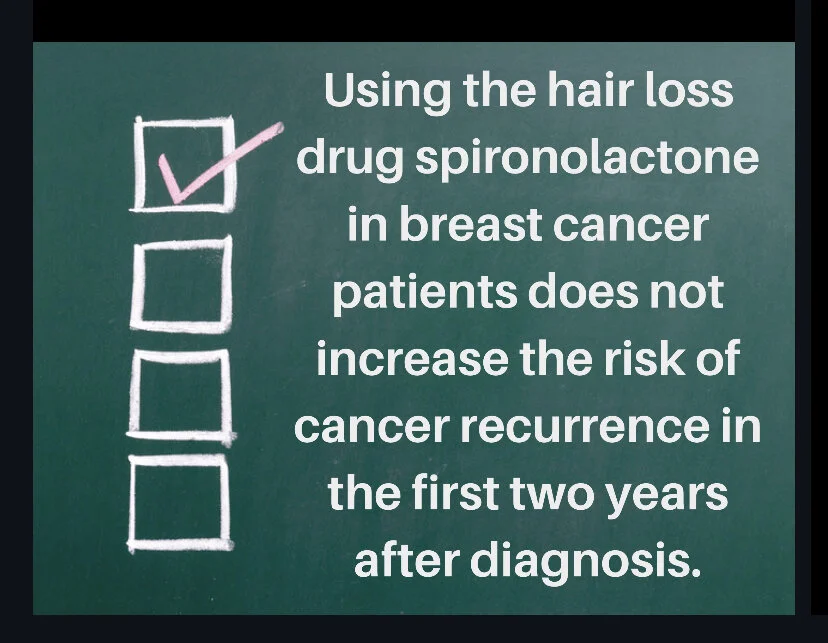
Spironolactone for Hair Loss: Can it be prescribed for patients with prior breast cancer?
Is Spironolactone Safe to Use in Patients with a Prior Diagnosis of Breast Cancer? Does it affect the chance of Cancer Recurrence ?
A new study examined whether the anti androgen pill spironolactone is safe to use if someone had a previous diagnosis of breast cancer.
About three studies to date have suggested that spironolactone does not increase the risk of breast cancer. However studies to date have not examined if using spironolactone once a patient is diagnosed with breast cancer confers any increased risk.
Estrogen levels are slightly increased in about one quarter of breast cancer patients using spironolactone which raised the question whether use of this medication might have other effects - such as increase the risk of breast cancer coming back in a patient who was previously diagnosed and treated for breast cancer. Breast cancer coming back is known as a recurrence and can be local recurrence (breast cancer coming back in the breast), regional recurrence (breast cancer coming back in the lymph nodes) or distant recurrence (breast cancer coming back in another part of the body such as the bone).
Preliminary Study Suggests Good Safety in First 2 Years
A new study by Wei and colleagues examined whether spironolactone increases the risk of recurrence within 2 years after a diagnosis of breast cancer. 746 breast cancer patients who had been prescribed spironolactone were matched to 746 breast cancer patients in a large database who had never used spironolactone
Breast cancer recurrence occurred in 16.5% of those who received spironolactone compared with 15.8% of those who did not receive spironolactone; the difference was deemed not statistically significant. The authors concluded that spironolactone was an option for treating hair loss in patients with breast cancer.
This study is valuable as it provides a start to understanding the use of these medications in women with breast cancer. I was surprised to see such a high rate of recurrence in this study (15 % at year 2). Most studies in the breast cancer literature do not have such high rates of recurrence by year 2. For example, stage 1 breast cancer is the most common type of breast cancer and only a very small proportion of women have recurrences by year 2 (well under 5 %).
More Studies Needed To Evaluate Safety in Years 2-20
More studies are needed especially longer studies that take us to five years (and beyond). Although recurrence risk is highest at 2 years (which was the cut off the authors of this study chose) well over 50 % of patients who are going to actually have a recurrence will have their recurrence beyond year two. For example, in some studies the median time is about 3 years meaning that one half of patients who are going to have a recurrence will have a recurrence after year 3 and one half will have a recurrence before year 3. We know the risk of recurrence is greatest in the first two years but most women are carefully followed for five years to evaluate for early recurrence. Five years is traditionally used in oncology as the benchmark not two years.
The chance of recurrence between years 2 and 5 is not insignificant and 20 % of recurrences occur between year 5 and 20. So longer term studies are absolutely needed. In addition, factors such as size of the tumor, pathology of the cancer, and the presence or absence of lymph node involvement all affect recurrence risk. Therefore detailed studies of high risk vs low risk patients is needed. We know that women with younger age, advanced stages, negative hormone receptor status, and poorly differentiated tumor cells experienced the greatest hazard for recurrence. Hopefully, larger and longer term studies will build on the important initial observations by these authors.
Reference
Wei C, et al. Published online May 21, 2020. J Am Acad Dermatol.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.