that they appreciate all the various causes of hair loss that exist and simply need to choose which one fits best. To the individual, they mistakenly feel that all the cards are on the table and they just need to pick the right one. The reality is that most patients considering their own diagnosis do not in fact appreciate all the 100 causes of hair loss. Instead of choosing from a list of 100 causes, many individuals with hair loss are trying to choose from a short list of common causes of hair loss. Fortunately, many patients will get their diagnosis right (because common hair loss conditions are common), but unfortunately too many patients get it wrong.
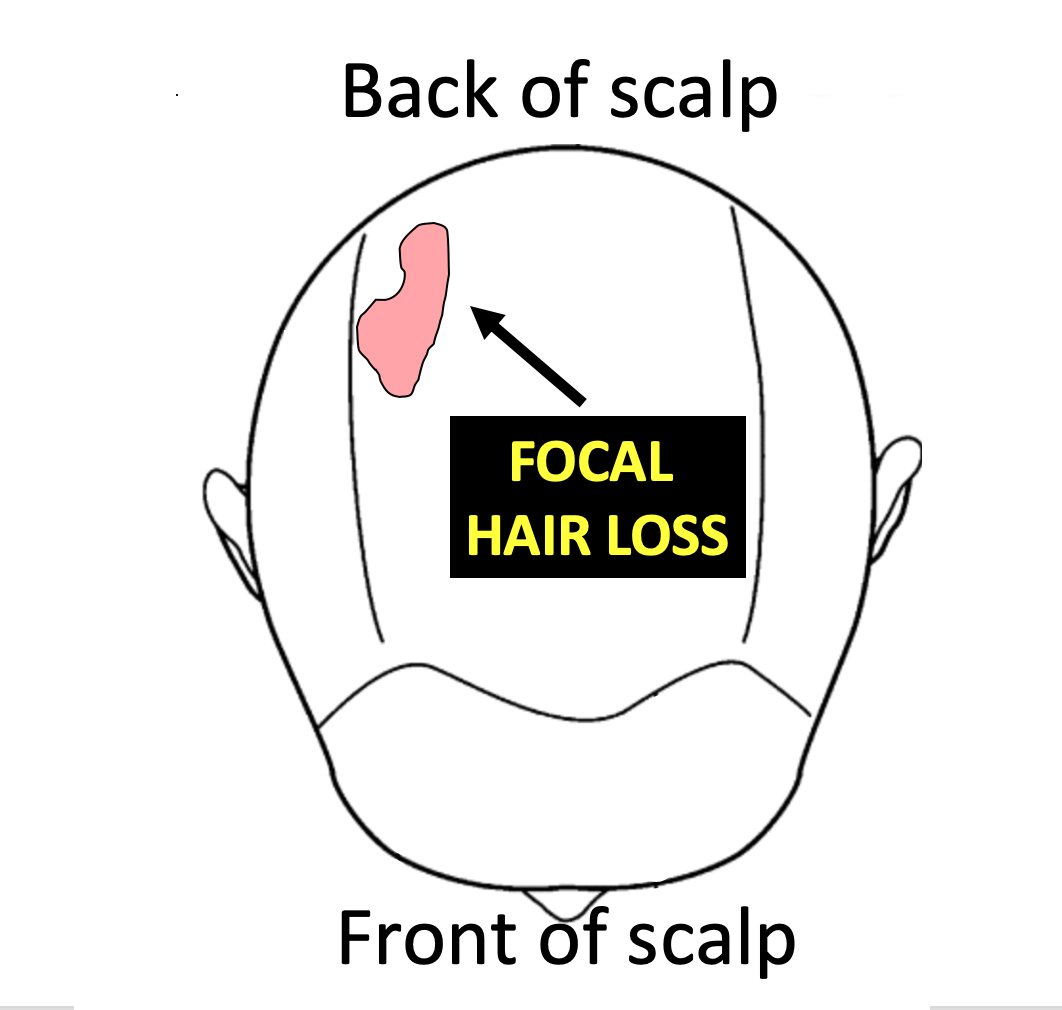
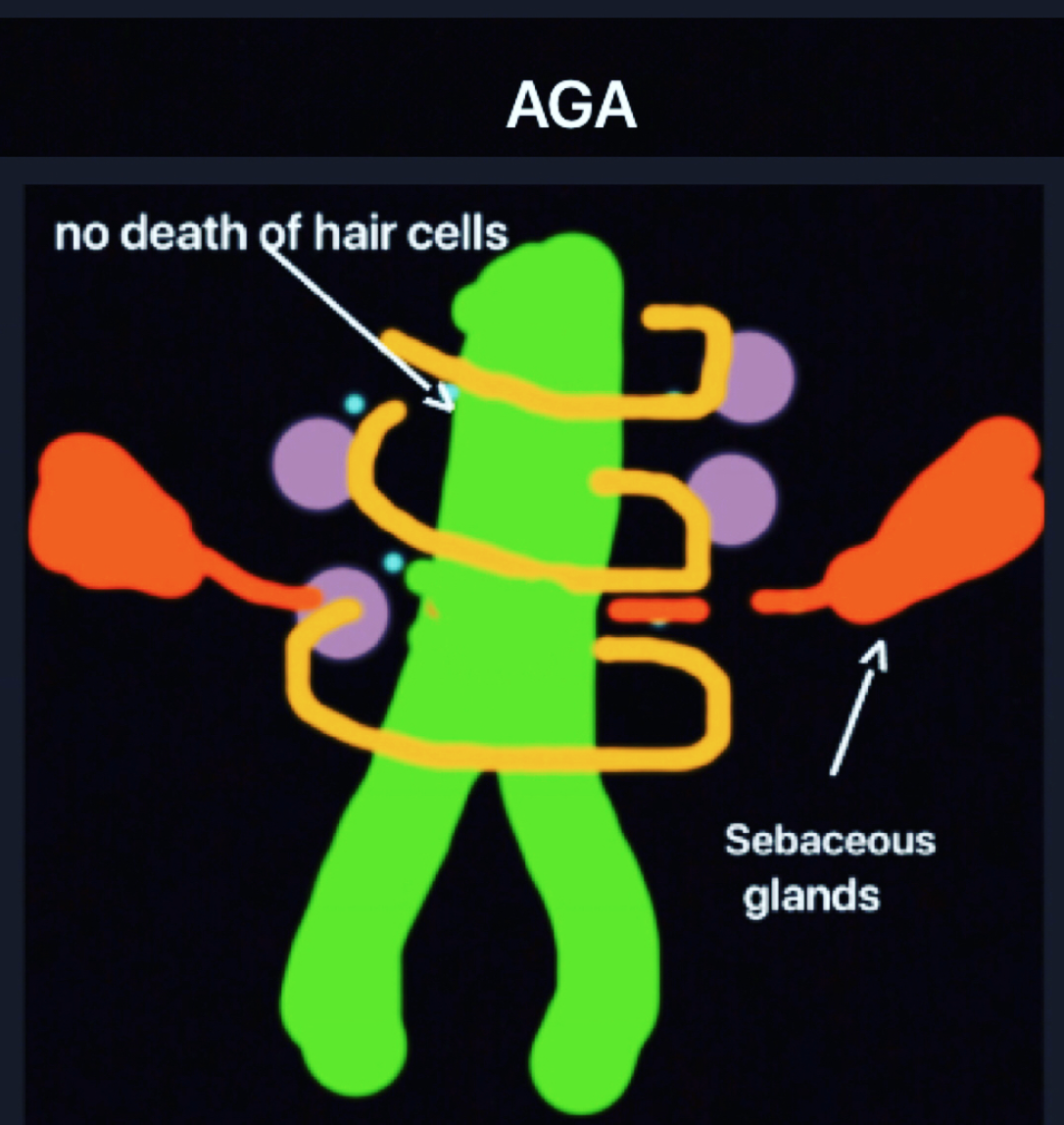
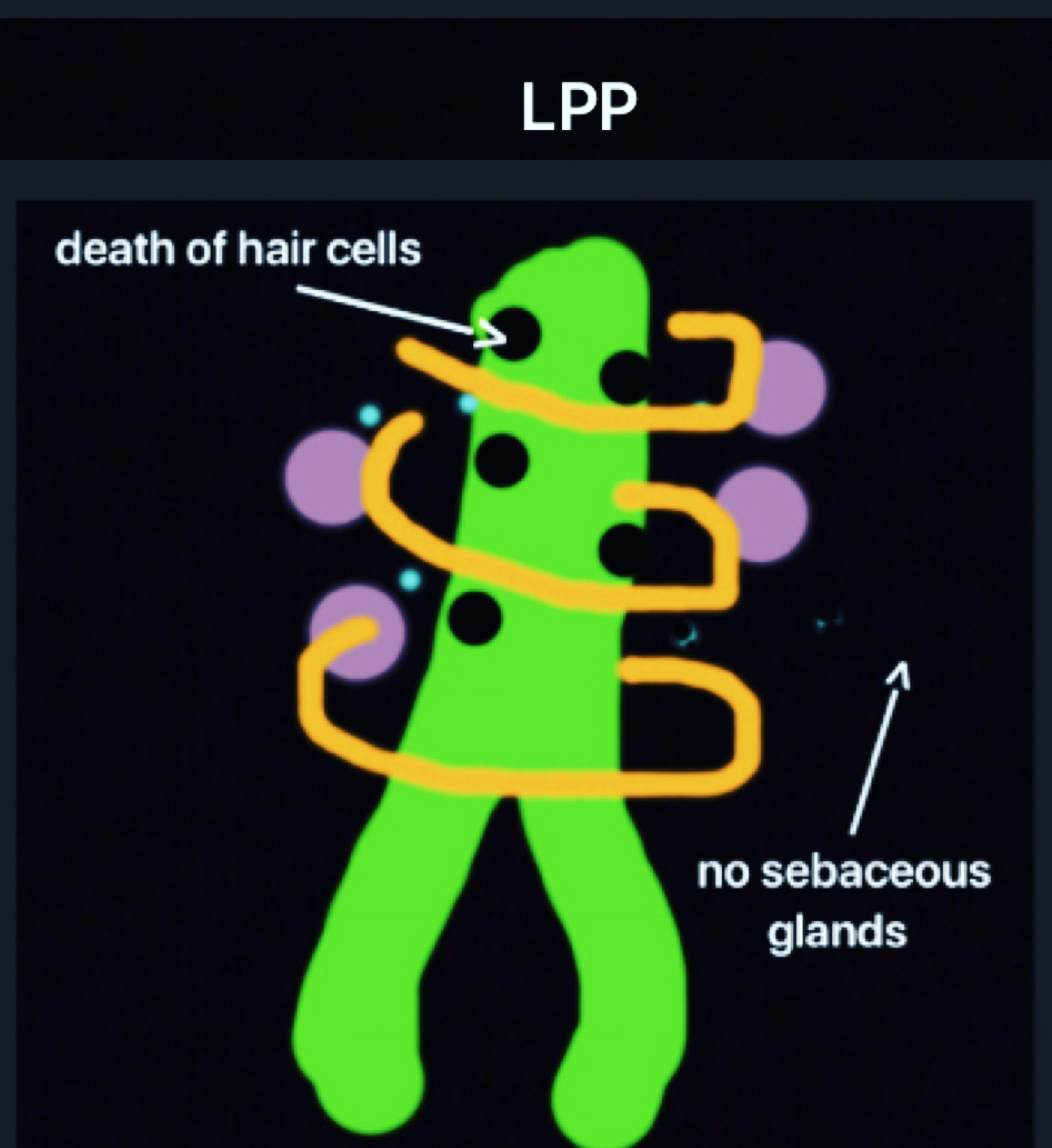
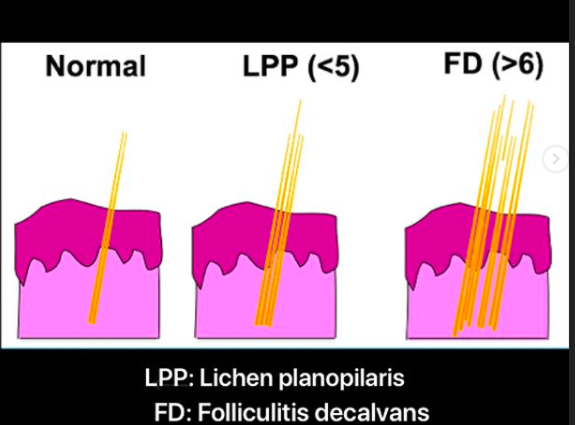
if you've never seen a zebra before, you'll be quite likely to call it some type of horse. Perhaps a striped horse. Dog owners with more exotic breeds will tell you that few people ever get their dog's breed correct. If you've never seen or heard of the hair loss condition 'pseudopelade', you're likely to incorrectly call a circular patch of hair loss 'alopecia areata'. If a patient has never seen folliculitis decalvans, then they are likely to go on battling what they think is stubborn folliculitis for a long time. If a patient has never heard of the condition lichen planopilaris, they may be continually searching for newer strategies for treating their stubborn dandruff or eczema.
