Do patients with immune mediated hair loss who use immunosuppressants need to stop their medications when they get a COVID 19 vaccine?
I’ve selected this question below for this week’s question of the week. It allows us to the review the decisions that go into stopping (or not stopping) medications after getting a COVID vaccine.
QUESTION
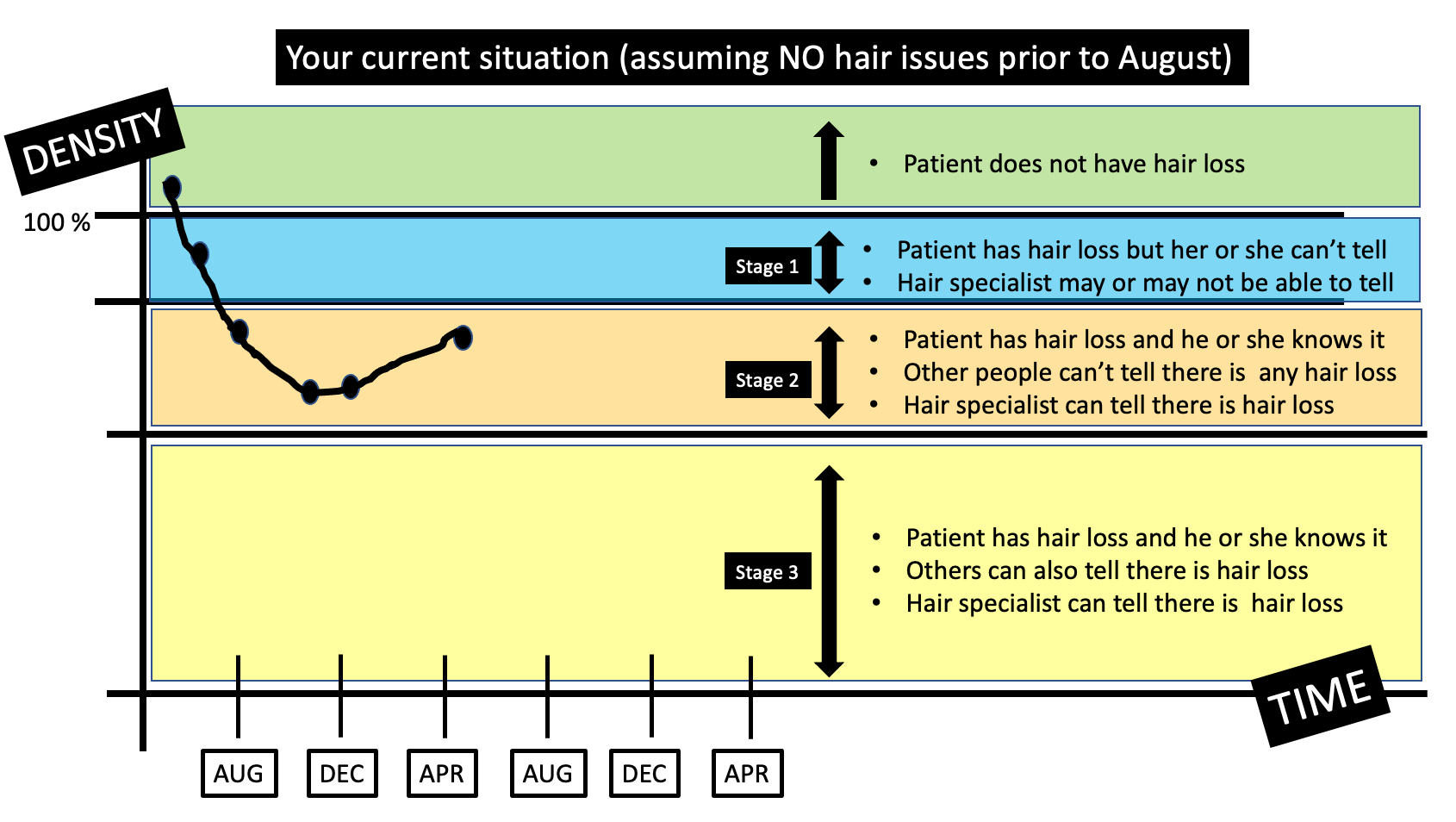
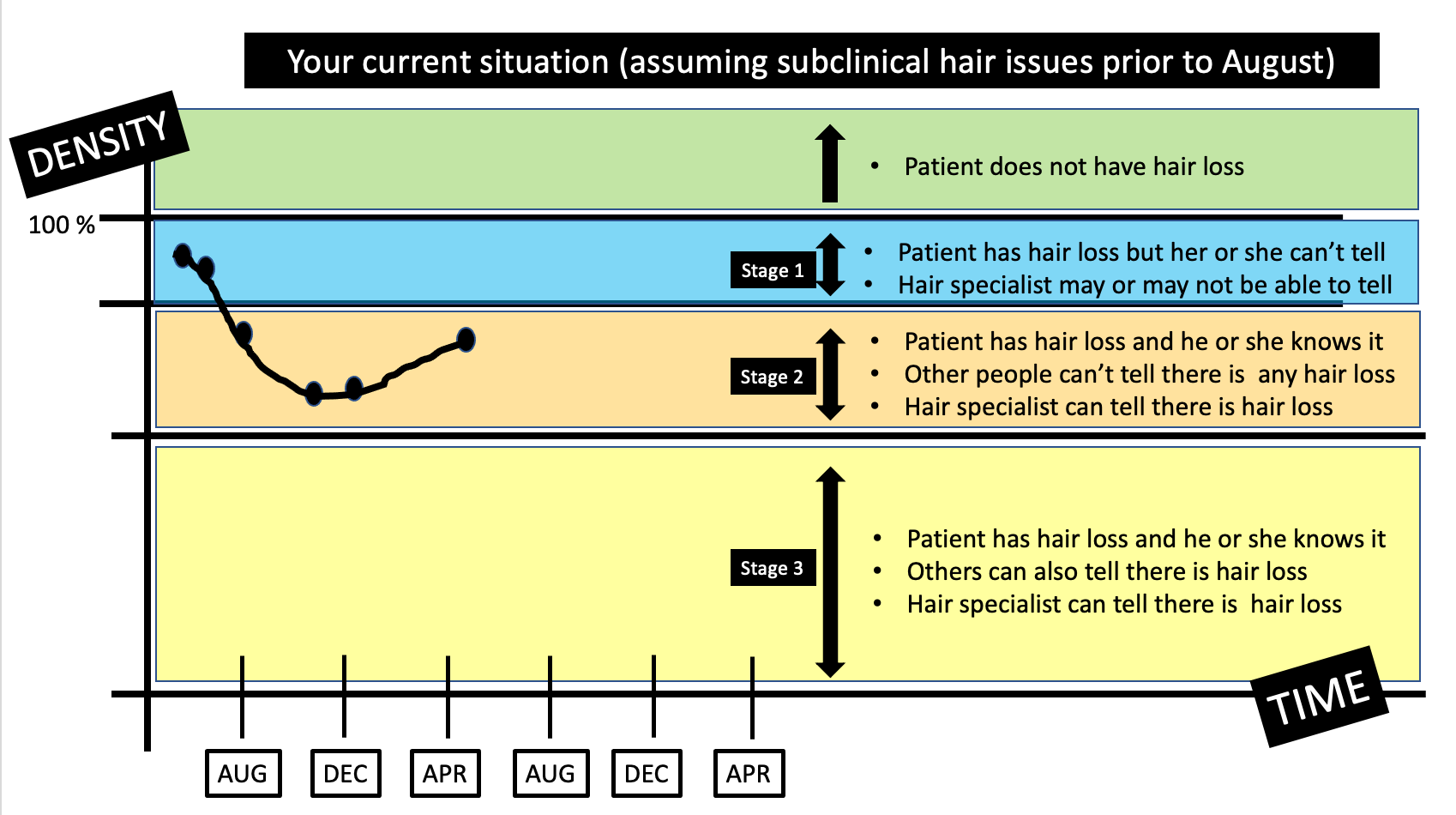
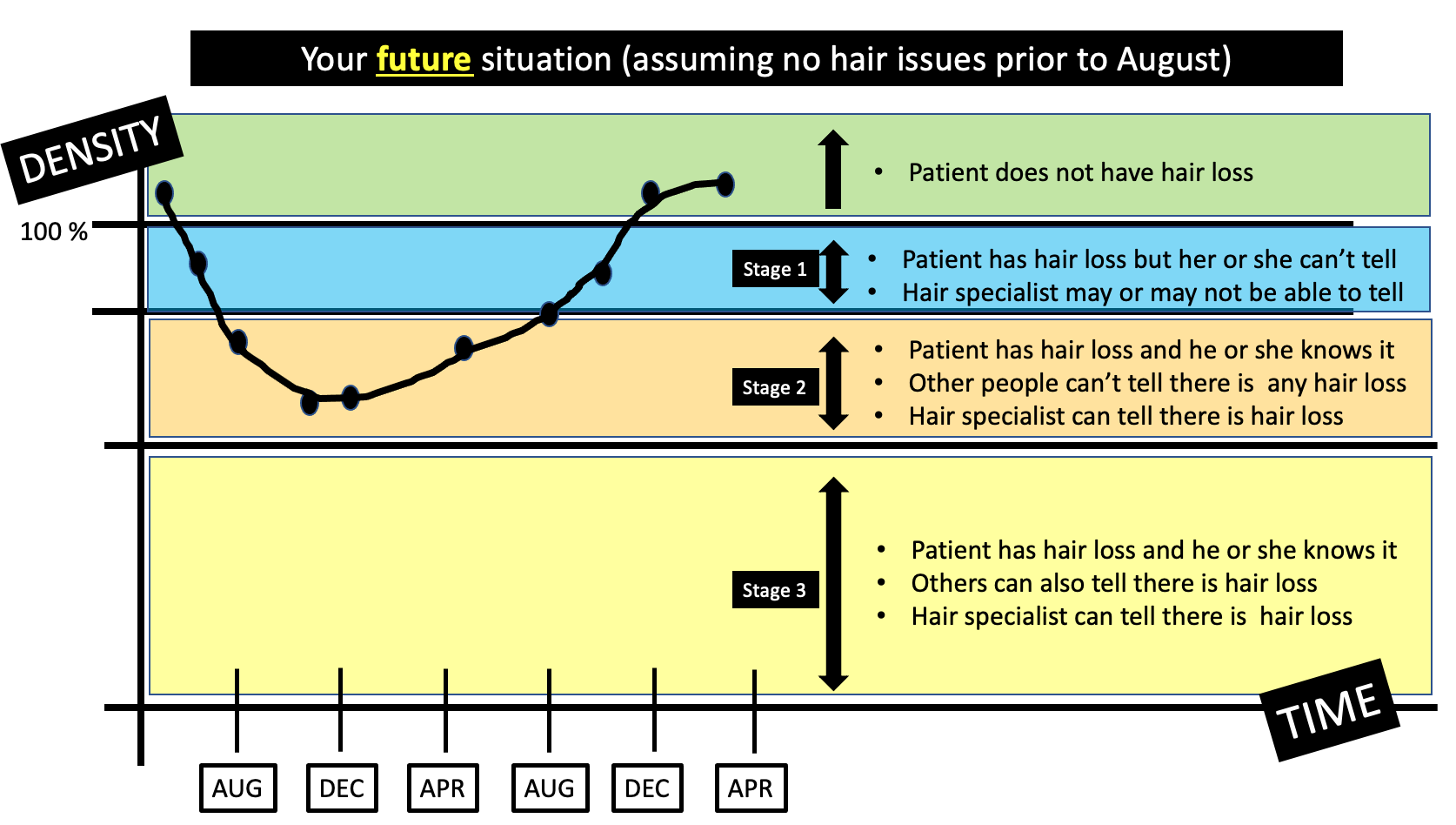
My daughter is 16 years old and was prescribed methotrexate for her alopecia areata. The treatment is working extremely well and she has had full hair for 9 months. She is planning to have her COVID vaccine in a few weeks and we are trying to get a sense as to whether she is supposed to stop her methotrexate or not before she gets her shot. Our various doctors have mixed views on what to do!
What are your recommendations for your patients?
ANSWER
Thanks for the great question. It’s an important one!
Short answer - it’s probably okay to continue !
