What is causing my beard, body and scalp hair loss?
What’s causing my beard hair loss?
I’ve selected this question below for this week’s question of the week. It allows us to discuss the importance of the speed of hair loss in the diagnosis of hair loss.
Here is the question….
QUESTION
I have diffuse thinning across my entire body. I am male, under 30. The hair loss initially started as rapid thinning on the entire scalp, soon spread across facial hair and body hair. Some distinguishable features of my hair loss are that my beard and body hair only have one hair per follicle, a lot of hairs remain as very short stubble and do not grow, eyebrows experience pain during periods of shedding. I've been to 4 dermatologists and had one scalp biopsy which was inconclusive. Hair loss has been very rapid, from initial onset I lost well over 50% of my hair density within 4 months. My beard presented with patches of hair loss which have grown in.
Beard photos, before (left) and right (after) hair loss
Scalp does not itch and I do not feel any burning. However I feel tenderness and itching in my eyebrows which are constantly shedding. I've been on finasteride ( discontinued ), oral minoxidil for 9 weeks, and steroid injections in the eyebrows which have helped with regrowth. Hair loss started 3 months after I experienced a very traumatic event and has continued well over 1 year now.. After the traumatic event I broke out with very severe cystic acne across my back, scalp neck and face and hair loss soon followed. The way I look today is completely indistinguishable from what I looked like 1 year ago.
What is the likely cause ?
ANSWER
Thanks for submitting your question. There are several possible hair loss conditions that could be causing this, but the most likely cause, by far, is alopecia areata. But it’s certainly not 100%.
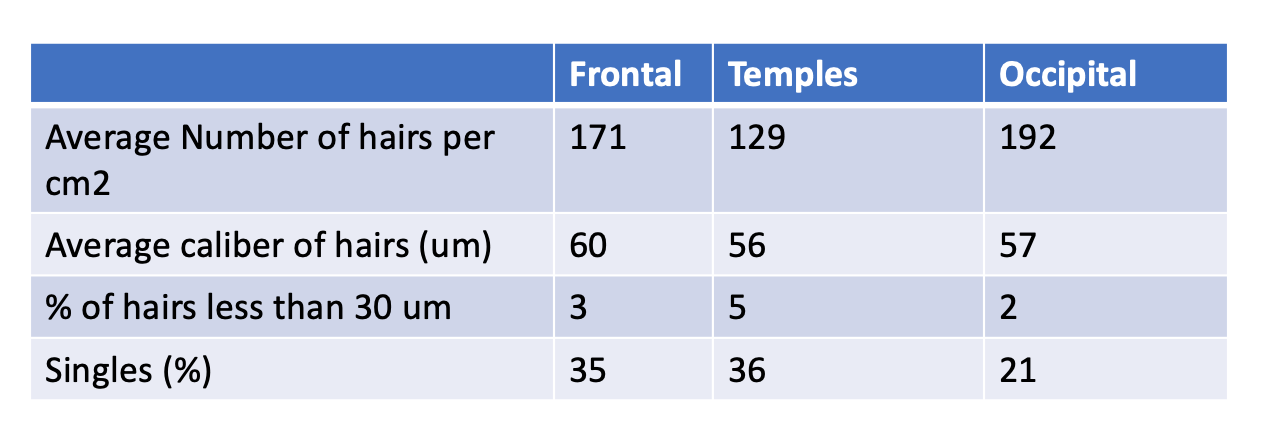
To help definitively figure out what’s going on, I would need to (1) ideally see photos of the scalp and eyebrows, (2) know the answers to a lot more questions I have, (3) review your biopsy and (4) review all your blood tests. I’d like to know if you’ve had patches of alopecia areata in the past, whether you have a family history of alopecia areata, how thin the eyebrows were, whether their was redness in the eyebrows too, whether the eyelashes were lost, whether you’ve had changes in your nails, weight loss, or abnormalities in your blood tests. I’d want to know if you’ve started or stopped any prescription medications and supplements in the last 12-16 months, started or stopped any anabolic steroids, and whether you’ve had any skin rashes of any sort in the last 2 years. Fevers, night sweats are important to know about as well. Of course, your entire medical history will be important.
