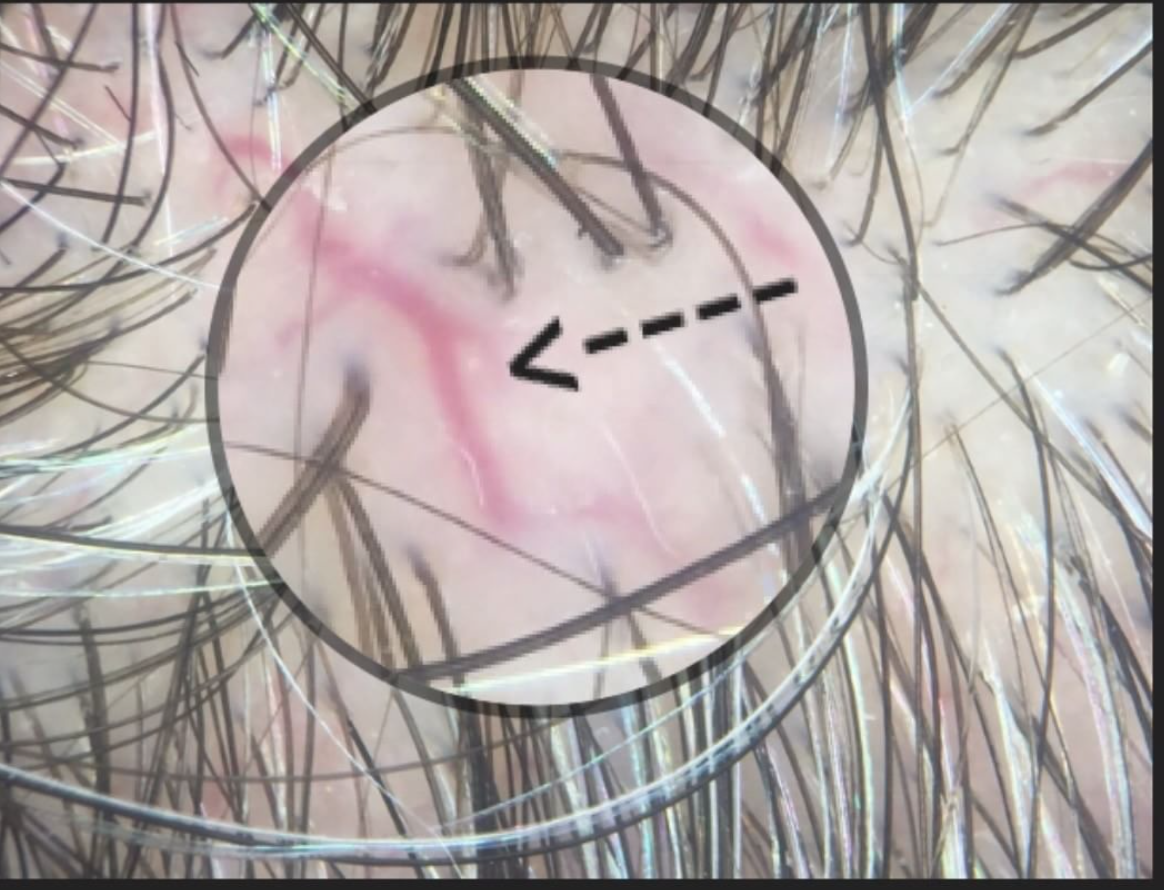
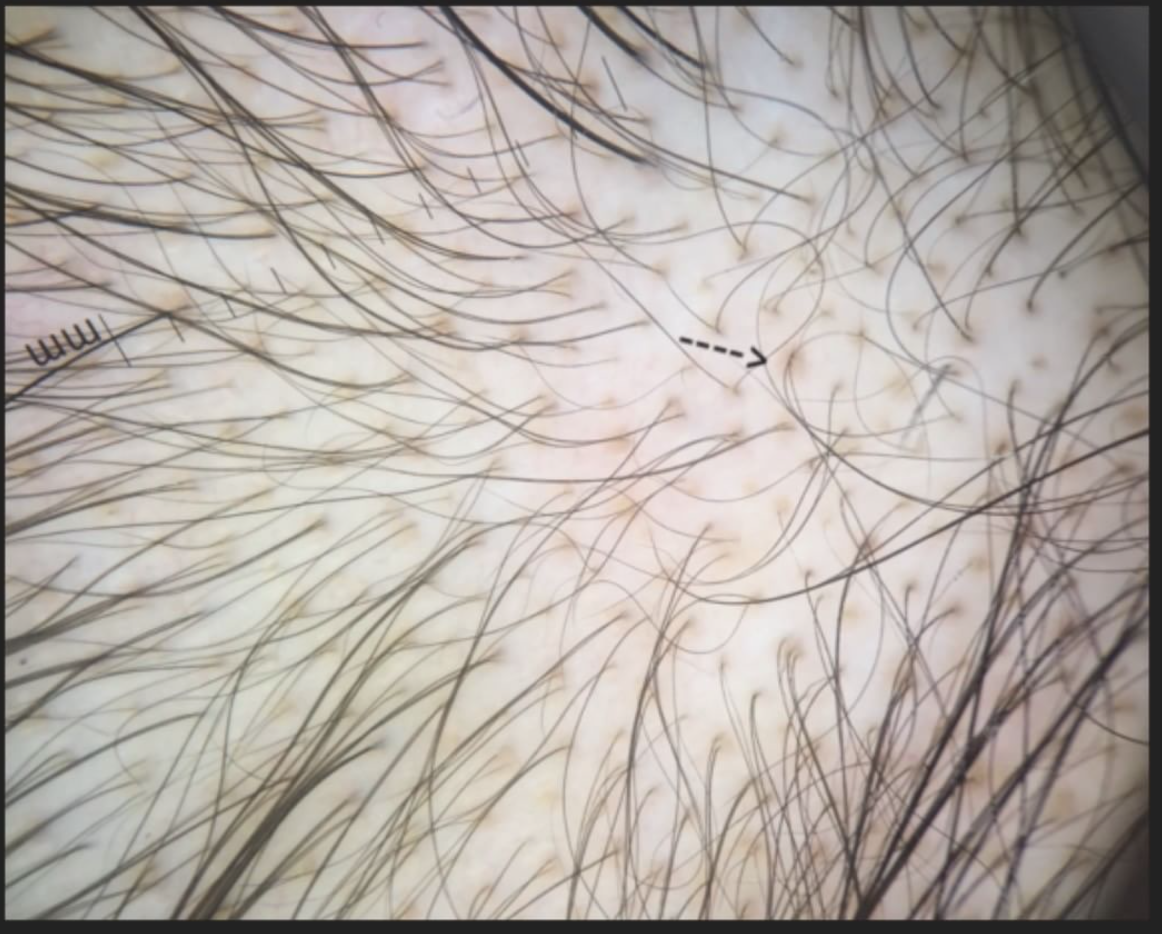
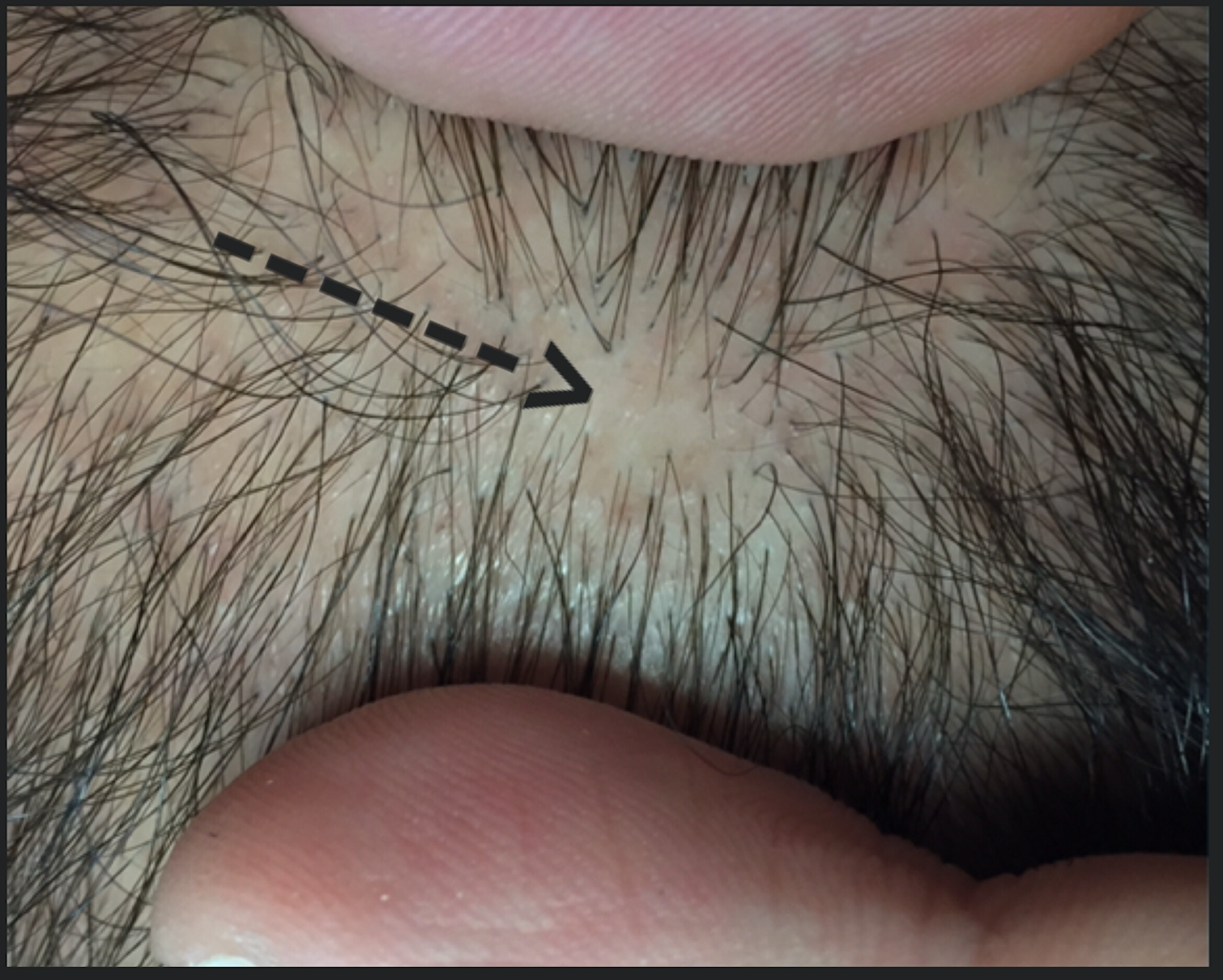
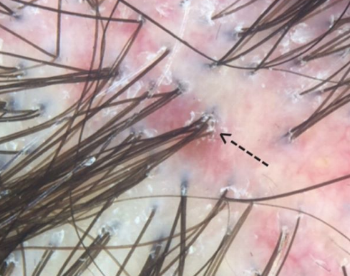
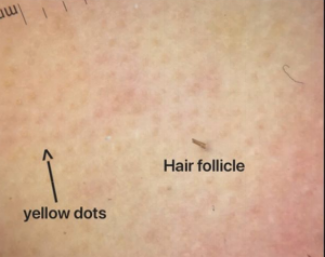
"Focal atrichia" (FA) refers to the absence of hairs is defined areas on the scalp. It is a feature generally seen in androgenetic alopecia whereby small circular areas totally devoid of hair are seen. These areas are typically the size of a pencil eraser and sometimes a bit bigger. Biopsies of these ares in the setting of androgenetic alopecia show accumulation of tiny vellus hairs.
It’s clear that FA is more common in androgenetic alopecia than other types of hair loss. A 2017 study by Olsen and colleagues showed FA was seen in 44 % of patients with FPHL compared to 2 % of other diseases. Those other 2 % may include area of primary scarring alopecia, scars from trauma, and even diffuse alopecia areata. Nevertheless, focal atrichia is most commonly seen in androgenetic alopecia.
There are still a few things that are unclear about whether one sees FA atrichia only in advanced disease. That same 2017 study by Olsen suggested 67 % of women with “late onset” FPHL had FA compared to just 15 % of those with “early onset” AGA. As we continue our discussion one must keep in mind that late onset generally has better prognosis.
Study 1: Olsen and colleagues, 2017