Let me begin by saying that at present, there are still no clear-cut, definite and universally agreed upon guidelines on what to do for patients with alopecia areata (or other immune based hair loss conditions). We only have guidelines from other medical organizations that then need to be interpreted for hair loss patents.
There is one recommendation, however, that is pretty clear - keep the appointment for the vaccination! That’s a far more important decision for your daughter than the decision to stop the methotrexate or not!
Let’s get into the key part of the question - should your daughter stop methotrexate or not?
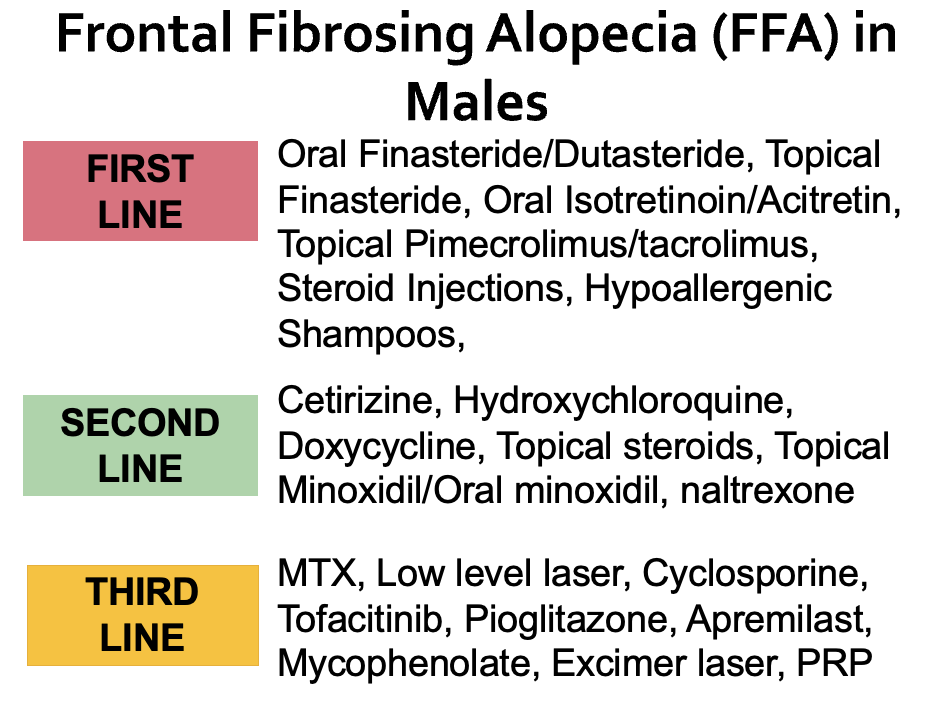
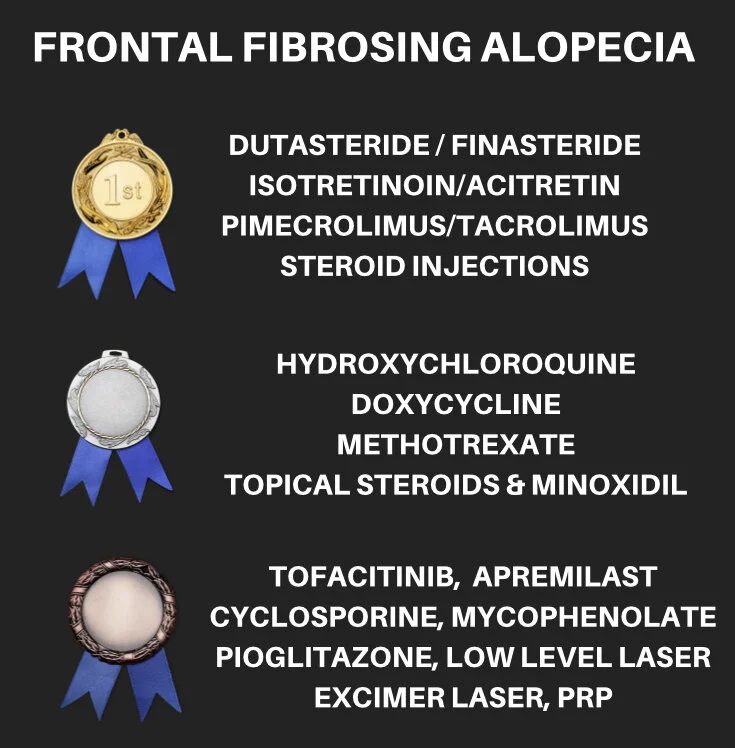
I’d like to point out that there are many different types of immune-mediated hair loss conditions for which immunosuppressive medications are prescribed. These include alopecia areata and patients with various scarring alopecias like lichen planopilaris, frontal fibrosing alopecia, discoid lupus, etc.