The full list of possibilities for the hair loss includes:
Alopecia areata alone
Alopecia areata with a telogen effluvium
Alopecia areata with seborrheic dermatitis
Alopecia area with a telogen effluvium with seborrheic dermatitis
Alopecia Areata with a telogen effluvium with seborrheic dermatitis with male balding of the scalp.
Telogen effluvium with seborrheic dermatitis
Frontal fibrosing alopecia/lichen planopilaris
Rare mimickers - syphilis, cutaneous T cell lymphoma
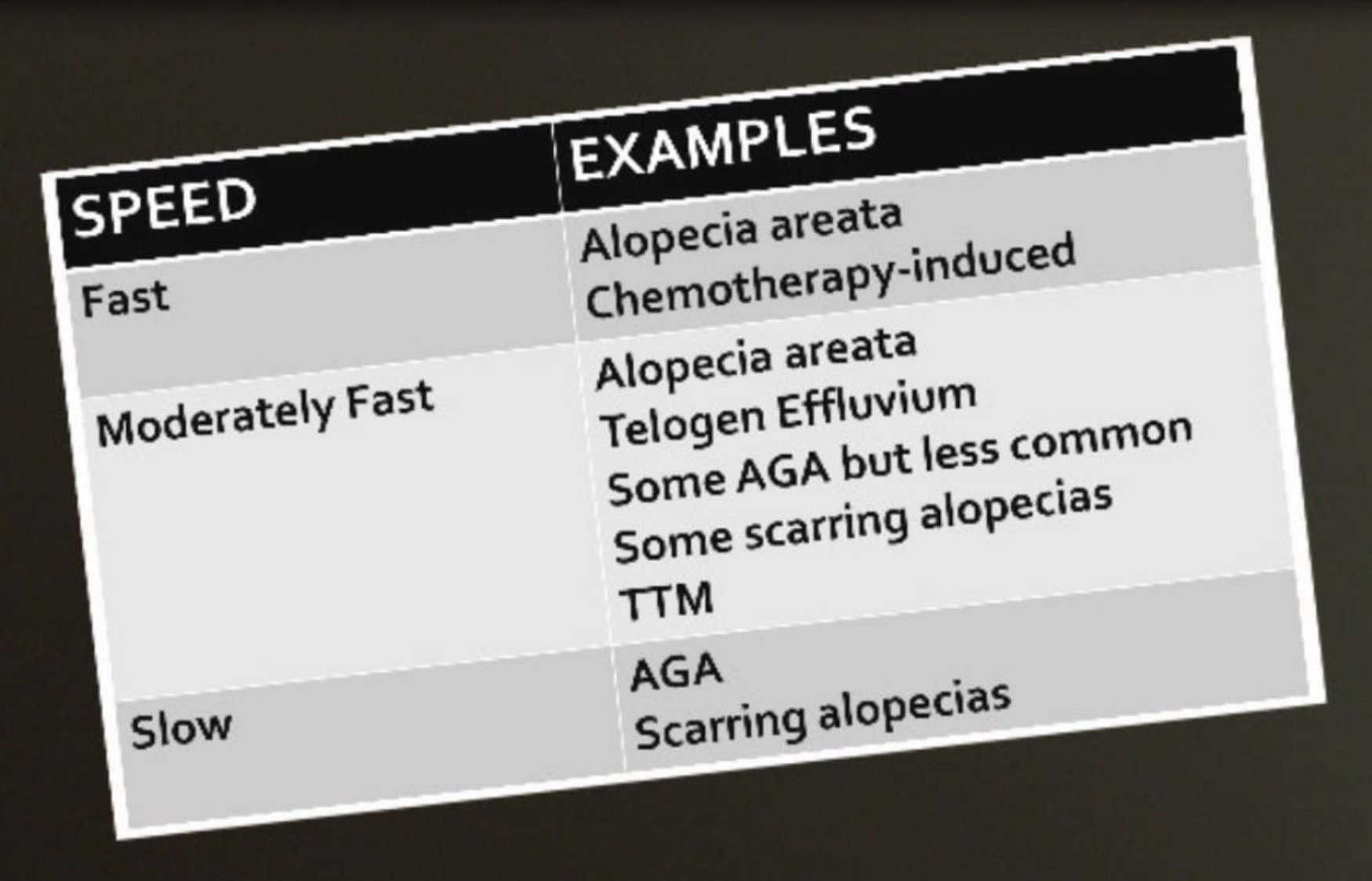
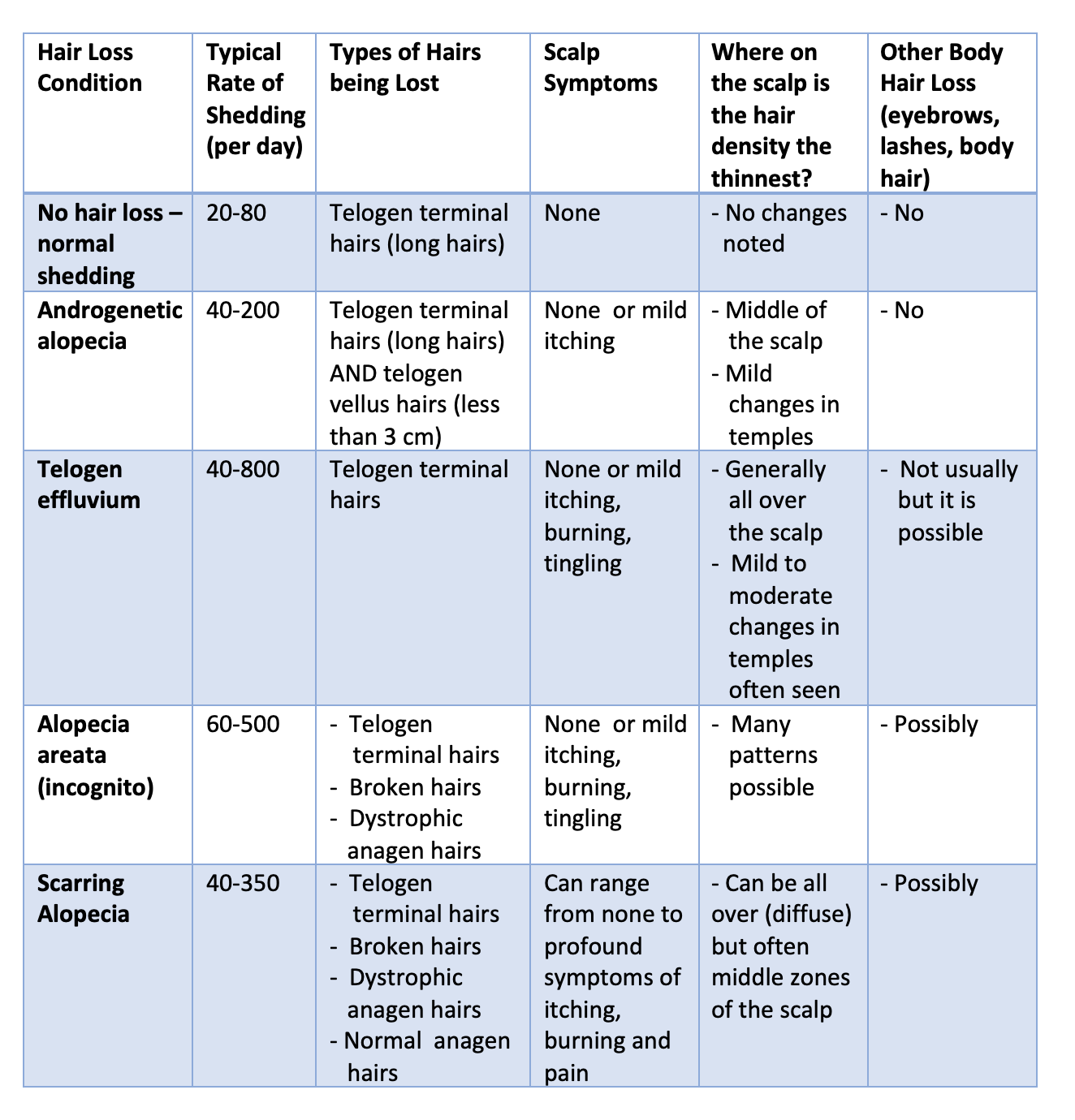
There are many features of the story here which fit well with alopecia areata. First, the speed of hair loss is fast. The loss of 50 % density in 4 months is seen in alopecia areata and sometimes telogen effluvium but this kind of rapid hair loss is more typical of alopecia areata. it’s far too fast for androgenetic alopecia but of course this may be a part of the hair loss that is happening as well (more chronically). It’s too fast for most scarring alopecias too (and I would not expect regrowth to occur in the manner you described if this were the case). It’s not impossible for FFA, but it is an uncommon story for FFA.