Attempting to self diagnosis one's hair loss can be challenging if one does not know all the potential entities on the list.
DIY Consideration 3: Most are On the Lookout for Only 'One' Diagnosis
In my experience, everyone with hair loss is on the lookout for the cause of their hair loss. However, very few people take the time to consider that they could have more than one cause for their hair loss. For many patients, it's not so much of a decision as to whether they have androgenetic alopecia or telogen effluvium but rather what proportion of the patient's hair loss is from androgenetic alopecia and what proportion if from telogen effluvium. Many patients have both! It's possible to have one, two three, four or even five causes contributing to one's hair loss.
DIY Consideration 4: The Hair Follicle is More Complex Than Your Car and Few of us Venture to Fix our Own Cars
The hair follicle is incredible. It's also incredibly complex. There are 20 different cell types in the hair follicle and 100,000 hairs on the scalp (2-4 million on the entire body). Added together there are trillions and trillions of cells working together in the scalp. Can one really try to sort through the actions (or inactions) of trillions and trillions of cells themselves?
It's difficult to think in terms of such large numbers, so let's go smaller. A car, they say, has over 30,000 parts when you consider all the tiny components. Few of us venture to even guess what's gone wrong when our car breaks down. We (hopefully) seek an expert. I often say to patients that if my car was making strange, strange noises and blowing black smoke out the back and front, I would likely be told to get an automobile mechanic to check things over. Any attempt at self-diagnosis and fixing the car oneself would not be wise, at least for most people. It certainly would not be wise for me. When my car breaks down, I need someone who works with cars and knows exactly how things go wrong. I need an expert.
DIY Consideration 5: Some diagnoses can only come from advanced tests meaning that an individual in such cases will never determine their diagnosis themselves.
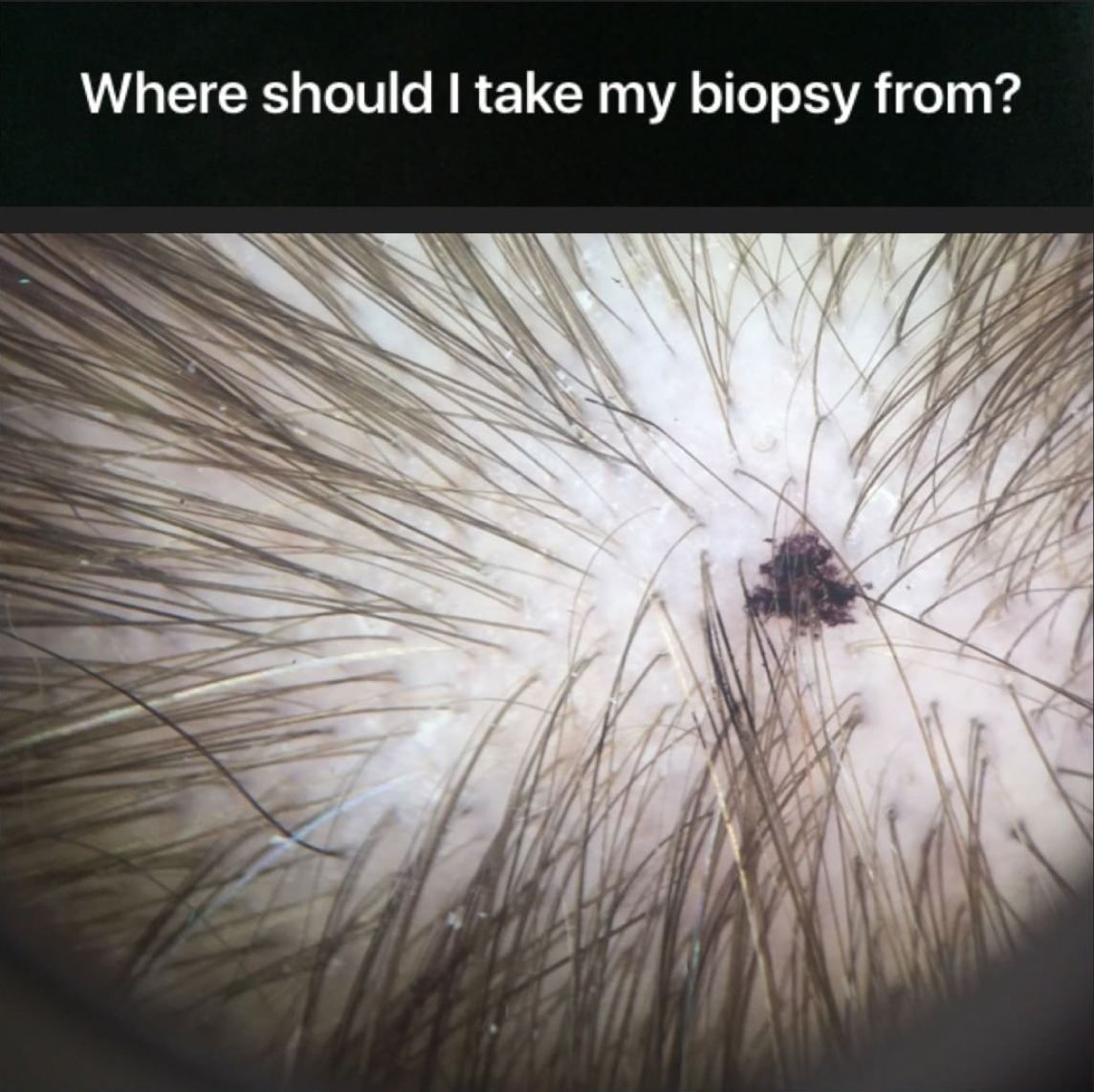
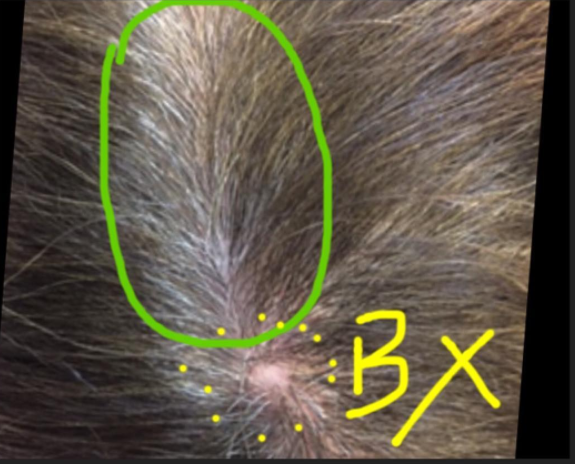