Methotrexate, cyclosporine, mycophenolate, TNF inhibitors, hydroxychloroquine, JAK inhibitors, oral steroids are all immunosuppressive medications that may be used by patients with immune-mediated hair loss. I prescribe them every day.
So does being on an immunosuppressive make it any more difficult for a patient to mount a full and normal immune response after getting a vaccination?
For some immunosuppressive medication that answer is a “yes.”
The Famous Park et al Study from South Korea
We know from data in the past that rheumatoid arthritis patients using the drug methotrexate had antibody responses to the influenza vaccine that were “slightly worse” when patients were told to continue their methotrexate compared to when they were told to stop taking the methotrexate for 2 weeks. This well known study has prompted many physicians to consider withholding methotrexate (if possible) before giving the influenza vaccine.
Let’s look at the study in more detail.
The South Korean study by Park and colleagues involved 156 patients with rheumatoid arthritis who continued their methotrexate before getting their influenza vaccine and 160 patents who stopped their methotrexate for 2 weeks AFTER getting their influenza vaccine. 75.5 % of patients who paused their methotrexate had satisfactory vaccine responses compared to 54.5 % of patients who kept taking the methotrexate. In addition, it’s important to take note that there was no change in disease activity between the groups and patients who took paused methotrexate for two weeks did not experience a disease “flare.”
The question then arises as to whether our hair loss patients who use immunosuppressive medications should withhold their treatment before or after getting COVID vaccine. The challenge with answering this question is we don’t have any good data on antibody responses in patients with specific autoimmune “hair loss” conditions. We have some guidelines for how patients on various drugs for rheumatologic disease should proceed with vaccination. In addition, we have some recommendation on how patients with skin diseases like psoriasis should proceed. However, we don’t have any studies or advice to specifically guide hair loss patients.
Being a hair loss doctor, these sorts of answers are important to me!
Should a 16 year old on methotrexate for alopecia areata stop her methotrexate for a period of time after getting a COVID vaccination?
Should a 16 year old on methotrexate and 10 mg prednisone for alopecia areata stop her methotrexate for a period of time after getting a COVID vaccination?
Should a 16 year old on methotrexate and 40 mg prednisone for alopecia areata stop her methotrexate for a period of time after getting a COVID vaccination?
Should a 16 year old on methotrexate for alopecia areata stop her methotrexate for a period of time after getting a COVID vaccination if her hair is thick and full and has been full for a long time?
Should a 16 year old on methotrexate for alopecia areata stop her methotrexate after getting a COVID vaccination for a period of time if her hair only started growing back last month?
Should a 21 year old on tofacitinib for alopecia areata stop her tofacitinib for a period of time after getting a COVID vaccination?
Should a 41 year old female using methotrexate for lichen planopilaris stop her methotrexate for a period of time after getting the COVID vaccine?
Let’s review some key stuff.
Recommendations from the Rheumatology Field
Rheumatologists frequently use immunosuppressive medications for treating autoimmune diseases so we frequently turn to the rheumatology field for guidance on how we might treat autoimmune hair loss. Various rheumatology organizations have put forth broad recommendations to help patients and their doctors. These organizations often recommend stopping some mediations for one week and rarely two weeks. We’ll take a look at some key studies and then we’ll take a look at their formal recommendations. Then, we’ll jump over to recommendations from other fields of medicine (other than rheumatology).