I’ve written about the importance of the speed of hair loss in the past. Alopecia areata is classically quite fast and has the potential to cause more rapid hair loss than telogen effluvium if the alopecia areata is active.
It’s possible of course, that a person has a telogen effluvium and alopecia areata too. A person can have two diagnoses or three or even four or five. The intense stress you had from the traumatic event can cause a telogen effluvium and if you are genetically predisposed, it could precipitate alopecia areata too.
The regrowth of your eyebrows with steroid injections is best in keeping with alopecia areata. I would need more information to know it it’s a little or a lot of regrowth. It would be helpful to know what the brows actually looked like before. If the regrowth has been really significant with the steroid injections, alopecia areata remains at the top of the list. That said, any inflammatory condition of the eyebrows can cause hair loss and steroid injections can help with regrowth. Seborrheic dermatitis of the eyebrow can cause a little bit of loss but it’s usually mild and steroid injections can settle down the redness and help get brows regrowing. Even frontal fibrosing alopecia can show some regrowth so the simple fact there was regrowth does not prove it is AA. Eyebrows can improve with steroid injections in quite a few conditions so this feature alone does not prove it’s alopecia areata.
The beard photos you’ve submitted are most in keeping with a diagnosis of alopecia areata. Are there mimicking conditions that can look 100% the same ? Yes, there certainly are. Rarely, a seborrheic dermatitis can cause beard loss but that’s quite unusual to be patchy in this manner. Rarely, an immune based issue can cause beard loss too (lichen planopilaris/frontal fibrosing alopecia) but regrowth is less likely in these types of situations. Frontal fibrosing alopecia really is one of the key conditions that you and your doctors need to rule out confidently. Beard hair loss or beard thinning happens in about 30-40 % of patients with FFA. Telogen effluvium affecting the beard in a patchy manner like shown in the photos is not typical so telogen effluvium would not explain the beard loss but could, of course, still be involved. Syphilis is not common cause of the hair loss pattern you are describing but this diagnosis needs to be considered by your doctors in a presentation like this. It is a great mimicker of alopecia areata. A rare condition of the blood cells (mycosis fungoides/cutaneous T cell lymphoma) needs to be considered if things don’t improve. I would not expect these latter two conditions to have spontaneous improvement you have described without treatment so they probably don’t fit well in your particular case. Alopecia areata is still at the top of the list of causes but your dermatologists can review these entities and perform a full skin examination.
The acne eruption you describe may or may not be related to the hair loss. I suspect it is related in some manner. Acne eruptions of this kind can be seen in alopecia areata. (See previous article alopecia areata and acne). In order to understand how hair could have a role in acne development, it is important to understand the function of hair. During the process of normal skin turnover, the shed skin cells from the hair follicle epithelium are carried upward in the follicular canal towards the skin surface. It is thought that the sebum that is secreted by the sebaceous glands helps in this process but helping the shed cells efficiency move out of the hair follicle canal.
Ringrose and colleagues first reported the relationship between acne and alopecia areata back in 1952. They described a male patient who developed acne, milia and cystic type eruptions only in the areas of alopecia. The authors proposed that the hair helps keep the follicular orfice open to allow sebaceous contents to be properly removed. They described the hair follicle as a “natural drain” to the removal of sebum.
