Topical Tofacitinib for Alopecia Areata: How much does it really help?
2% Ointment Helped 1 of 10 Patients
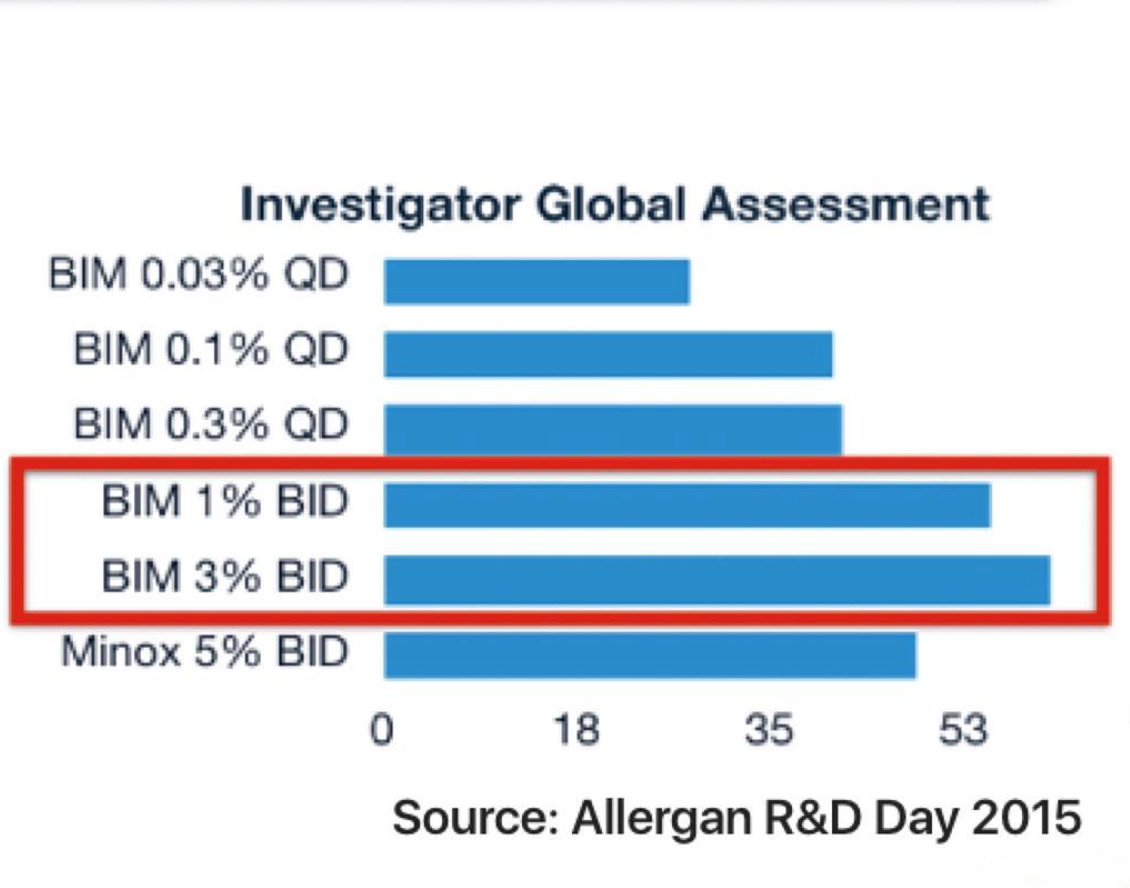
Oral tofacifitinb belongs to a group of medications known as JAK inhibitors and represents an off-label treatment for alopecia areata. Its use is limited by cost but also by potential side effects associated with its immunosuppressive effects. An increasing interest is mounting regarding the potential use of topical JAK inhibitors in treating alopecia areata.
The optimal formulation (liposomal vs ointment) has yet to be definitively proven. Previous studies have suggested a benefit of both topical ruxolitinib and topical tofacitinib in at least some patients with alopecia areata.
New Study Examines Topical Tofacitinib
Researchers from Yale set out to examine the benefit of tofacitinib ointment in adults with alopecia areata. In their report, the authors described the results of a 24-week, open-label, single-center pilot study of 10 patients with AA treated with tofacitinib 2% ointment applied twice daily. Patents were eligible for the study if they were 18-years-old or older, had at least 2 patches of alopecia areata, had stable or worsening disease for 6 months, and have received no treatment for AA for at least 1 month prior enrolment. Tofacitinib was applied to half of the involved scalp and, if and when evidence of hair regrowth was observed, tofacitinib was subsequently applied to the entire involved scalp.
What were the results?
The authors showed that 3 of 10 subjects experienced hair regrowth with topical tofacitinib with a mean decrease of 34.6% in SALT score (standard deviation 23.2%). Of these three patients, only one had excellent regrowth. 2 others had partial growth. Skin irritation was reported by 40 % of patient and folliculitis in 10 %. Both of theses side effects resolved even without treatment. 40 % of patients had a minor increase in cholesterol levels. Despite these minor side effects there were no serious side effects.
Conclusion and Summary
This is an interesting study by these Yale researchers who are leaders in this area of JAK inhibitors. It was disappointing that only 1 of 10 patients had significant improvement. Whether a differential topical vehicle (such as a liposomal vehicle) could have different results awaits further study. The main message of all of the topical JAK inhibitors studies to date is that they could help some patients with alopecia areata, but for many they do not.
REFERENCE
1. Liu L et al. Tofacitinib 2% ointment, a topical janus kinase inhibitor, for the treatment of alopecia areata: a pilot study of 10 patients. Journal of the American Academy of Dermatology.
DOI: http://dx.doi.org/10.1016/j.jaad.2017.10.043
2. Topical Ruxolitinib Promotes Eyebrow Regrowth in Alopecia Universalis
3. Topical JAK inhibitors for Children and Adolescents with AA
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.