Vitamin D deficiency is common. Given that there may be some role between hair growth and vitamin D signaling inside cells, the current view is to ensure that vitamin D levels are adequate. This remains controversial from the perspective of hair loss because simply taking vitamin D tablets is not going to promote hair growth for most. Nevertheless, having low vitamin D levels could impair hair function, at least theoretically.
Vitamin D: The 30/75 Target Number
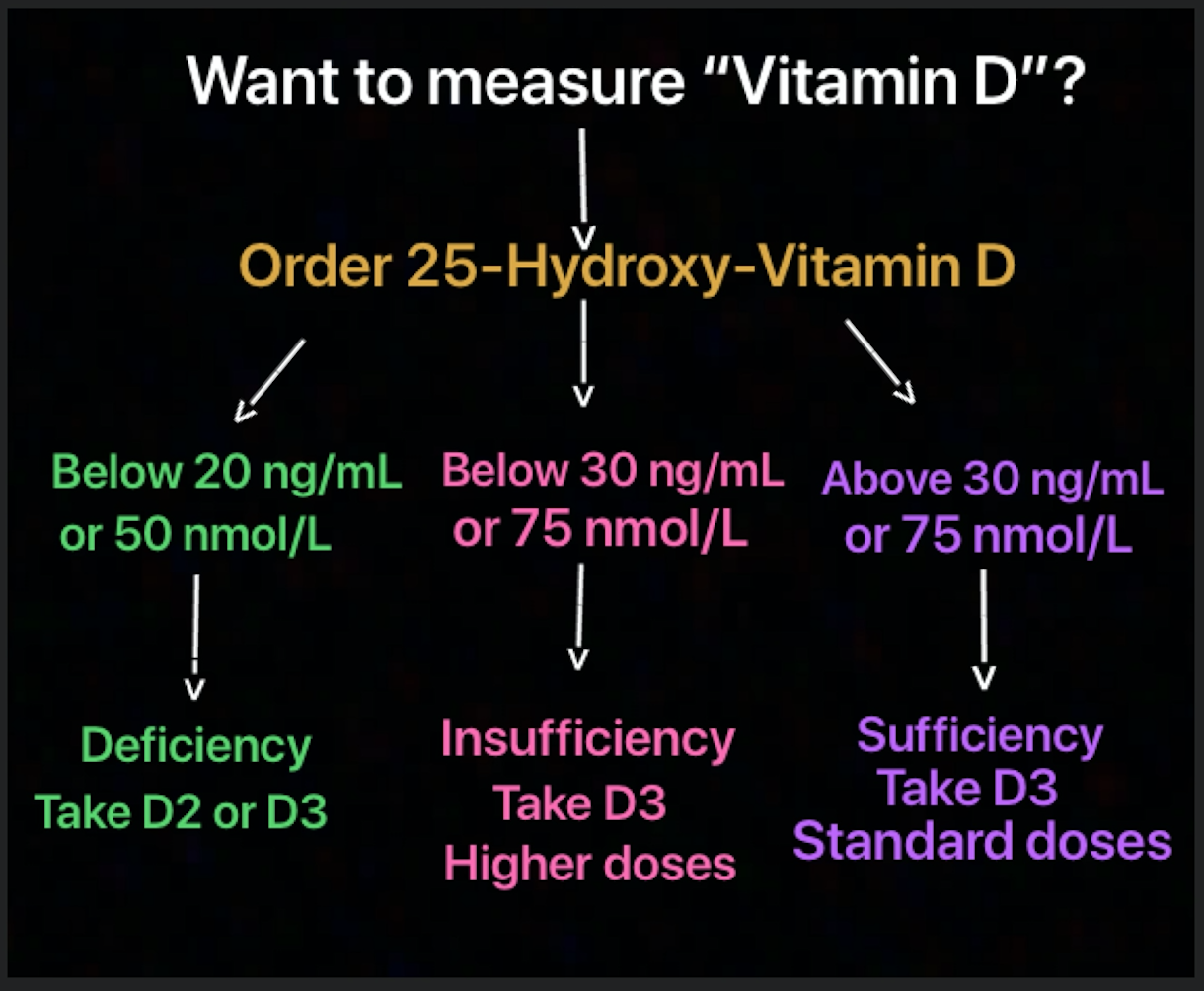
To monitor vitamin D levels, we don't actually measure vitamin D, we measure 25 hydroxy-vitamin D (sometimes simply referred to as 25 OH D). It's important to maintain 25 hydroxy-vitamin D levels above 30 ng/mL which translates to 75 mol/L. Some countries like the United States use ng/mL as their base measure and other countries (such as Canada) use mol/L. It's important to take note of these units. These numbers of 30/75 come from recommendations of the World Health Organization and others:
Vitamin D Deficiency is 25 OH D levels less than 20 ng/mL (50 nmol/L)
Vitamin D Insufficiency is 25 OH D levels less than 30 ng/mL (75 mol/L)
Vitamin D2 and Vitamin D3
To complicate matters slightly, there are two common forms of vitamin D supplements that can be taken. Vitamin D3, known as cholecalciferol, is the most common and available in doses of 400, 800, 1000, 2000 IU at most pharmacies and grocery stores. It is not typically available on prescription. High doses of vitamin D are available through use of vitamin D2, which is called ergocalciferol. It is the only form of vitamin D typically available by prescription. Vitamin D2 is available in 50,000 IU pills which makes higher dosing easier and for this reason it's the typical form using for individuals trying to correct vitamin D deficiency. In general, vitamin D3 (cholecalciferol) is thought to be more bioavailable than vitamin D2.
Vitamin D toxicity: A Healthy Respect
We need to respect all supplements since any supplement has the potential to be toxic. Large doses of vitamin D can cause calcium balance to go out of whack, leading to hyperalcemia. For vitamin D3, doses up to 10,000 IU daily are generally viewed to be quite safe for most individuals. For vitamin D2 mega-doses of 50,000 IU weekly (not daily), there is good safety when taken for short periods of time. studies have shown that individuals who mistakingly take vitamin D2 daily instead of weekly or monthly, can develop serious side effects. In other words, if anyone is going to take vitamin D, they need to know if they are taking vitamin D3 or vitamin D2 and focus on whether they are supposed to be taking it daily or weekly or monthly.