These same authors performed some interesting histological studies by examining biopsies of these acne lesions. They found that acne lesions were not seen in areas that contained hair and were not seen in areas where the pilosebaceous unit was completely degenerated. The proposal here was the acne lesions of alopecia areata represented a transition period - between normal growth patterns and complete loss.
in 2007, Sergeant and colleagues proposed that the hair follicle acts as a type of ‘wick’ and acts to draw sebum up towards the skin surface. They stated that the hairs on the scalp may do this more efficiently that hairs on the face and therefore the hairs on the face may be predisposed to the formation of “micocomedones” and the typical lesions of acne. Microcomedones are a prerequisite for the ultimate acne lesion.
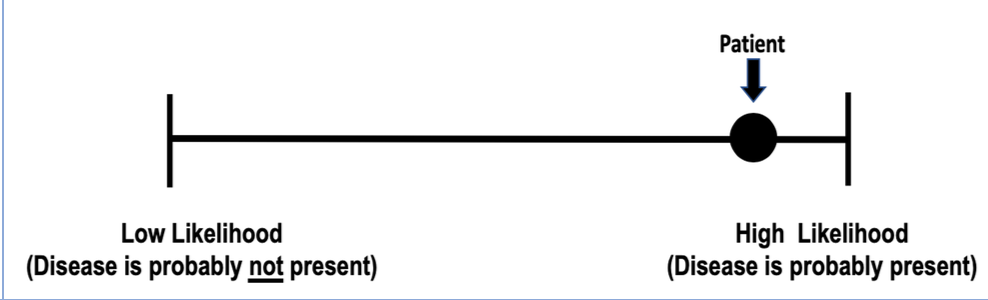
So in your case, there is a high likelihood a diagnosis of alopecia areata is present. It is certainly not 100 % but the likelihood is quite high. It will be really helpful to follow all hair bearing areas - as definitive signs of alopecia areata (or scarring alopecia or another condition) may show up over time. In my opinion, frontal fibrosing alopecia is the mimicker that really needs to be ruled out.
FINAL COMMENTS
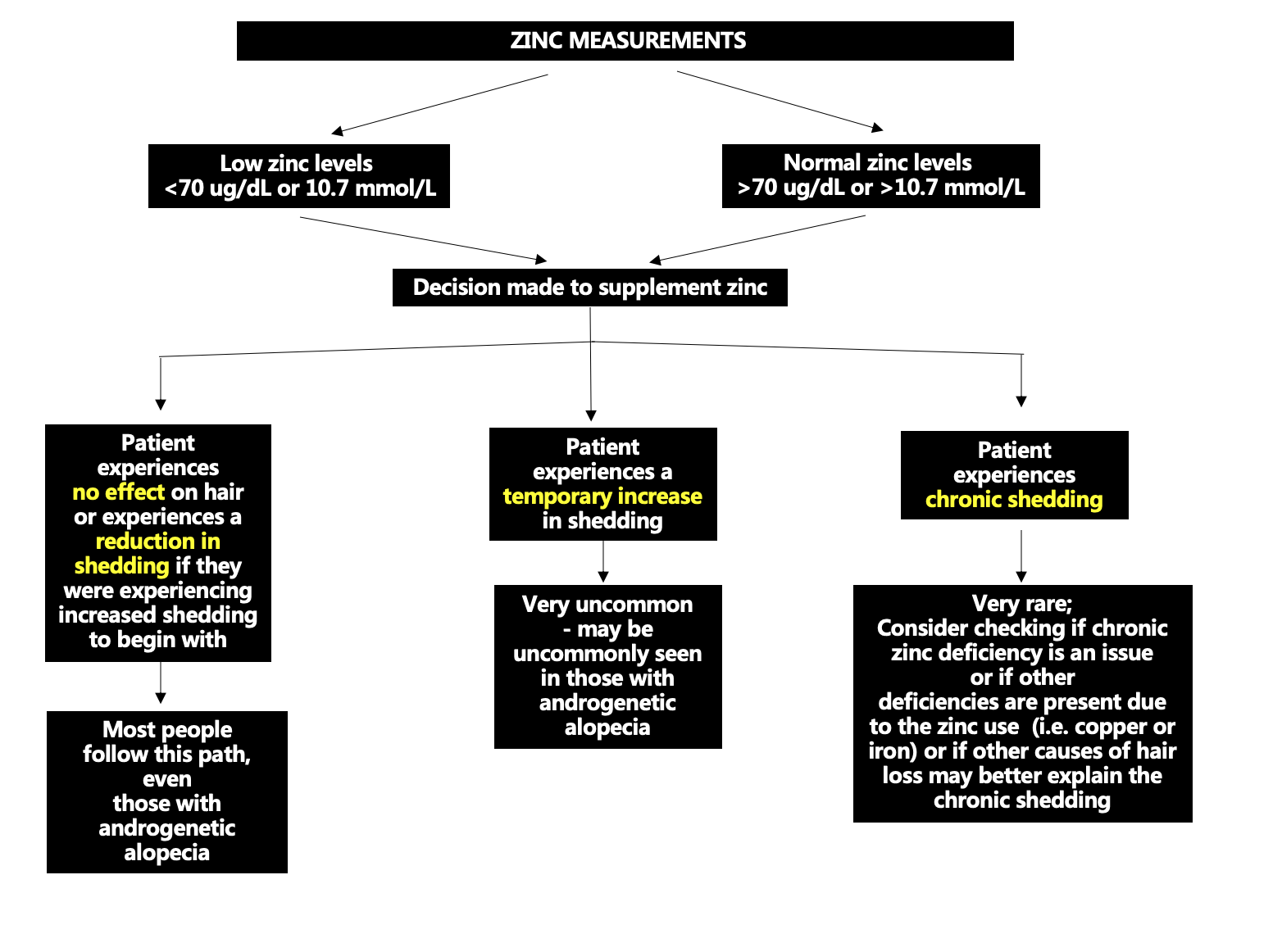
At this point, the evidence would suggest alopecia areata but I would need more information to confirm or refute that. I would recommend that you speak to your doctors about these issues as they will know your case best. I would suggest you considering asking them about blood tests for CBC, TSH, ferritin, testosterone, B12, ESR, ANA, zinc, vitamin D, RPR, creatinine, AST, ALT, urinalysis if you have not already. if any of these are missing you might get them done. If the diagnosis is not clear, a repeat scalp biopsy can be considered. It may be that with trichoscopy a dermatologist can evaluate whether alopecia areata is present although I certainly do appreciate that your story is complex and you’ve probably had many evaluations (with trichoscopy too). Biopsies of the arm hair, leg hair and eyebrows are trickier and often given less information. If a repeat biopsy is needed, it should come from the scalp. The main thing we are trying to distuish in the biopsy is alopecia areata vs scarring alopecia (ie frontal fibrosing alopecia) .
