Hair Systems vs Wigs for Scarring Alopecia: Which should I consider?
Is a hair system possible for someone with active scarring alopecia?
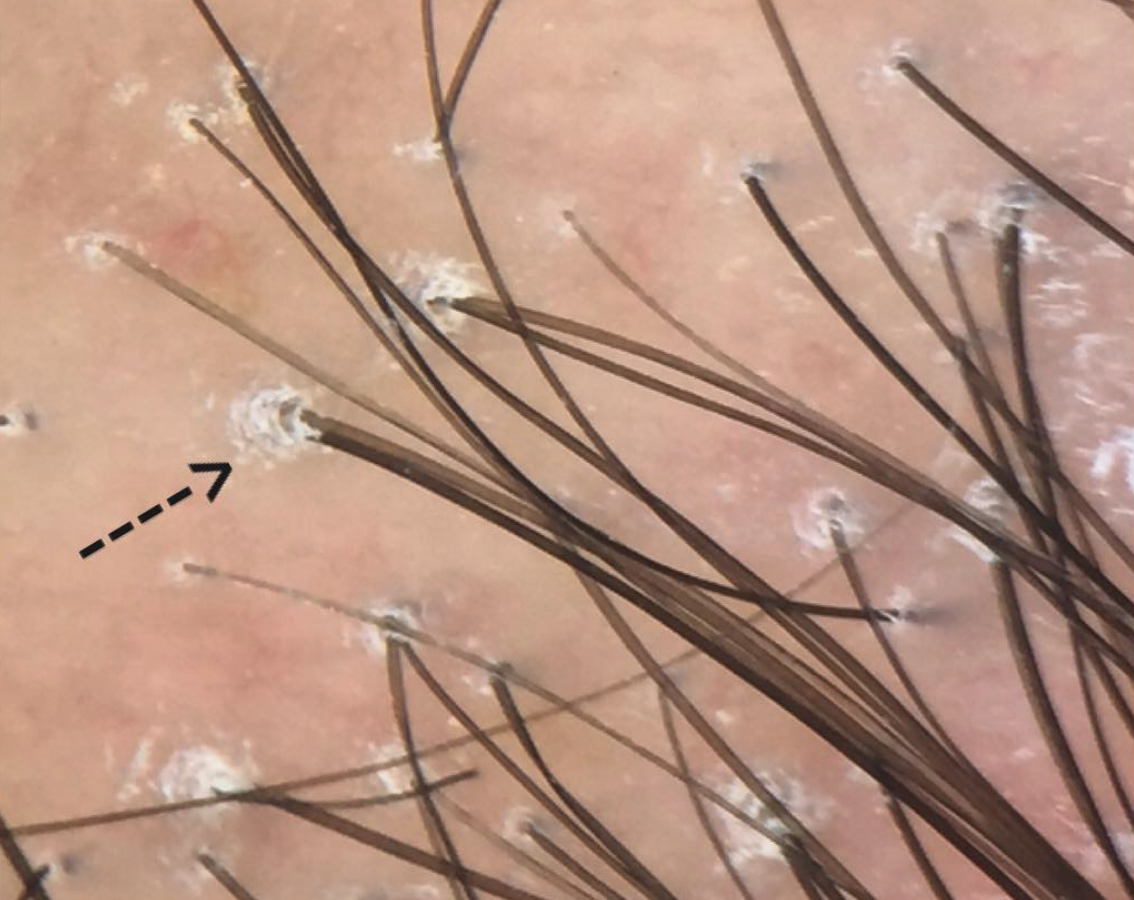
Scarring alopecia is a form of hair loss which can lead to permanent bald areas on the scalp. Treatments focus on helping to stop hair loss but do not improve hair in most. Some individuals elect to purchase a wig, hairpiece or hair system while receiving treatment. For the purposes of the discussion that follows, I will specifically use the term hair system to refer to a scalp camouflaging method whereby synthetic or human hair is attached to a layer of some sort and glued to the scalp with some type of adhesive. I will use the term wig or hairpiece to include a broad array of similar products that attach via clips, tape or elastic.
Two Key factors to consider
The are quite a few factors that go into deciding what type of wig, hairpiece or hair system is appropriate for someone with scarring alopecia. The two main factors to consider when I am meeting with a patient trying to decide what type of system they should purchase are the following:
(1) How active is the scarring alopecia right now?
(2) Does the patient need topical steroids, steroid injections or special shampoos as part of his or her ongoing management strategy?
(1) How active is the scarring alopecia right now?
If a patient has a very active scarring alopecia (with many symptoms and/or rapid hair loss), it will be important to consider choosing a hair piece or wig with clips or tape over a hair system that is attached to the scalp with adhesive. A patient with an active scarring alopecia needs to have the scalp examined often to determine if treatment is working and to modify the exact treatment. For some scarring alopecias like folliculitis decalvans it may be important in some cases to frequently shampoo the scalp with antibacterial agents. An easily removable wig or hairpiece is preferred.
As the scarring alopecia becomes "quieter" it may be possible to consider shifting to a hair system and more permanent types of adhesive-based attachments. I generally ask patients to coordinate removal of the hair system at their salon on the same day as their follow up appointment with me or if that is not possible to have good pictures taken at the salon in the day that their system is removed, washed and reapplied (generally referred to as a "servicing).
(2) Does the patient need topical steroids, steroid injections or special shampoos as part of his or her ongoing management strategy?
For patients who answer yes to the above question, a wig or hairpiece will be preferred over a hair system. Topical steroids and steroid injections can be the mainstay of treatment for many patients with scarring alopecia. Even in relatively quiet scarring alopecias, topical steroids may still be needed every few days. For very active scarring alopecias, steroid injections may be needed monthly. As mentioned above under point (1), for some scarring alopecias like folliculitis decalvans it may be important in some cases to frequently shampoo the scalp with antibacterial agent. Therefore, in such cases where there is active disease, a more permanent hair system becomes either impractical or inconvenient. It needs to be removed for these treatments to be properly administered and this is not easy if a hair system is glued to the scalp.
Conclusion
All in all, these are the discussions that patients will want to have with their dermatologist. If topical steroids are needed daily and steroid injections are needed monthly for example (for very active disease) use of a hair system with an adhesive is less preferred over wigs or hairpieces with clip attachments or tape. If possible, these are discussions the dermatologist might have with the wig salon itself to best coordinate the proper care of the patient .
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.