It is important to keep in mind that some diagnoses can only come from a biopsy and some diagnoses can only come from blood tests. Individuals attempting to diagnose the cause of their own hair loss may never reach their diagnosis unless they have these specific tests performed. A patient with hair shedding may think they have a vitamin deficiency or some other cause of telogen effluvium. However, a biopsy could reveal that the hair loss was actually from a scarring alopecia. Similarly, a patient with hair shedding may think their hair loss is simply from stress when the reality is that they have low iron levels from a life-threatening bleeding stomach ulcer.
In these cases, any attempt to try to self diagnose one's hair loss simply leads to a delay in getting the appropriate medical attention that is needed. Rarely, this delay in diagnosis can have serious consequences.
DIY Consideration 6. Patients who self diagnosis often fall prey to online marketing
Finally, a high proportion of individuals who attempt self diagnosis end up spending hundreds and sometimes thousands of dollars on products and supplements they have seen online. The patient's vulnerable state makes them very susceptible to consider buying anything that could help. Online marketing is remarkably powerful. Supplements, pills, shampoos, vitamins, tonics can all be bought with a click of a button. And often are.
Conclusion
I've read many Do-it-Yourself books on various topics and I'm all for liberating people to take on new challenges. DIY self diagnosis, however, is rarely a good idea.
I'm not one to judge how patients want to access their health care. Certainly patients are spending more and more time looking for reliable information from the internet and there are many reasons why individuals want to self diagnose the reasons for their own hair loss. However, properly diagnose hair loss one needs the full story, not the abbreviated version. And to properly diagnosis hair loss one needs the story told with as little bias as possible. Second, a full examination of their scalp (including use of dermoscopy) is needed. There are many mimickers of hair loss and one needs to know all the potential mimickers to make a proper diagnosis. Finally, one needs to have blood tests to complete the basic work up.
Reference
1; Danielle Ofri, MD What Patients Say, What Doctors Hear (Beacon Press, 2017). Reprinted with permission from Beacon Press.
2. Jerome Groopman. How Doctors Think. Houghton Mifflin 2007