If it is alopecia areata that you have, I suspect that over time, a patch of typical alopecia areata hair loss will occur that will allow your doctor to definitively tell you if that’s what it is. There are ways to explore the diagnostic possibilities further. Certainly, the blood tests above are important. You’ll want to make sure there are no systemic issues that increase the chances for cystic acne and hair loss. We’ve spoken about the possibility of having a repeat biopsy. This should be done on the scalp and be 4 mm and be done with horizontal sections and read by an expert dermatopathologist. Alopecia areata can be tricky to diagnose in some cases. However, an increased proportion of catagen and telogen hairs and eosinophils in the tracts and peribulbar inflammation can all point to the diagnosis. A biopsy will pick up immune based issues, lymphomas, and if the percent of telogen hairs is high the biopsies will give an idea of how high it really is.
Sometimes in a situation like this, we consider a "therapeutic challenge.” A therapeutic challenge means we give certain medications to observe what happens when those medications are given. If the response to the medications is exactly what we predicted, it suggests we are probably correct with our diagnosis. I would need to know more about your story to describe exactly what might be appropriate but you and your doctor could consider therapeutic challenges like steroid injections to the entire scalp, or a 4-6 week course of oral steroids is an approach therapeutic challenge if alopecia areata is considered. If you get significant regrowth during these types of therapies, it’s a pretty good indication that there is an inflammatory issue that was blocking the growth of hair. Alopecia areata would be the most likely diagnosis in such as case.
If alopecia areata is the final diagnosis, then continued beard injections together with other systemic options would be possible including dexamethasone, methotrexate, cyclosporine, tofacitinib. A return to oral minoxidil could be reconsidered depending on exactly what your story was when you stopped it
Thanks again for submitting your case. I hope this was helpful.