The Giesen and Colleagues Study
A study by Giesen and colleagues examined if patients with chronic inflammatory disease who use immunosuppressive medications mount good antibody responses after COVID vaccination and whether these vaccines flare underling disease. The researchers studied 42 healthy controls and 26 patients with inflammatory disease (including psoriasis, psoriatic arthritis, lupus, rheumatoid arthritis, spondyloarthropathy). Antibody responses at week 1 were good in patients with chronic inflammatory disease who were using immunosuppressives although antibody titers were about 20 % less than controls. The main conclusion of the Giesen study was that patients with various immune mediated diseases still mount pretty good antibody responses and the authors proposed these antibody responses should still be fairly protective. That wasn’t studied in the research study so it’s a bit of a best guess.
The Deepak and Colleagues Study
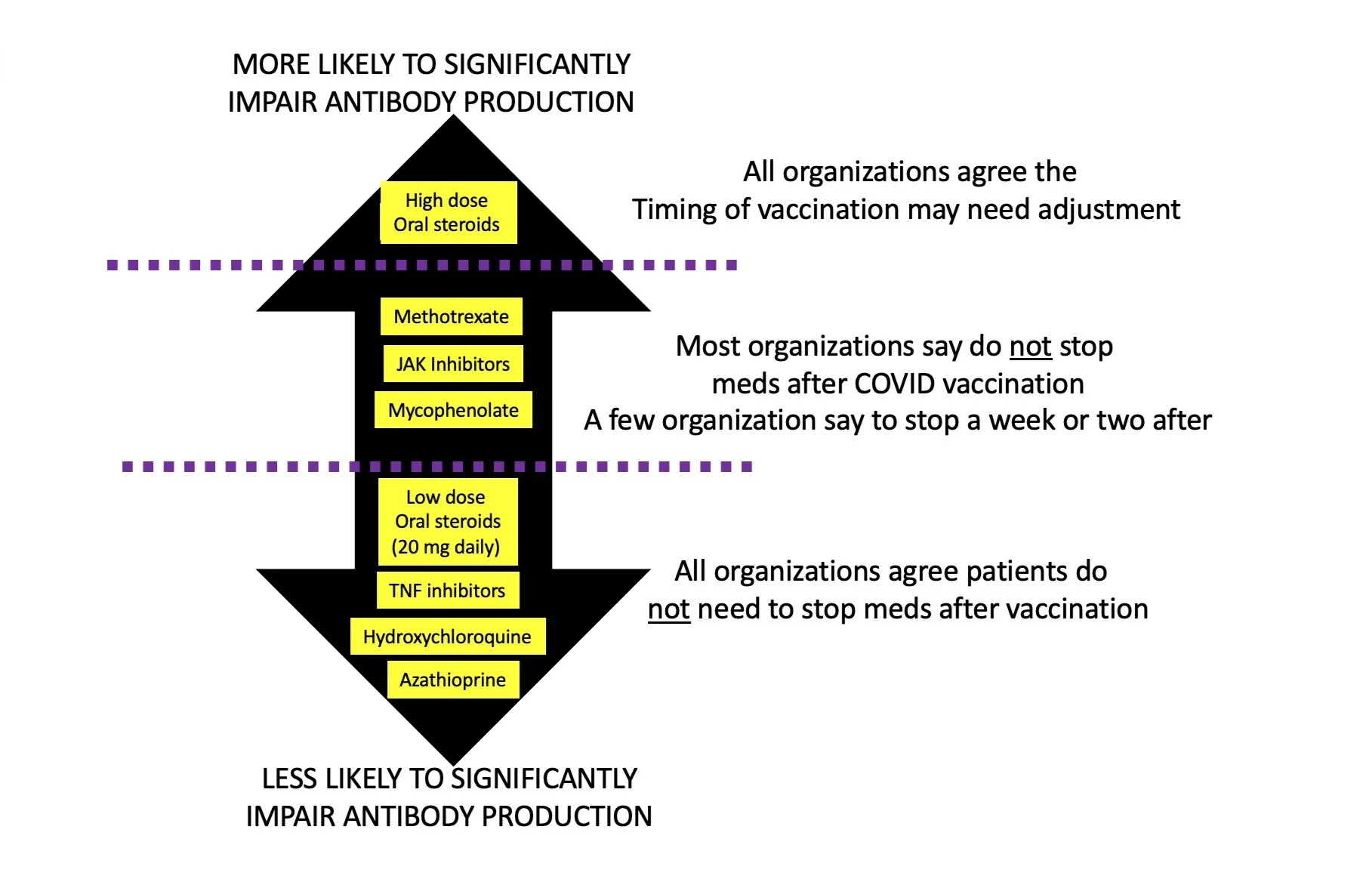
Preliminary data from the Washington University in St. Louis and the University of California, San Francisco suggests that immunosuppressive medications blunt the antibody responses in patients who get the COVID mRNA vaccine. The authors found that oral steroids and B cell depleting agents (i.e. rituximab) are most likely to impair antibody responses but that drugs like tofacitinib and methotrexate can also impair antibody responses - but to a lesser degree. The use of TNF inhibitors had only minimal effects.