Individuals with chronic medical conditions, including osteoporosis, diabetes, kidney disease and women who are pregnant may need to follow other doses recommendations than listed here.
Correcting vitamin D deficiency: Are we taking enough?
There is a great deal of focus on the dose of vitamin D we should be taking. Depending on one's age and risk for various diseases, this may range from 400 IU daily to 2000 IU daily. But these numbers are generally for individuals who have normal levels and are trying to maintain them. The question then arises: What type of dosing is appropriate is someone is trying to simply get their levels up to a normal range?
There are a variety of different dosing schedules. For individuals with mild vitamin D insufficiency, I typically recommend 3000-4000 IU daily for a period of 6 months and retesting the 25 OH D levels down the road. For individuals who have more marked deficiency, I generally follow standard protocols, and prescribe vitamin D2 in many cases:
FOR SEVERE DEFICIENCY:
Vit D2 50,000 IU weekly for 12 weeks then once monthly for 3-5 months
FOR MODERATE DEFICIENCY
Vit D2 50,000 IU weekly for 4-8 weeks then once monthly for 2-4 months
In patients who don't respond adequately to the above regime, 50,000 IU of vitamin D2 used three times weekly for 6 weeks may be advised.
Studies have shown that for most people a total dose of 600,000 IU is needed over a 6 month period to help get vitamin D levels up high enough. For patients with vitamin D deficiency, I generally recommend retesting at the 6 month mark.
Conclusion
If one has vitamin D "deficiency" or "insufficiency", taking the standard vitamin D3 doses of 400 IU or 1000 IU that are available in pharmacies is not usually enough to correct the vitamin D deficiency. It's enough to keep levels normal once they are normal, but it's not enough to get levels up to a normal range. One needs slightly different doses for shorter periods of time to bring the vitamin D levels up.
REFERENCE
Pepper KJ et al. EVALUATION OF VITAMIN D REPLETION REGIMENS TO CORRECT VITAMIN D STATUS IN ADULTS. Endocr Pract. 2009; 15(2): 95–103.