Shingles (Herpes zoster) Infections in Patients Who Use Hydroxychloroquine (Plaquenil)
Do Users of Hydroxychloroquine Have a Higher Change of Shingles?
I’ve selected this question below for this week’s question of the week. It allows us to review some concepts related to zoster infections in patients using hydroxychloroquine
Question
I am a 63 year old female and I use hydroxychloroquine (Plaquenil) for lichen planopilaris. I also have topical mometasone furoate steroid lotion and receive steroid injections at my doctor’s office every 2 months or so. I have developed shingles and I am specifically wondering if the patients who use hydoxychloroquine are at increased risk to develop shingles?
Hydroxychloroquine (Plaquenil) Increases the Risk of Shingles.
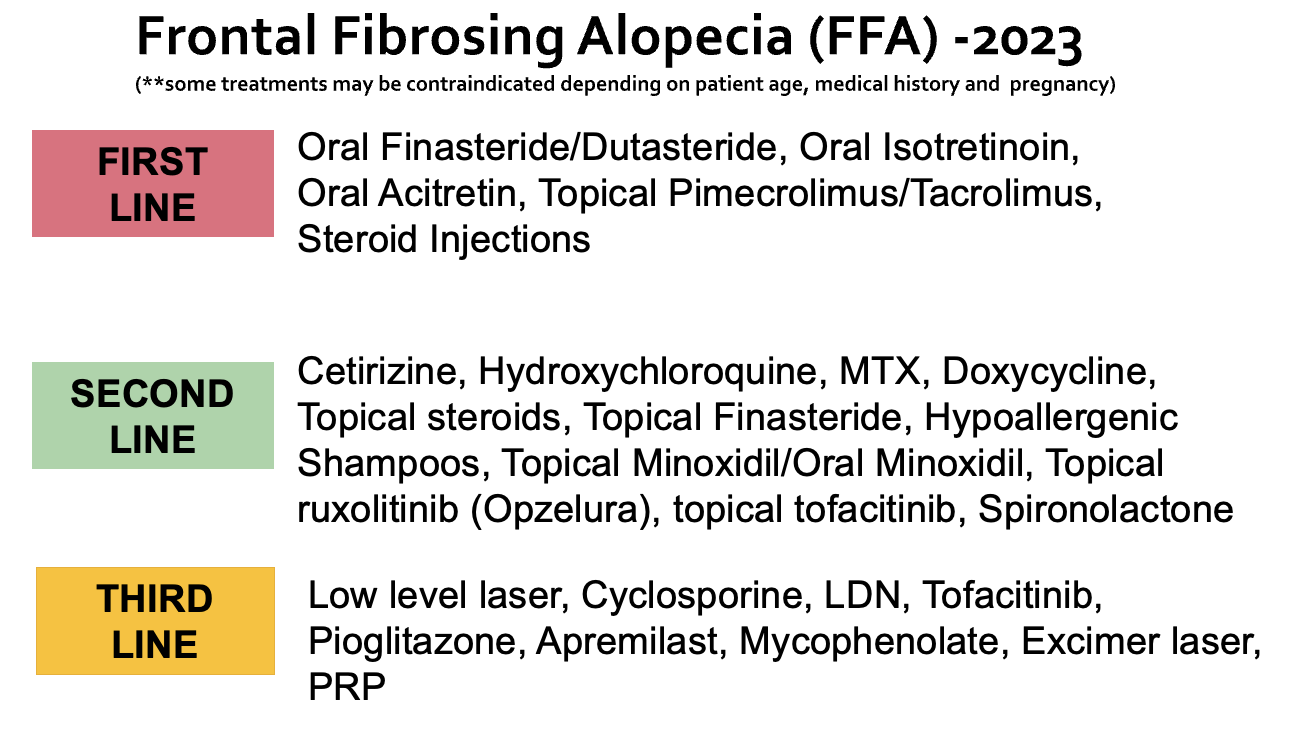
Hydroxychloroquine (Plaquenil) is an oral medication that is commonly used in the treatment of many types of autoimmune hair loss conditions. The list of hair loss conditions that we use hydroxychloroquine for includes lichen planopilairs, frontal fibrosing alopecia, discoid lupus and pseudopelade.
Some immunosuppressants are known to increase the risk of patients developing infections. Today, we’ll take a look at the risk of a specific infections known as shingles in patients who use hydroxychloroquine. Shingles is caused by the herpes zoster virus.
Hu SC et al, 2016
In 2016, Hu and colleagues set out to examine the risk of zoster infections in patients who use hydroxychloroquine. The researchers evaluated the risk of zoster (shingles) in patients with lupus (SLE) treated with different immunosuppressants. The authors found that hydroxychloroquine use did increase the risk of shingles. In fact, the risk was dependent on dose with patients using higher doses having slightly higher risk of shingles. Other medications associated with greater herpes zoster (shingles) risk in patients with SLE included oral corticosteroids, intravenous methylprednisolone, oral cyclophosphamide, intravenous cyclophosphamide, azathioprine, methotrexate, and mycophenolate mofetil.
