Do we need to be concerned about melanoma when using Bimatoprost (Latisse, Lumigan)?
I was recently asked a very interesting question - and that is whether one needs to exercise caution when using prostaglandin analogues like bimatoprost (Latisse) or latanoprost (Xalatan) in patients with a history of melanoma. The short answer is that there is no good evidence to support an increased risk of melanoma in users of any of the prostaglandin analogues - which includes latanoprost (Xalatan) and bimatoporst (Latisse). However, a number of points are important to carefully consider here - especially for individuals who already have a history of this type of cancer.
In general, patients with a personal or family history of melanoma (especially eye melanomas or skin melanomas around the eye) should speak with their physician if prostaglandin analogue type drugs are to be prescribed. This includes latanoprost (Xalatan) and bimatorpost (Lumigan, Lattise).
1. Prostaglandin analogues increase pigmentation.
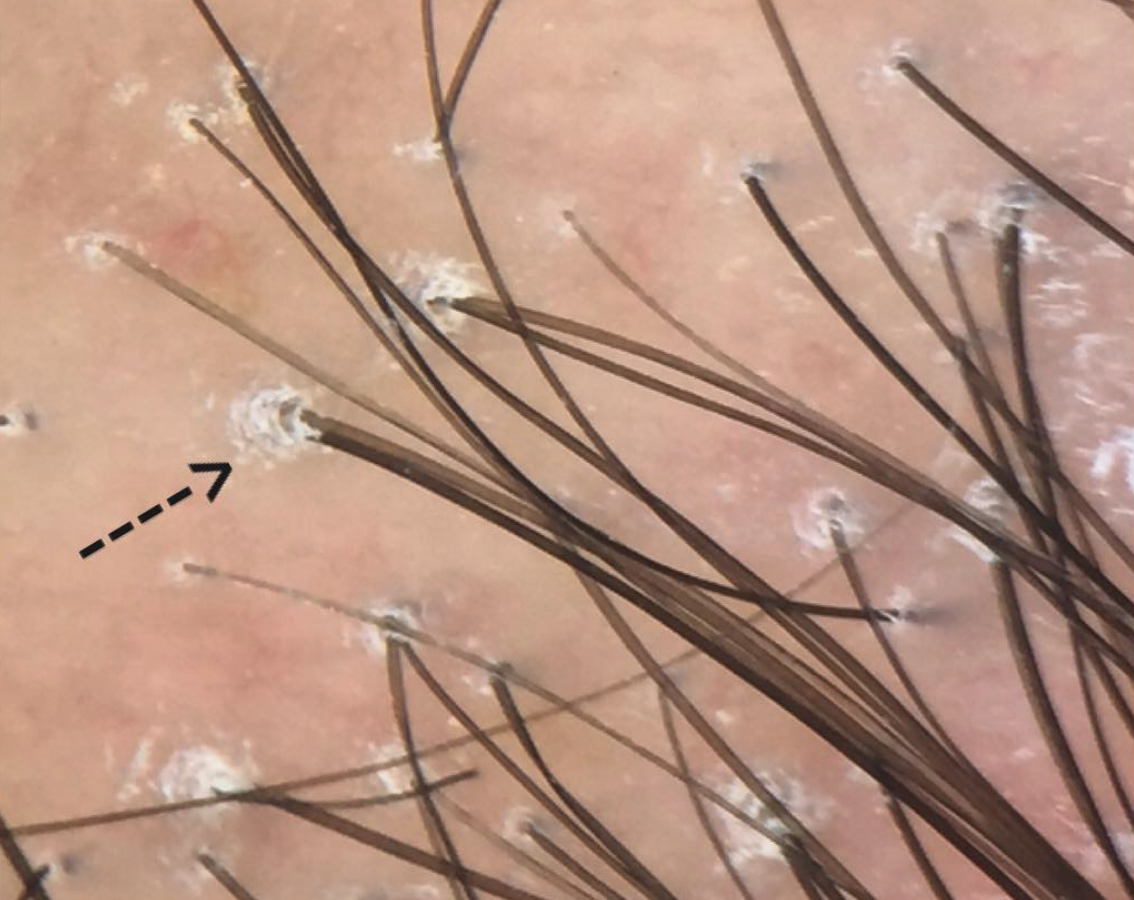
It is well known that users of prostaglandin analogues can develop increased pigmentation. For example, users of Bimatoprost (Latisse), can sometimes develop pigmentation of the eyelid or skin around the eyelid. Bimatoprost is a drug that stimulates prostaglandin F2 alpha (PGF2a). There is a good scientific basis for the observation that PGF2a drugs can cause pigmentation. In 2005, a study by Scott and colleagues (see reference below) showed that PGF2-alpha stimulates the activity and expression of tyrosinase, the rate-limiting enzyme in melanin synthesis. The group showed that fluprostenol, a potent and specific analog of PGF2a, stimulates tyrosinase activity in normal human melanocytes, but does not affect melanocyte proliferation. They also showed that melanocytes produce PGF2a in response to UVR.