The 2017 Olsen study set out to evaluate the frequency of focal atrichia in various types of hair loss and its histologic characteristics in female androgenetic alopecia. The authors reviewed 250 consecutive female patients seen with hair loss for the presence or absence of FA. Interestingly, FA was identified in 46/104 (44%) of women with female pattern hair loss, including 15 % of early onset and 67% of late onset compared to 3/146 (2%) of those with other hair disorders. The histological (biopsy) findings of FA in FPHL showed mainly a more progressive miniaturization process than that of haired areas of the scalp. Taken together Olsen and her colleagues concluded that FA wasa clinical clue to the diagnosis of FPHL, particularly late onset subtype.
Study 2: Hu and colleagues, 2015
Studies by both Hu and colleagues and Zhang and colleagues both independently showed FA was associated with more severe disease. Additionally, Zhang et al showed that it was also associated with longer duration of disease. These findings seem to be at odds with the Olsen study.
Hu and colleagues performed a case-control observational study to identify the trichoscopic findings of AGA and to evaluate their relationship with the overall severity of the androgenetic aloepcia. The authors performed trichoscopic examination for 750 male AGA patients and 200 female (FPHL) patients, along with 100 male and 50 female normal controls. In this study, FA was positively related to severity of hair loss (P < 0.05).
Study 3: Hu and colleagues, 2012
Zhang and colleagues set out to analyze characteristics and investigate associations and clinical and trichoscopic features of female patients with FPHL. The did so by evaluating data from 60 patients with FPHL. FA was positively correlated with the stage and duration of hair loss.
Taken together, it is clear that FA is frequently seen in androgenetic alopecia. At first glance, is not uncommon to wonder whether these areas in fact represent scarring alopecia (i.e. tiny patches of Pseudopelade of Brocq or lichen planopilaris) or represent small areas of alopecia areata. However, when taken in context with the miniaturization going on in other areas of the scalp nearby, one can generally be confident these are area of FA.
The general consensus would be the FA is a negative prognostic factor.
Reference
Olsen et al. Focal Atrichia: A Diagnostic Clue in Female Pattern Hair Loss.
J Am Acad Dermatol. 2017.
Hu R, et al. Trichoscopic findings of androgenetic alopecia and their association with disease severity. J Dermatol. 2015.
Zhang X, et al. Female pattern hair loss: clinico-laboratory findings and trichoscopy depending on disease severity. Int J Trichology. 2012.