Liao TL et al, 2017
In 2017, Liao and colleagues set out to determine the risk factors and outcomes of herpes zoster (shingles) among patients with RA. The researchers found that exposure to Plaquenil was associated with a two fold increased risk of developing shingles (aOR=1.95, 95% CI 1.39 to 2.73, p<0.001)). Other immunosuppressants were also associated with an increased risk including corticosteroids (≥10 mg/day adjusted OR (aOR)=2.30, 95% CI 1.25 to 4.22, p=0.01), anti-tumour necrosis factor biologicals (aOR=2.07, 95% CI 1.34 to 3.19, p=0.001) and conventional synthetic disease-modifying anti-rheumatic drugs (methotrexate (aOR=1.98, 95% CI 1.43 to 2.76, p<0.001). To read the paper yourself, simply click on the link below.
Zamora et al. 2020
In contrast to other studies, a 2020 study by Zamora and colleagues showed that certain patient groups may be less likely to develop zoster while on hydroxychloroquine. The purpose of this 2020 study was to identify clinical risk factors associated with developing herpes zoster (HZ) infections in patients with systemic lupus erythematosus (SLE). The authors performed a case control study of zoster infections in SLE patients. Cases were matched 1:2 to SLE controls without HZ infection for age, sex, and disease duration.
The study involved 65 SLE patients who developed zoster compared to 130 SEL patients who did not develop zoster. Prednisone, cyclophosphamide, and mycophenolate mofetil use increased the risk of developing zoster. Surprisingly, hydroxychlorqouine use reduce the risk of zoster by 87% (adjusted odds ratio 0.13, P = .003). The authors of this study felt that hydroxychloroquine use confers a protective role against developing zoster.
Qian J et al. 2021
A 2021 study by Qian and colleagues showed that patients who used hydroxychlroqouine had an increased risk of developing shingles. The risk of shingles was higher for hydroxychloroquine users than methotrexate users.
The authors’ study set out to evaluate the association between use of certain types of antiinflammatory medications (namely DMARD type drugs) and subsequent risk of herpes zoster. To do so, the authors used a heterogeneous and prospective population-based cohort study.
There were slightly over 250,000 participants in the study. There were 6295 new DMARD users and 17 024 incident herpes zoster events. Compared with non-users, the risk of zoster was higher in those who used biologic (b)DMARDs, either alone or in combination with conventional synthetic (cs)DMARDs than in those who only used csDMARDs (adjusted hazard ratio [aHR] 2.53 [95% CI: 2.03, 3.16]) for bDMARDs vs 1.48 [95% CI: 1.33, 1.66] for csDMARDs, P-heterogeneity < 0.001; reference: non-users). Among users of csDMARDs, compared with non-users, zoster risks were highest in those using exclusively cyclophosphamide (aHR 2.69 [95% CI: 1.89, 3.83]), more moderate in those using azathioprine (aHR 1.57 [95% CI: 1.07, 2.30]) and hydroxychloroquine (aHR 1.43 [95%CI: 1.11, 1.83]) and not elevated in users of methotrexate (aHR 1.24 [95% CI: 0.98, 1.57]), sulfasalazine (aHR 1.00 [95% CI: 0.71, 1.42]) and leflunomide (aHR 0.41 [95% CI: 0.06, 2.88]).
Conclusions: The risk of zoster was high among bDMARD and cyclophosphamide users. Also, the risk was increased in those using hydroxychloroquine alone and in combination with methotrexate but not methotrexate alone. Preventative strategies such as zoster vaccination or antiviral therapies should be considered in these populat
Mok CC et al 2023
A 2023 study published in the journal Clinical Rheumatology also showed that hydroxychloroquine is associated with an independent risk of zoster - at least in Rheumatology patients. In this study, 1,479 patients were studied (88.3% women, age 45.0 ± 15.8 years). Th commonest rheumatic diseases in this study were systemic lupus erythematosus (SLE) (38.7%) and rheumatoid arthritis (28.3%). The cumulative risk of having HZ reactivation after 2 years was 4.9 % and after 4 years it was 7.6%. Cox regression analysis revealed that a diagnosis of SLE, increasing age, higher NLR, use of cyclophosphamide, and increasing doses of prednisolone, azathioprine, hydroxychloroquine and leflunomide were independently associated with HZ infection.
Conclusion
Hydroxychloroquine (Plaquenil) appears to increase the risk of shingles in patients with Rheumatoid arthritis and patients with lupus. Whether it increases the risk in patients with scarring alopecia has not been studied but there is no reason to believe it should not. By virtue of affecting the risk of shingles, it would seem quite reasonable to classify hydroxychloroquine as a true immunosuppressant.
REFERENCE
Zamora LD et al. Risk factors for herpes zoster infection among Filipinos with systemic lupus erythematosus. Int J Rheum Dis. 2020 Feb;23(2):197-202
Liao TL, et al. Risk and severity of herpes zoster in patients with rheumatoid arthritis receiving different immunosuppressive medications: a case-control study in Asia. BMJ Open. 2017.
Hu SC, et al. Immunosuppressive medication use and risk of herpes zoster (HZ) in patients with systemic lupus erythematosus (SLE): A nationwide case-control study. J Am Acad Dermatol. 2016.
Mok CC et al. Prevalence and risk factors of herpes zoster infection in patients with rheumatic diseases not receiving biologic or targeted therapies. Clin Rheumatol. 2023 Apr;42(4):1019-1026.
Qian J et al. Use of disease-modifying antirheumatic drugs and the subsequent risk of herpes zoster in older adults. Rheumatology (Oxford). 2021 Nov 3;60(11):5042-5051.