2. There is no solid evidence of eye melanoma with prostaglandin eye drops
Given that the prostaglandin F2 alpha drugs can stimulate melanocyte pigmentation, health authorities have asked manufacturers of these drugs to submit data and monitor if there is any increased risk of eye melanoma (ocular melanoma) in users of these drugs. In studies and discussions in 2002 examining whether latanoprost (Xalatan) increased the risk of ocular melanoma , the conclusion was that it did not.
READ DISCUSSION
3. There have been cases reports of melanoma associated temporally with use of latanoprost and bimatoprost
Latanoporst (Xalatan) and bimatoprost (Latisse, Lumigan) are both drugs that target the prostaglandin F2 pathway. Latanoprost and Bimatoprost are widely prescribed as "first-line" agents for glaucoma.
In 2009, Esteve and colleagues reported 1 case of eyelid melanoma associated with the use of latanoprost. Two group reported two other cases of choroidal melanoma and earlobe melanoma that was associated with the use of latanoprost.
In 2012, Sun and colleagues reported a 77 year old patient who developed eyelid melanoma. She had used bimatoprost (Lumigan) for 6 years prior. When she first presented to her physicians, the pigmented lesion she had on her lower eyelid was biopsied and felt to benign. However, it subsequently progressed to a superficial spending melanoma in situ.
4. To date, there is no good evidence PGF2a affects negatively affects the biology of melanoma cells
Melanocytes express receptors for prostaglandins, including PGF2-alpha and PGE2 as well. PGF2-alpha binds to the FP receptor to activates signals in melanocytes. PGF2-alpha stimulates melanocyte dendricity. As mentioned above, PGF2α stimulates the activation of tyrosinase (the rate limiting step in melanin synthesis), and the formation of dendrites, which facilitate the transfer of melanosomes from melanocytes to keratinocytes
One study suggested that melanomas reduce their expression of the PGF2-alpha receptor (FP receptor) suggesting that the FP receptor is lost at the transcriptional level in melanoma and in nevi and melanoma in vivo. it appears the FP receptor is expressed only by melanocytes, but is lost in melanoma and in nevi. There remains some uncertainty as to whether melanomas increase their expression of PGF2 alpha on account of loss of the FP receptor.
Conclusion
To date, there is no good evidence to suggest that users of prostaglandin analogues like latanoporst (Xalatan) or bitmatoprost (Latisse) are at increased risk of skin or eye melanomas. However, individuals who are already diagnosed with melanoma of the eye or skin around the eye or face should speak to their physicians as the use of the drugs would need to be considered on a case by base basis. There are no guidelines for using these drugs if a patient already has a diagnose of melanoma and current prescribing guidelines do not offer it as a contraindication. Although previous case reports do not prove any cause, these findings simply prompt one to take pause and carefully consider the risks and benefits based on current scientific evidence.
REFERENCE
1. Fricke A, et al. The PGF(2alpha) receptor FP is lost in nevi and melanoma. Pigment Cell Melanoma Res. 2010.
2 Scott et al. Effects of PGF2a on human melanocytes and regulation of the FP receptor by ultraviolet radiation. Exp Cell Res 2005.
3. Esteve E et al. Melanoma during latanoprost therapy: three cases. Ann Dermal Venereol 2009; 136: 60–1.
4. Sun LL, et al. Lower eyelid melanoma during bimatoprost (Lumigan) therapy. Clin Exp Ophthalmol. 2012.