To provide more detail, the authors found that compared to immunocompetent controls, there was a three-fold reduction in anti-S IgG antibody titers (P=0.009) and SARS-CoV-2 neutralization (p<0.0001) were observed in immunosuppressed patients. Patients using B cell depleting therapies and corticosteroids had a 36- and 10-fold reduction in humoral (antibody) responses, respectively (p<0.0001). Janus kinase inhibitors and antimetabolites, including methotrexate, also blunted antibody titers (P<0.0001, P=0.0023, respectively). For methotrexate , there was an average a two- to-three-fold reduction in antibodies and neutralization. For JAK inhibitors, it was approximately 4.5 fold reduction. Other targeted therapies, such as TNF inhibitors, IL-12/23 inhibitors, and integrin inhibitors, had only modest impacts on antibody formation and neutralization.
The American College of Rheumatology recommends STOPPING some (but not all) immunosuppressive medications for 1 week after vaccination in order to help improve the effectiveness of the vaccine. This is mainly for those with well-controlled disease who have low chances of flaring when the drug is stopped.
a) Mycophenolate - skip for 1 week after each vaccine dose
b) JAK inhibitors - skip for 1 week after each vaccine dose
c) Methotrexate - skip for 1 week after Pfizer or Moderna (skip 2 weeks after J&J)
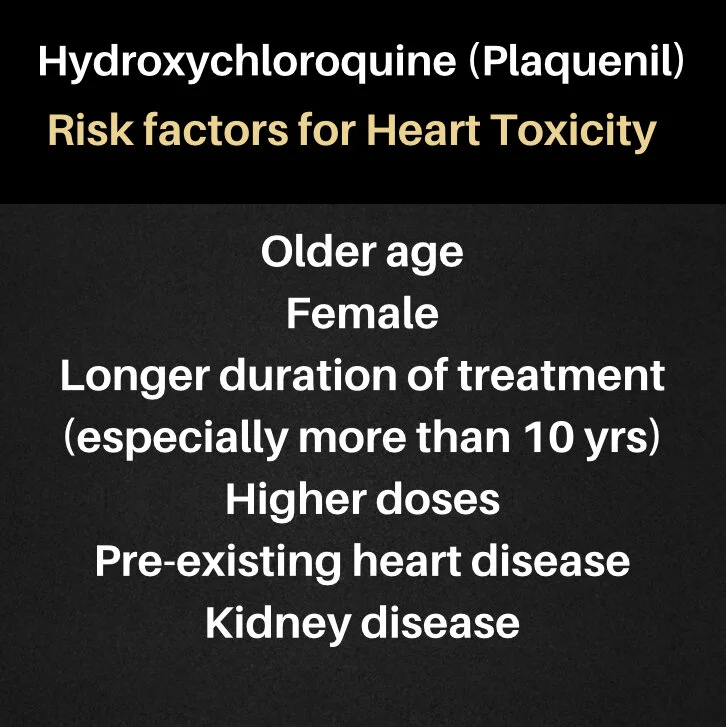
d) Hydroxychloroquine (Plaquenil) - no need to stop the drug
The ACR also recommends that patients have the exact same vaccine the second time if they are having an mRNA vaccine. In other words, if a patient gets the Pfizer vaccine for his or her first dose, they should get the Pfizer vaccine for his or her second dose. The ACR does not recommend switching up vaccines depending on availability.
