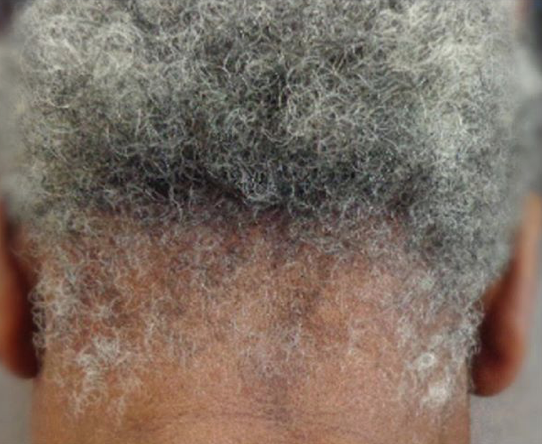
My hair was ripped off: Will it grow back?
Traumatic Hair Pulling: Full Regrowth May or May Not Occur
I am often asked if hair that is pulled out forcefully will regrow. Examples of this are the pulling of hair by children on the playground, hair getting caught in doors, machines etc or cases of hair pulling during assault or abuse-related situations (for example domestic abuse).
Without actually seeing the scalp, and knowing details of the patient's story, it is impossible to determine if hair will or will not grow back in any particular case. This requires an in person examination so that the scalp can be properly examined.
Hair regrowth is not a guarantee
There is no guarantee that hair regrowth will occur. One will know in 6-9 months if they will acheive full regrowth or not because that is how long it takes for hair to grow back following any type of injury.
It is certainly possible for repeated pulling to give permanent hair loss. However, in the vast majority of cases where hair is pulled from the scalp, hair grows back. If you or I were to reach up a pluck a hair, it will grow back. However, if pulling is repeated many times or is excessive with bleeding a greater chance exists for scarring to develop. Hair pulling that is accompanied by injury to the skin layers (i.e. that creates an actual wound) has a markedly increased chance of being associated with permanent scarring. It is such scarring that blocks the regrowth of hair. Scar tissue is permanent and, if present, generally destroys stems cells.
Anyone with concerns about incomplete growth after episodes of hair pulling should see a physician who specializes in hair loss for consideration of a scalp biopsy.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.