The Canadian Rheumatology Association has published helpful guidance. Their recommendations are different than the American College of Rheumatology. The Canadian group recommends that only two drugs should really change how vaccines are given. Those are high dose prednisone (more than 20 mg per day) and rituximab (which is not used in treating hair loss). Other drugs can be continued including
a) TNF inhibitors - no need to stop after getting the vaccine
b) Azathioprine - no need to stop after getting the vaccine
c) Cyclosporine - no need to stop after getting the vaccine
d) Hydroxychloroquine - no need to stop after getting the vaccine
e) Methotrexate - no need to stop after getting the vaccine
f) Prednisone (20 mg or less) - no need to stop after getting the vaccine
The European Alliance of Associations for Rheumatology (EULAR) advises that most drugs can be continued in those undergoing vaccination. The only exception is the drug rituximab (which is different than Ruxolitinib so readers should not confuse the two!)
The Korean College of Rheumatology has recommended withholding MTX for 1-2 weeks and to consider withholding tofacitinib and JAK inhibitors one week (but recognize that data for JAK inhibitors is less clear than for methotrexate).
The British Society of Rheumatology has recommended that everyone get vaccinated “regardless of treatment regimen or underlying diagnosis”
Other researchers have put for recommendations to stop methotrexate up to 2 weeks after vaccination.
Recommendations from the Psoriasis Field
The National Psoriasis Foundation (NPF) does NOT recommend that patents with psoriasis stop most medications before getting the vaccine. The only exception is the Ad26.COV2.S (Johnson & Johnson or “J&J” vaccine in which case the NPF recommends possibly stopping the J&J vaccine for 2 weeks if the patient is older than 60, has at least one risk factor for poor COVID outcomes, and his or her psoriasis is stable and his or her doctor agree with this plan.
This seems to be the only exception in the psoriasis field. It’s important to point out that we don’t actually know if stopping makes any difference to improve vaccine responses. But this has been the take on the NPF’s recommendations.
Summary of Study Results to Date in the World Regarding Vaccines, COVID Vaccines and Immunosuppressive Medications
The following is a helpful summary of the main key findings of data so far:
Current vaccines reduce the chance of developing COVID 19.
Current vaccines reduce the chances of developing severe disease even if one does get COVID 19.
Some protection against COVID 19 in better than no protection.
We still have no clear cut idea about what antibody level after vaccination signals that a person is protected. Fortunately, most people do have pretty good protection after vaccination (but not all).
If at all possible, vaccinate patients when their immune disease is quiet.
Younger patients have better vaccine responses than older patients.
Some immunosuppressive drugs reduce the amount of antibodies that are formed to the Sars-COV-2 virus. Rituximab (which we don’t typically use in any hair loss condition) impairs antibody responses the most - and second highest are the oral steroids. In one study, JAK inhibitors like tofacitinib impair antibody responses 4.5 times and Methotrexate reduces responses by 2-3 fold. There is no good studies yet to suggest these antibody reductions mean the patient is more likely to get COVID19 disease.
Organ transplant patients on various immunosuppressant medications don’t mount very good antibody responses to the COVID vaccine. A study from John Hopkins found that only 15 % of patients had good antibody responses after 1 dose and just over one half had good responses after two doses.
Doses of prednisone of less than 10 mg daily seem to be associated with good antibody responses. Ideally, patients should not be vaccinated if possible until the doses of prednisone fall below 20 mg.
Sulfasalazine, hydroxychloroquine, azathioprine and leflunomide may reduce vaccine antibody titers but have not been shown to inhibit a seroprotective response to the pneumococcal or influenza vaccines. Most of the main world medical organizations suggest these drugs NOT be stopped when patients go for their vaccine.
TNF inhibitors probably don’t affect the vaccine response all that much. Most of the main world organizations suggest these drugs not be stopped when patients go for their vaccine.
In organ transplant patients, mycophenolate was shown to reduce antibody titers after vaccination but not below the threshold for protection. In one study of mycophenolate users, only 27 % of 11 patients using mycophenolate had good antibody responses. Some organizations like the American College of Rheumatology (ACR) suggest stopping 1 week. Other organizations do not.
JAK inhibitors impair vaccine response slightly after various types of immunizations. It’s not clear if this really reduces antibody responses below a protective level after COVID 19 vaccinations or not. Holding it one week could make sense in a stable well controlled patient. This is the view of the American College of Rheumatology and the view of the Korean College of Rheumatology